Tarsometatarsal Arthrodesis
Shine John
Alan R. Catanzariti
Robert W. Mendicino
The tarsometatarsal (TMT) joint, also known as Lisfranc joint, describes articulations of the metatarsals with their respective cuneiforms and cuboid. The major function of the TMT joint complex is the regulation and redirecting of loading forces during weight-bearing (1). During normal gait biomechanics, this joint generally undergoes limited motion. Primary arthritis of this joint is rare, but not uncommon. Trauma-related incidents, whether by lack of recognition, misdiagnosis, malreduction, or inadequate stabilization, can elicit adverse motion in this joint that can result in significant posttraumatic arthritis, pain, deformity, and disability. The typical symptom complex may include local pain confined to the TMT joint or pain secondary to lateral impingement syndrome when associated with adult-acquired flatfoot (2). Arthrodesis is indicated when nonoperative treatment is ineffective. Goals of arthrodesis include improvement of symptoms, deformity correction, realignment of the foot, and functional preservation. Discussion of TMT arthrodesis will be exclusive of neuroarthropathic deformity correction.
ANATOMY AND BIOMECHANICS
The TMT joint is comprised of five metatarsals, three cuneiforms, and cuboid. In general, these skeletal components and their respective morphologies, in concert with a vast arrangement of ligamentous attachments (dorsal, interosseous, and plantar), form a complex polyarticular system (3). The plantar and dorsal ligaments are oriented in three different directions: longitudinal, oblique, and transverse (4). The plantar and interosseous ligamentous attachments receive supportive reinforcement by the plantar fascia, intrinsic muscles, and extrinsic tendons. Except for metatarsals one and two, intermetatarsal ligaments connect metatarsals two through five. Lisfranc ligament, considered the main ligamentous stabilizer of the entire joint, originates from the lateral surface of the medial cuneiform and courses in an oblique manner to the medial aspect of the second metatarsal (5). This ligament is the largest and strongest of the interosseous ligaments (3,6). Recognizing that there is no intermetatarsal ligament between the first and second metatarsals illustrates the importance of the Lisfranc ligament in the maintenance of the anatomic relationship between the medial and middle columns (7). The second metatarsal is most secure in the complex as it sits within a five-bone mortise configuration and is the key for TMT joint stability.
Traditionally, the TMT joint complex has been subdivided into three separate columns: medial, middle, and lateral. The medial column involves the articulation of the first metatarsal with the medial cuneiform. The middle column involves the articulations of the second and third metatarsals with the middle and lateral cuneiforms, respectively. The lateral column includes the fourth and fifth metatarsal articulation with the cuboid. These three columns are integrated in both the longitudinal and transverse arches of the foot that provide the osseous stability of the TMT joint (4).
Respective to other tarsal joints, the TMT joints individually undergo limited motion. Ouzounian and Shereff (8) noted that motion occurring at the individual columns of the joint includes limited dorsiflexion, plantarflexion, supination, and pronation. As a functional unit, the TMT movements are that of pronation and supination of the forefoot (9,10). The second metatarsal-middle cuneiform articulation exhibits the least motion in both planes. The fourth and fifth metatarsal-cuboid articulation (lateral column) exhibits the most motion of the entire complex.
ETIOLOGY
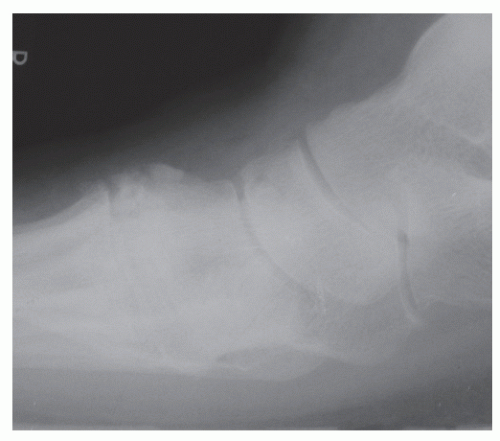
History of a TMT joint injury significantly predisposes the patient to painful arthritis at this area (Fig. 56.1). These injuries are associated with motor vehicle accidents and falls, as well as crush and twisting injuries of the foot (11). These may be caused by both direct and indirect forces. Extent and management of the traumatic injury, as well as duration since the injury, likely plays a role into the severity of posttraumatic arthritis and prognosis. These may also play a role into the onset of painful arthritis.
Subtle, unrecognized injuries may precipitate pain and progressive deformity quicker as there is sustained instability during axial load. Lack of recognition is plausible as subtle fracture-dislocation injuries may at times spontaneously reduce and can be misdiagnosed as foot sprains. The extent of articular damage may not be appreciated until the patient develops painful arthritis. More overt, traumatic, higher energy injuries usually lead to significant soft tissue, articular, and vascular damage that is often difficult to manage. Comparatively, nonoperative treatment for these injuries has yielded less favorable results than that of open surgical management (9,12,13 and 14).
Initial management for any type of TMT joint injury should seek to achieve stable anatomic reduction. Degenerative changes are precipitated by inadequately reduced/stabilized TMT joint injuries. Interestingly, regardless of the adequacy of initial management, a high prevalence of posttraumatic osteoarthritis after TMT fractures and dislocations has been reported (10,11,14).
TMT joint complex arthrosis is most often associated with significant deformity. However, primary degenerative arthritis can be noted with little to no associated deformity in some patients, particularly in patients with a rigid pes cavus foot. Compression arthropathy is the likely causative factor leading to arthrosis of TMT joint complex. Systemic arthritides can also be a causative factor of painful, degenerative changes at this joint complex.
EVALUATION/ASSESSMENT (CLINICAL AND RADIOGRAPHIC)
A comprehensive history and physical should be attained with these patients. The surgeon should determine whether any injuries, minor or major, have been incurred by the patient prior to their presentation. Appreciation for the extent of initial injury and attempted management can facilitate comprehension of the predisposing factors for pathologic changes at the TMT joint.
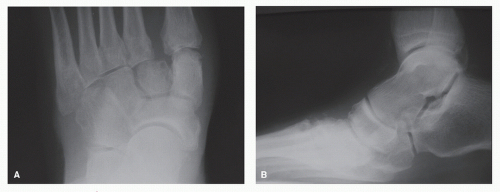
Typical symptoms include chronic, deep aching pain confined to the TMT joint or pain secondary to lateral impingement syndrome when associated with an adult-acquired flatfoot deformity. Patients with a history of higher energy injuries may present with a more intricate and global symptom complex than those typically related to degenerative arthritis. Significant skin and soft tissue damage likely may have resulted at the time of injury and may have been exacerbated with attempted surgical stabilization. Symptoms can include those consistent with neuritis, neuromas, and metatarsalgia. Prominent dorsal osteophytic changes may impinge and irritate the deep or superficial peroneal nerve (Fig. 56.2). Patients may also describe positional changes, footwear problems, and gait disturbances. Symptoms consistent with complex regional pain syndrome (CRPS) should be noted. The authors have seen a relatively large number of patients with TMT injuries develop CRPS. CRPS has obvious implications when considering surgery.
The patient should be examined off weight-bearing as well as in static stance. The patient should be asked to identify areas of maximum tenderness during manual exam on the exam table and while weight-bearing. Some patients present with a focus of pain located at one or more of the individual TMT joints, while others complain of pain at adjacent areas as well. Differentiation must then be established between referred pain and neighboring joint degeneration. A passive pronation and abduction test has been described to localize pain within the TMT joint (15). Gentle, passive pronation and abduction of the forefoot with the hindfoot stabilized resulted in increased midfoot pain. Each individual TMT joint should be carefully palpated and manually manipulated in the sagittal and transverse plane to delineate the involved areas of pain. Some authors have described the use of manipulation under fluoroscopy to determine which joints are involved in the instability pattern (16). The hindfoot is stabilized while the forefoot is manipulated, first with an abduction-adduction force and then
with plantar flexion and dorsiflexion stresses. Posttraumatic or primary arthritis at the TMT joint invariably involves the middle column (second and third metatarsal-cuneiform joints). The medial column (first metatarsocuneiform joint) is usually involved, whereas the lateral column (fourth and fifth metatarsocuboid joints) is rarely involved.
with plantar flexion and dorsiflexion stresses. Posttraumatic or primary arthritis at the TMT joint invariably involves the middle column (second and third metatarsal-cuneiform joints). The medial column (first metatarsocuneiform joint) is usually involved, whereas the lateral column (fourth and fifth metatarsocuboid joints) is rarely involved.
Those patients that have suffered misdiagnosed or untreated injuries, with progressive deformity, can demonstrate sagittal and transverse plane deformity (Fig. 56.3). Weight-bearing and gait exams of both extremities may resemble an adult-acquired flatfoot deformity with unilateral abduction and dorsiflexion noted at the TMT in relation to the rearfoot, decreased longitudinal arch height, and a plantar medial eminence (Fig. 56.4). Physical examination may reveal callosities secondary to uneven forefoot loading and altered shoe wear may be evidenced. Function of the posterior tibial tendon should be tested in these patients. Assessment for posterior muscle group contracture should also be performed as equinus contracture may develop and worsen with progressing deformity. Skin quality and vascular competence may be compromised if prior surgical stabilization was performed and/or significant crush injury was incurred at the time of injury. The dorsal skin quality should be assessed for incisional placement planning. The authors routinely utilize noninvasive vascular studies of both lower extremities to quantitatively assess vascular sufficiency. These include pulse volume recordings, ankle and digital-brachial
indices, and transcutaneous oximetry. Advanced vascular imaging and intervention are sought based on necessity.
indices, and transcutaneous oximetry. Advanced vascular imaging and intervention are sought based on necessity.
Weight-bearing anteroposterior (AP), oblique, and lateral radiographs of the foot should be obtained in the angle and base of gait. An assessment of degenerative changes and underlying deformity should be performed. Angular measurements can be useful in evaluation of structural deformity. The talar-first metatarsal angle in the AP and lateral projection can be used to appreciate the degree of forefoot abduction and dorsiflexion, respectively, relative to the hindfoot. Respective congruity of the dorsal and plantar aspects of each metatarsal to its corresponding cuneiform or cuboid on an AP and lateral projection can elicit points of instability and misalignment within the joint complex (17). Oblique views are useful for comparing orientation and position of the middle and lateral TMT columns. Radiographs of the contralateral, unaffected foot should be compared to the affected foot.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree