HISTORICAL REVIEW
Tarsal coalitions have been identified and recorded for several hundred years or more. Heiple and Lovejoy (
1) reported a tarsal coalition in the foot of a pre-Columbian Indian skeleton
circa 1000 ad. Coe and Broman (
2) found an even older specimen in the ruins of a Mayan temple in Guatemala. More recently, in 2005, Silva (
3) reported two cases of nonosseous calcaneonavicular coalition in older specimens from Portuguese burial sites dating back to between the late Neolithic period and the early Bronze age (i.e., between 3600 and 2000 BC).
Historically, the first written description of tarsal coalition is attributed to Buffon (
4) in 1769. Jones (
5) provided the first detailed clinical recounting of peroneal spastic flatfoot in 1897, but he did not associate it with tarsal coalition. The first radiographic demonstration of tarsal coalition was by Kirmisson (
6) in 1898, only 3 years after Roentgen’s discovery of x-rays.
Many years passed between the earliest anatomic descriptions and the discovery of x-rays, and many more years elapsed before the identification of the relationship between tarsal coalition and peroneal spastic flatfoot. In this sense, the two most common tarsal coalitions—calcaneonavicular and talocalcaneal—were identified in similar fashion. First they were identified anatomically, then radiographically, and, more recently, they were related to peroneal spastic flatfoot.
Calcaneonavicular coalition was first described anatomically by Cruveilhier (
7) in 1829. Slomann (
8), in 1921, reported five cases of calcaneonavicular bar and demonstrated the coalition on an oblique radiographic view of the foot. Not until 1927, however, when Badgley (
9) resected a calcaneonavicular coalition, was the deformity associated with peroneal spastic flatfoot.
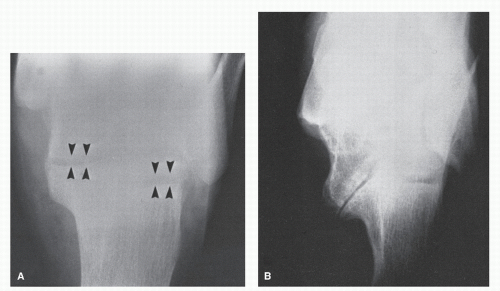
Similarly, Zuckerkandl (
10) first anatomically identified
talocalcaneal coalition in 1877. Korvin (
11), in 1934, used an axial radiographic view of the calcaneus to demonstrate a talocalcaneal coalition. In 1948, Harris and Beath (
12) popularized Korvin’s axial or ski-jump view of the calcaneus and recognized talocalcaneal coalition as a cause of peroneal spastic flatfoot.
Other tarsal coalitions are less frequent but have been reported.
Talonavicular coalition was first reported by Anderson (
13) in 1879.
Calcaneocuboid coalition was first recognized by Holland (
14) in 1918.
Cubonavicular coalition was first reported by Waugh (
15) in 1957, and Lusby (
16) first identified
naviculocuneiform coalition in 1959. Multiple and massive coalitions involving several tarsal bones also have been reported (
17,
18).
Before the advent of radiography, earlier clinicians had to rely on clinical examination alone to diagnose a tarsal coalition. Today, with advanced radiographic and diagnostic imaging techniques, the demonstration and diagnosis of tarsal coalition are simplified. However, although much has been written about tarsal coalition and much is understood, several diagnostic and therapeutic questions remain unanswered.
ETIOLOGY
Tarsal coalition is clearly the most common cause of peroneal spastic flatfoot. However, the cause of tarsal coalition is not so clear. Many authors have attempted to attribute all tarsal coalitions to one etiologic factor. It is now certain that the condition has many causes, and tarsal coalitions may be either congenital or acquired.
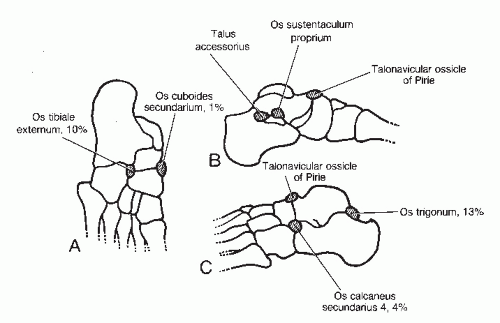
Congenital coalition is more frequently identified and reported, although the mechanism of congenital coalition is not conclusively known. Pfitzner (
19) suggested that a congenital tarsal coalition is formed from the incorporation of accessory ossicles into the normal tarsal bones on either side of a joint or in close approximation with one another. Many authors have supported this theory, and the primary evidence has been that the os sustentaculum proprium accessory bone occurs at the side of the middle facet of the subtalar joint in which many coalitions occur. In addition, other investigators have described a tarsal coalition occurring in the area of the os trigonum accessory bone (
20,
21 and
22). This evidence strongly suggests that any accessory bone may fuse to one or more tarsal bones and may result in a tarsal coalition (
Fig. 45.1). Although this has been shown to be one possible cause of coalition, Harris (
23) disproved it as the sole cause by demonstrating a tarsal coalition in a fetus. The appearance of a tarsal coalition in a fetus, in which development and incorporation of accessory ossicles would not have had time to occur, certainly works against Pfitzner’s theory.
Harris’s finding supports the theory proposed by Leboucq (
24), who suggested that congenital coalition results from the failure of differentiation and segmentation of primitive mesenchyme. This concept, which is the most commonly accepted theory today, attributes congenital coalitions to a heritable defect or to an insult in the first trimester of pregnancy. Subsequently, numerous authors have reported hereditary patterns of coalitions (
17,
25,
26,
27,
28,
29,
30,
31,
32 and
33). Most evidence supports a gene mutation for coalition formation, which is then passed on to future generations as an autosomal dominant gene.
A large field study by Leonard (
34) provided the most evidence in support of Leboucq’s theory. Leonard concluded that tarsal coalition was a unifactorial disorder with autosomal dominant inheritance. Kawashima and Uhthoff (
35) examined 20 cartilaginous talocalcaneal bridges in 16 embryos and fetuses ranging from 7 to 20 weeks and concluded that coalition was caused by a failure or delay in differentiation of mesenchymal
tissue between the posterior portion of the sustentaculum tali and the corresponding area of the talus during the 7.5 to 8.5 postovulatory weeks. More recently, histopathologic evidence has been found to support Leboucq’s theory further (
36). Thus, the generally accepted theory is that congenital coalition is caused by a genetic mutation to an autosomal gene that results in the failure of differentiation and segmentation of primitive mesenchyme.
Tarsal coalition may also be acquired.
Acquired tarsal coalition may result from arthritis, infection, trauma, neoplasms, or other conditions (
37). Acquired coalition is less common in pediatric and adolescent patients (
38). The acquired coalition typically starts as a diminished range of motion within the involved joints, with varying progression to complete fusion (
39). A talonavicular coalition in a 24-year-old patient has been described secondary to osteoarthritis, which resulted from a previous tuberculosis septic arthritis of the tarsus when the patient was 11 years of age (
40). A case of restricted subtalar joint motion and peroneal spastic flatfoot that occurred secondary to a fibrosarcoma has also been noted (
41). Healey and Willkens (
42) reported two patients with juvenile rheumatoid arthritis with resultant tarsal arthritis and eventual tarsal coalition. In a retrospective review of 88 patients with juvenile rheumatoid arthritis and 97 patients with classic or adult rheumatoid arthritis, 16% of the patients with juvenile rheumatoid arthritis and 10% of the patients with adult rheumatoid arthritis had intertarsal ankylosis (
43). Roth (
44) reported a case of massive tarsal ankylosis in a patient with juvenile ankylosing spondylitis. Talonavicular coalition has also been reported after Köhler disease (i.e., avascular necrosis of the navicular) (
45). In addition, subtalar joint limitus and eventual coalition are known to result from a joint-depression calcaneal fracture (
46). Thus, when all age groups are considered, it is clear from these examples that acquired coalition is common and is a frequent cause of peroneal spastic flatfoot.
INCIDENCE
The incidence of tarsal coalition in the general population is not known. Rankin and Baker (
47) reported a 0.04% incidence (24 cases in 60,000 young adults) in a large population of military personnel. Shands and Wentz (
48) reported an incidence of 0.9% (11 cases in 1,232 children) in a population of children in a clinic. Vaughan and Segal (
49), studying army personnel, found the incidence to be approximately 1.4% (28 cases in 2,000 patients). This is the highest reported incidence to date. However, one may argue that these studies were not conducted on representative populations in regard to age or sex. Thus, the actual incidence in the general population may be higher or lower.
Nonetheless, the incidence of tarsal coalition is not the same as the incidence of peroneal spastic flatfoot. Peroneal spastic flatfoot is usually a sequela of the tarsal coalition. A tarsal coalition may be present without symptoms or without peroneal spastic flatfoot. In addition, peroneal spastic flatfoot may be present without tarsal coalition. Harris and Beath (
12) examined 3,619 Canadian army enlistees and found an approximately 2% incidence of peroneal spastic flatfoot, with a correspondingly lower incidence of tarsal coalition of 0.03%.
Tarsal coalition has been reported to have no racial preference (
47). Further, roughly 50% of the cases have been reported as bilateral (
47), although Leonard (
34) reported that the incidence of bilateral involvement was as high as 80%.
Several authors have suggested a greater incidence of tarsal coalition in male patients, with male-to-female ratios reported in two different studies as 12:5 (
50) and 4:1 (
51). Investigators have theorized that this unequal sex predilection may reflect that the studies were performed on army personnel (
52). Indeed, if these studies are correct in their suggested predilection, the theory of mutation of an autosomal dominant gene must be reconsidered. Leonard (
34) reported a more equal sex incidence in his large study. Thus, the actual sex predilection remains unclear.
Talocalcaneal coalition and calcaneonavicular coalition are by far the most common anatomic types of this condition. These two forms account for approximately 90% of all tarsal coalitions (
53). However, controversy exists about which of these two coalitions is most prevalent. Leonard (
34) reported an extremely skewed study in which 27 of 31 patients with coalitions had calcaneonavicular involvement. Conversely, Harris (
54) reported 66 talocalcaneal coalitions and 29 calcaneonavicular coalitions among the total of 102 coalitions found. Other studies have demonstrated a more even distribution (
47,
55,
56,
57,
58 and
59). Stormont
and Peterson (
59), after reviewing the literature, tabulated the relative incidence of talocalcaneal and calcaneonavicular coalitions reported in all articles they found that included cases of more than one type of coalition. The calculated relative incidence was 48.1% for talocalcaneal coalitions, 43.6% for calcaneonavicular coalitions, and 8.3% for other coalitions. Thus, the current consensus is that talocalcaneal and calcaneonavicular coalitions account for about 90% of all coalitions, and talocalcaneal coalition is slightly more common.
Talonavicular coalition appears to be the third most common type of tarsal coalition. This type is rare, with fewer than 50 cases reported in the literature (
13,
25,
31,
47,
51,
54,
55,
58,
60,
61,
62,
63,
64,
65,
66,
67,
68,
69,
70,
71,
72,
73 and
74). Calcaneocuboid (
14,
54,
58,
75,
76,
77,
78 and
79), cubonavicular (
15,
47,
80,
81,
82,
83,
84 and
85), naviculocuneiform (
16,
86,
87,
88,
89,
90,
91,
92,
93,
94,
95 and
96), metatarsocuneiform (
97,
98 and
99), combination tarsal coalitions, and massive coalitions occur with even less frequency (
52,
95).
ASSOCIATED ABNORMALITIES
The association of tarsal coalition with other skeletal abnormalities and syndromes is well documented. Once a tarsal coalition has been identified, one should query and examine the patient to rule out the presence of these coincidental deformities.
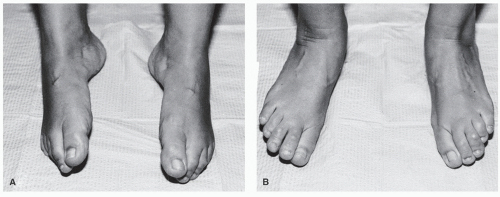
Symphalangism, or ankylosis of the interphalangeal joints, has been shown to be associated with tarsal coalition (
Fig. 45.2). In 1917, Drinkwater (
100) described proximal interphalangeal joint anarthrosis transmitted through 14 generations but did not associate tarsal coalition with the digital deformity. Later, Austin (
101) reported a case of bilateral symphalangism of the distal interphalangeal joints of the third, fourth, and fifth toes associated with bilateral talocalcaneal and calcaneocuboid coalitions. Symphalangism associated with fusion of the second through fifth metatarsals with the cuneiforms and cuboid has been noted in one family (
33). Two families with symphalangism of the hands and concomitant talonavicular coalitions have also been described (
64). Investigators suggested that the two deformities were determined by a single gene, because in both kindreds the inheritance followed an autosomal dominant pattern. Harle and Stevenson (
102) also believed that a coupling effect of genes was responsible for the two conditions, along with metatarsal and midtarsal fusions. Gaal et al (
103) described three distinct ethnic pedigrees that they believed confirmed that symphalangism was an autosomal dominant genetic trait. Castle et al (
104) reviewed four generations of a family with 15 family members exhibiting symphalangism with associated tarsal synostosis and hypophalangism. Typically, symphalangism is not identifiable at birth, because the involved phalanges have not ossified. With growth, however, the affected bones show a faster rate of epiphyseal closure than the nonaffected bones. After epiphyseal closure, the joint space narrows until complete bony fusion occurs.
Tarsal coalitions have also been associated with
metatarsal abnormalities and massive coalitions. Bersani and Samilson (
17) reported a mother and two children who had bilateral massive coalitions involving the talus; navicular; cuboid; second and third cuneiforms; and second, third, and fourth metatarsals. A case of lesser tarsal ankylosis involving the cuneiforms and cuboid and a synostosis between the bases of the fourth and fifth metatarsal bones has also been reported (
105). Illievitz (
66) reported a unilateral case in a boy with four toes, four metatarsals, and coalition of the talonavicular joint.
In addition,
tarsal and carpal coalitions may coexist. O’Rahilly (
106) claimed that fusions of almost every possible combination in the carpal and metacarpal region and in the corresponding portion of the foot have been found. However, despite the developmental similarity of the carpus and tarsus, coalitions in the two areas seem to be unrelated (
40,
67).
Less commonly, tarsal coalitions have been reported with other
major limb anomalies. Tarsal and carpal coalitions have been noted in cases of phocomelia (
106) (i.e., defective development of the arms or legs so the hands or feet are attached close to the body), and tarsal coalitions have been noted in patients with fibular and tibial hemimelia (i.e., absence of a portion of a limb) (
106,
107,
108,
109 and
110). Lamb (
111) reported the association of a ball-and-socket ankle joint with tarsal coalition, but whether the ankle change is an isolated congenital anomaly or is secondary to compensation for the tarsal coalition itself is debatable (
112).
Further, multiple or massive tarsal coalitions may be part of a more complex syndrome. In 1944, Nievergelt (
113) described a syndrome occurring in both sexes in three successive generations of a family. The syndrome consisted of elbow dysplasia with radioulnar synostosis and subluxation of the radial head, dysplasia of the tibia and fibula with the fibula remaining longer because of lesser involvement, and tarsal synostosis associated with atypical clubfoot. Twenty years later, Pearlman et al (
114) reported a similar combination of deformities in a mother and daughter. Their patients did not have dysplasia of the tibia, but they did have concomitant carpal synostosis, symphalangism, and associated brachydactylia (i.e., short fingers) and clinoamptodactylia (i.e., flexion and angulation of the fingers). These investigators termed the combined deformity
Nievergelt syndrome. Later, Dubois (
115) reported an additional case and suggested that
Nievergelt-Pearlman syndrome would be a more appropriate name. In 1975, Murakami (
116) reported three additional cases in a family with impairment of hearing resulting from bony fusion of the ossicles in the middle ear. In 1978, Nixon (
117) reviewed Nievergelt-Pearlman syndrome and believed it would be better termed
multiple synostoses syndrome. He concluded that this syndrome appeared to be inherited in an autosomal dominant fashion and was probably caused by a single gene abnormality.
Similarly, in
Apert syndrome patients may have massive synostosis of the tarsal bones. Tachdjian (
118) described an example of the resulting condition with craniosynostosis, midfacial hypoplasia, osseous or cutaneous syndactyly of all digits (or commonly of the second, third, and fourth fingers and toes), and a broad distal thumb and hallux. Collins et al (
119) used computed tomography (CT) to define the dysmorphology of the foot in three patients with Apert syndrome. These investigators found five consistent findings among the three pairs of feet: (a) anomalous great toes with phalangeal and metatarsal pathologic features, (b) syndactyly of toes 2 to 5, (c) fusions between metatarsals, (d) tarsal coalitions, and (e) limitations in shoes.
Osebold-Remondini syndrome is yet another skeletal dysplasia, first described in 1985 (
120). Mesomelic shortness of limbs and associated shortness of stature, absence of hypoplasia of the middle phalanges with synostosis of the remaining phalanges, and carpal and tarsal coalitions are the typical anomalies associated with this syndrome. Although rare, these syndromes are seen because affected persons have normal health and life spans (
121).
A relationship between tarsal coalition and
clubfoot deformity has also been reported (
122,
123,
124,
125 and
126). Turco (
126) reported 8 feet in a series of 240 resistant clubfeet to have tarsal coalitions in the region of the sustentaculum tali. Callahan (
122) reported a single clubfoot discovered intraoperatively to have an absent tibialis posterior tendon and a middle facet talocalcaneal coalition. Five cases of arthrogryposis multiplex congenita have been described in association with tarsal coalition (
123). Spero et al (
124) reported 18 cases (14 patients) of rigid equinovarus deformity with a tarsal coalition. In their series, preoperative radiographs demonstrated the coalition in only a single case, and the coalitions in the other cases were identified at surgery or at morbid dissection. These authors suggested the possible preoperative use of magnetic resonance imaging (MRI) studies to identify the presence of any coalition before surgical treatment.
Takakura et al (
127) in 1991 reported a possible association between tarsal coalition and
tarsal tunnel syndrome. In 23 of 67 feet with symptomatic talocalcaneal coalitions, these investigators found tarsal tunnel syndrome to be present. They believed that the bony eminence in the area of the middle facet most likely accounted for the external compression on the posterior tibial nerve. In a later paper, Takakura et al (
128) discussed seven cases of tarsal tunnel syndrome that were believed to be caused by a medial talocalcaneal coalition and a concurrent ganglion. They excised the coalition and ganglion in six of the seven cases with mixed results. In 2002, Lee et al (
129) described the ultrasonic findings of tarsal tunnel syndrome caused by a talocalcaneal coalition.
Finally, one study noted that patients with tarsal coalition had significantly
lower bone densities than normal patients. The trabecular bone density was approximately 17% lower, on average, in patients with a tarsal coalition. These investigators concluded that the pain and gait changes associated with a tarsal coalition may lead to inactivity, resulting in a decrease in bone density (
130).
CLASSIFICATION
Tarsal coalitions may be classified in several ways: (a) etiologic type, (b) anatomic type, (c) tissue type, and (d) according to articular involvement. Downey (
131,
132) proposed the last classification (i.e., according to articular involvement) as a surgically based classification system that relates criteria associated with a particular tarsal coalition to the likelihood of surgical success with a proposed procedure.
Tarsal coalitions may be classified according to their origin, as either congenital or acquired (
53). This classification is not generally helpful in ascertaining the best possible treatment plan. Tarsal coalitions may be classified according to their anatomic constituents. Tachdjian (
118) provided a classification that subdivides coalitions into the bones that are abnormally united or, infrequently, part of a complex malformation (
Table 45.1). Although only descriptive, Tachdjian’s classification suggests the importance of assessing other areas of the foot and the remainder of the body when an apparently local or isolated coalition is identified.
Another common way of grouping tarsal coalitions is to classify them according to the tissue type of their union. In this way, a coalition may be a
synostosis (osseous union), a
synchondrosis (cartilaginous union), a
syndesmosis (fibrous union), or a combination of these. A synostosis may evolve from a synchondrosis or a syndesmosis. Investigators have theorized that this occurs with age or possibly after trauma to the coalition (
36,
38). A synostosis is also referred to as a
complete coalition because all motion is necessarily absent. An
incomplete coalition is fibrocartilaginous and has varying amounts of interposed cartilaginous or fibrous tissue that may allow motion between the bones involved. The tissue type of the coalition may be important when one is attempting to diagnose this condition.
By combining the aforementioned classifications, one may make a useful description of a tarsal coalition. For example, a tarsal coalition may be described as a congenital synchondrosis of the middle facet of the talocalcaneal joint. Given this information (i.e., the cause, tissue type, and anatomic constituency), one may more accurately understand the tarsal coalition present. However, these classification systems, even when combined, are only descriptive and provide only a small amount of information related to the development of a surgical treatment plan.
Identifying this deficiency, Downey (
131,
132) proposed the
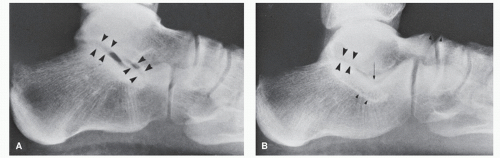
Articular Classification System based on the articular relationship of the bones involved in the coalition and the indirect effect of the coalition on surrounding joints (
Table 45.2). This articular classification system, when combined with the descriptive parameters already discussed, may serve as a basis for communication about possible surgical treatment. The classification assumes that the most important criteria for determining treatment are the age of the patient, the type of coalition, and the degree of secondary arthritic changes. The classification begins by distinguishing between juvenile (osseous immaturity) and adult (osseous maturity) tarsal coalitions. These conditions are then further subdivided into the types of coalition, whether extra-articular or intra-articular (
Table 45.3).
Extra-articular coalitions are those that occur outside a normal joint. These coalitions are commonly called
bars, and the calcaneonavicular coalition is the most frequently occurring example.
Intraarticular coalitions occur at normal joint sites and have been referred to as
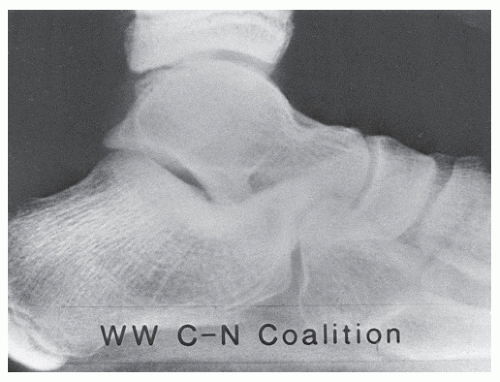
bridges. A talocalcaneal coalition of the middle facet of the subtalar joint is the most common example of an intra-articular coalition. Finally, the classification is subdivided into the presence or absence of significant secondary arthritic or adaptive changes within surrounding joints. As an example, a middle facet talocalcaneal coalition occurring in an adult with secondary arthritic changes at the talonavicular or calcaneocuboid joints would be an “adult IIB” coalition or an “adult intra-articular coalition with secondary arthritic changes” (
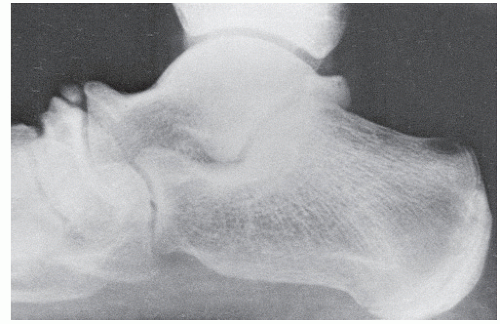
Fig. 45.3). A calcaneonavicular coalition occurring in a child with no secondary arthritic changes would be a “juvenile IA” coalition or a “juvenile extra-articular coalition without secondary arthritic changes” (
Fig. 45.4). In this manner, treatment plans may be related to the classification system.
While the Articular Classification System is not meant to be all-inclusive, it does describe important considerations used in the development of any treatment regimen. As noted, the original description included several parameters: patient age, articular involvement, and the extent of secondary adaptive or arthritic changes (
131,
132). In addition to these factors, Downey (
133) has more recently recommended that the size of the coalition, and possibly the degree of heel valgus, also be considered when developing a surgical treatment plan, especially with talocalcaneal coalitions.
CLINICAL FINDINGS
Tarsal coalition may be completely without symptoms and an incidental finding on routine radiographs. In a study of 23 patients with tarsal coalition, Jack (
57) found that 5 (22%) had no symptoms. Three clinical findings—pain, limitation of motion, and muscle spasm—should make the clinician suspect a tarsal coalition. Unfortunately, these patients are often erroneously treated for recurrent ankle sprains, sinus tarsi syndrome,
tarsal tunnel syndrome, or other problems that may cause pain in the rearfoot and ankle. A thorough understanding of the common clinical findings associated with tarsal coalitions, at the very least, permits a high index of suspicion for possible coalition after a routine history and physical examination.
Pain is a common finding in patients with tarsal coalition. The pain is usually deep and aching and is frequently in the area of the tarsal coalition. Rarely, it is neuritic. Kumai et al (
36) examined 55 coalitions histologically and found that no nerve endings existed in the coalition itself, but numerous nerve endings were present in the periosteum around the coalition site and in the articular capsule surrounding affected tarsal bones. Further, their study found histologic evidence of vascular proliferation, bleeding caused by vascular damage, osteoblastic and osteoclastic activity, interposition of fibrous connective tissue containing large amounts of cellular components, and irregularity of the cartilaginous bony interface at the boundary between the coalition site and the bone tissue involved. Thus, the pain in a tarsal coalition does not appear to be mediated by nerve endings in the coalition site and is more likely secondary to repeated mechanical stress, with cycles of microfracture and remodeling, with the associated pain mediated by free nerve endings in the surrounding periosteum and strained articular capsules. Katayama et al (
134) also discussed a case that showed an association of symptoms and progressive ossification seen on diagnostic imaging. Their patient developed his symptoms simultaneously with ossification of the coalition, which suggested that his pain was caused by mechanical stress.
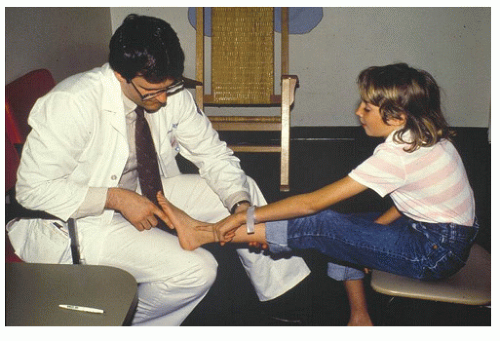
The patient often can localize the pain to the sinus tarsi, the anterolateral part of the ankle, or the dorsum of the midfoot. With a middle facet talocalcaneal coalition, the patient may indicate that the pain encompasses the entire rearfoot and localizes the pain to the sustentaculum tali medially and the sinus tarsi laterally (
Fig. 45.5). If significant secondary arthritic changes are present, the pain may be greatest in these areas (e.g., at the talocalcaneal coalition). If the patient is unable to pinpoint the pain, the clinician can usually localize it accurately with firm palpation.
The onset of the pain is usually insidious, developing after some unusual activity (e.g., excessive walking, hiking, or running) or innocuous trauma (e.g., minor ankle sprain). Rarely, trauma to the foot or ankle injures the area of the coalition (
135,
136 and
137). This symptom-producing injury has been termed “awakening” trauma (
138). Further, investigators have stated that all coalitions are initially cartilaginous and eventually ossify and have suggested that the different coalitions ossify at different ages and the pain begins as this ossification process occurs. Cowell stated that a talonavicular coalition ossifies from the ages of 3 to 5 years, a calcaneonavicular coalition ossifies from the ages of 8 to 12 years, and a talocalcaneal coalition ossifies from the ages of 12 to 16 years (
139) (
Table 45.4).
The pain associated with a tarsal coalition is usually aggravated by activity and is relieved with rest. On questioning, the patient frequently relates pain associated with walking over rough, uneven terrain, with prolonged standing, or with athletic activity. Investigators have hypothesized that the decreased rearfoot motion associated with a tarsal coalition may cause an increase in laxity of the ankle ligaments and may result in more frequent sprains in the patient with a coalition (
140). Evidence to support this hypothesis came from Snyder et al (
141), who, in 1981, retrospectively examined the radiographs of patients with sprained ankles (no other clinical criteria were used) and reported a 63% incidence of calcaneonavicular abnormalities. However, the radiographic criteria used for their assessment were marginal. In a study of 48 patients with tarsal coalition, Gonzalez and Kumar (
142) reported that nine (19%) were initially seen because of repeated ankle sprains. Appropriately, investigators have suggested that any active adolescent with recurrent ankle sprains or strains should be considered as potentially having a tarsal coalition until proven otherwise (
143,
144).
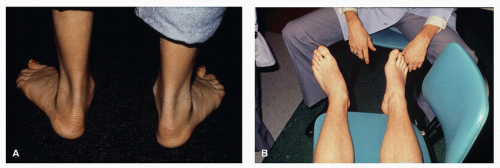
Limitation of subtalar and midtarsal joint motion is common with tarsal coalition and is typically the most obvious clinical finding. Usually, the subtalar joint is limited in the direction of inversion. This limitation becomes even more apparent when
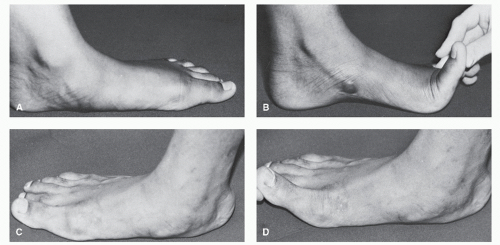
peroneal muscle spasm is present. In the case of an incomplete coalition, as ossification progresses, range of motion at the subtalar and midtarsal joints decreases. Clinical examination for subtalar and midtarsal joint motion may be performed with the patient both seated and standing. While the patient is seated, the examiner may assess the subtalar and midtarsal joints passively for the amount of motion available. A decrease in motion may be found in either or both joints. In unilateral cases, the motion may be compared to that of the contralateral limb. Similarly, it is easy to evaluate the patient while he or she is standing. If a pes valgo planus deformity is present, as is seen with the typical peroneal spastic flatfoot, the
Hubscher maneuver or the
toe test of Jack may be used to assess the flexibility of the deformity. These maneuvers involve passive dorsiflexion of the hallux while the patient stands in a normal, relaxed position. When the hallux is dorsiflexed, the medial strand of the plantar fascia and the flexor hallucis longus are tightened via the windlass mechanism. If the deformity is flexible, the medial longitudinal arch will increase in height and the rearfoot will supinate (
Fig. 45.6A and B). If the deformity is rigid, as typically seen with a tarsal coalition, no change in the longitudinal arch will be seen (
Fig. 45.6C and D). Cass and Camasta (
145) described how a false negative Hubscher maneuver could occur in a patient without a tarsal coalition and concomitant ankle equinus. They surmised that the posterior equinus contracture could preclude the ability to reproduce the arch height in an otherwise flexible deformity. Therefore, they recommended that a “step-forward” Hubscher maneuver be performed. In this way, the patient stands and steps forward with the extremity to be examined. This “step-forward” plantarflexes the foot on the leg and negates the effect of the ankle equinus. With the gastrocsoleus complex relaxed, a more accurate Hubscher maneuver can be performed.
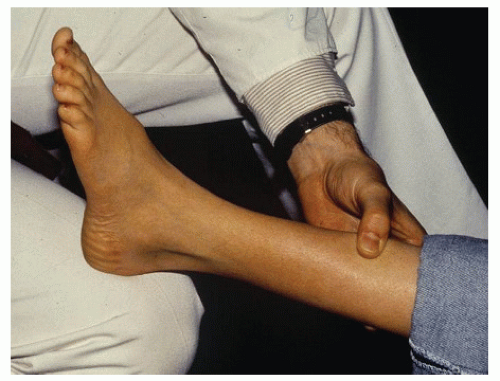
Another method of assessing subtalar joint motion is to ask the patient to roll to the outside of the feet (i.e., invert the feet) and then to roll to the inside of the feet (i.e., evert the feet). In patients with a tarsal coalition, inversion is diminished (
Fig. 45.7). Koeweiden et al (
146) advocated a similar test, which they termed the
heel-tip test, and in nine patients with known talocalcaneal coalitions, they found 8.4 degrees of motion as compared with 27 degrees of motion in 60 anatomically normal control feet. Other investigators have proposed that measurement of hindfoot movement helped to quantify the extent of restriction and aided in the earlier detection of coalition (
147).
With tarsal coalition,
tonic muscle spasm may occur. It should be clearly understood that this is a tonic muscle spasm and
not clonic muscle spasticity. Electrodiagnostic studies have confirmed the absence of true neurologic clonic spasm (
148). The peroneus brevis is usually the muscle that is most significantly involved. However, spasm of the peroneus longus, tibialis anterior, tibialis posterior, gastrocnemius, and soleus may occur (
149,
150 and
151). Investigators have theorized that as subtalar joint motion becomes painful, the peroneus brevis attempts to guard or restrict this motion. This tonic spasm resembles abdominal muscle guarding in a patient with appendicitis. In the simplest sense, it is a subconscious attempt by the peroneus brevis to limit painful motion. This spasm is not neurologic, as in clonic spasticity, but represents simply an increase in tension of the peroneus brevis muscle-tendon unit (i.e., tonic spasm). The muscle spasm, like pain associated with the coalition, is precipitated by activity and is relieved by rest.
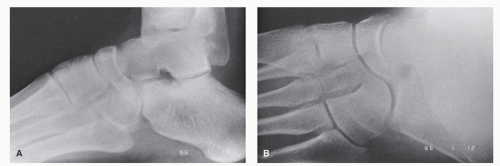
The peroneus brevis muscle spasm may be intermittent or continuous. As the symptoms progress, the muscle guarding or tonic spasm generally becomes more intense. As the peroneus brevis contracts, subtalar joint motion is further
restricted, and the taut tendon may be palpated or observed laterally (
Fig. 45.8). The rearfoot is maintained in a valgus position with depression of the medial longitudinal arch and abduction of the forefoot. The rearfoot valgus occurs because this is the position of comfort of the foot. Kyne and Mankin (
152) tested the intra-articular pressure of the subtalar joint during range of motion. They found that pressure within the subtalar joint is increased with inversion. When joint effusion was present, a reflex mechanism to limit painful inversion ensued. Thus, the peroneus brevis spasm is nothing more than reactive immobilization of a swollen, painful joint to maintain that joint in the position of maximum capsular capacity (i.e., eversion). With time, and if left untreated, the valgus deformity will become more rigid. In this manner, tarsal coalition may become associated with rigid peroneal spastic flatfoot. Further, significant forefoot supinatus, forefoot abductus, and changes secondary to associated ankle equinus may become apparent. Clinical identification of these secondary adaptive changes is imperative to the development of an appropriate treatment plan (
Fig. 45.9). Cass and Camasta (
145) described a “Gray Zone” group of patients who have an incomplete tarsal coalition that has not yet ossified and therefore have varying degrees of motion available in the hindfoot. These patients do not have a rigid pes valgoplanus deformity and do not have a flexible pes valgoplanus deformity either. These “Gray Zone” patients have signs and symptoms lying somewhere in between the extremes, and a semirigid pes valgoplanus deformity (
145).
Peroneal spastic flatfoot does not always occur with tarsal coalition, and peroneal spastic flatfoot may result from other conditions (
153). Occasionally, other muscles may be spastic in patients with a tarsal coalition. If other muscles are involved, the foot may not develop a pes valgo planus attitude. Several authors have reported a varus position of the heel in patients with a tarsal coalition (
51,
131,
142,
151,
154,
155,
156,
157 and
158) (
Fig. 45.10). Further, peroneal spastic flatfoot may occur secondary to other causes, including arthropathies, inflammation, infection, and osteochondral fractures (
159). These may also be considered acquired causes of tarsal coalition in certain instances. Lowy (
153) outlined a suggested protocol for evaluating and treating patients with peroneal spastic flatfoot deformities with or without associated tarsal coalitions and advocated the use of a common peroneal nerve block to reduce the spastic muscular contracture and to allow better evaluation of joint motion.
Similarly, during evaluation of a patient who has a tarsal coalition associated with restricted motion or muscle spasm, a local anesthetic injection in the area of the coalition or to a proximal nerve segment (e.g., a common peroneal block) may provide valuable diagnostic information. The anesthetic block may relieve the pain and muscle spasm sufficiently to allow more accurate assessment of joint motion. This technique not only allows direct confirmation of the extent of the coalition (i.e., complete vs. incomplete) but also may afford information on the quality and quantity of joint motion. This information may be helpful if surgery is considered and resection of the coalition is contemplated.




 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access