CHAPTER 34 Surgical wounds and incision care
1. Discuss current issues related to surgical wound infection and recommendations made by national collaboratives or evidence-based guidelines to address these problems and improve outcomes.
2. Compare intrinsic and extrinsic (modifiable) patient characteristics associated with surgical wound healing complications or infection.
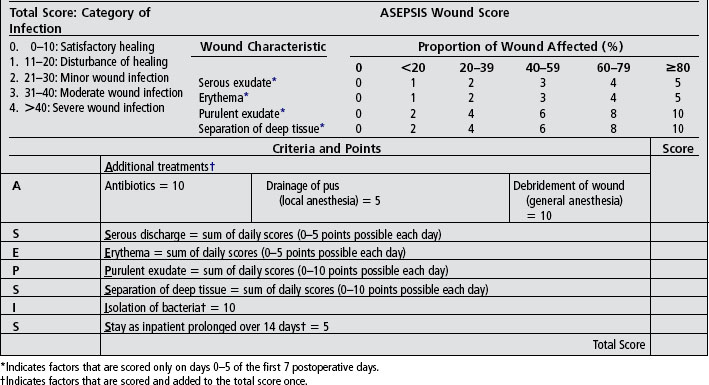
3. Identify wound assessment characteristics comparing the ASEPSIS method of evaluating wounds with Centers for Disease Control and Prevention–defined characteristics for surgical site infection.
4. Identify evidence-based measures for surgical wounds, including dressings, topical treatment, and care of sutures, staples, and tissue adhesives.
5. Discuss three aspects of care or evaluation for patients with surgical wounds and how they can help to promote healing and prevent complications of healing.
Approximately 30 million surgeries are performed each year in the United States (Centers for Disease Control and Prevention [CDC], 2009). Although surgical procedures have become less invasive through the development and use of arthroscopic and laparoscopic techniques, many surgeries still are performed through open incisions. Even the less invasive surgical approaches create an incision and an acute wound requiring a normal physiologic wound healing response (see Chapter 4). Surgical wounds that heal within an expected time frame and without complications are considered acute wounds (Franz et al, 2008). In caring for the patient with a surgical wound, a major goal is preventing complications such as surgical site infection (SSI) and wound healing failure through careful surveillance and interventions. Surveillance is largely accomplished through patient evaluation for risk factors and assessment of the surgical wound for signs of disruption in healing. Interventions are targeted toward reducing modifiable risk factors associated with healing complications, providing systemic and environmental support to facilitate healing to the greatest extent possible. Box 34-1 lists the 11 impediments to surgical wound healing addressed in the guidelines (Franz et al, 2008), many of which are addressed in detail in chapters throughout this text.
BOX 34-1 Impediments to Surgical Wound Healing
Surgical wound closure
The goal of wound healing is to reestablish tissue integrity and function with a cosmetically acceptable result and to prevent infection. These are also the goals of wound closure. Surgical wounds are closed primarily or are left open for either delayed primary closure or healing by secondary intention (see Figure 4-2). Primary wound closure is the fastest method for facilitating wound healing (Hollander, 2003). However, wounds with greater than 105 bacteria per gram of tissue should not be closed (Franz et al, 2008). In these cases, wounds are often left open and then closed on a delayed schedule, but ideally within a few days, once bacterial load is reduced below critical levels and the wound bed is healthy and can support healing. Primary repair should approximate (Plate 67), but not strangulate, the incision (Franz et al, 2008). Incisions are approximated with sutures, staples, adhesive tapes, and skin adhesives to provide support and stability to tissues until healing has progressed and an acceptable degree of wound tensile tissue strength is reestablished.
Sutures and staples
Multiple techniques and suture materials are available for closing an incision. National guidelines state that the type of suture material used does not matter, as long as the primary repair is anatomic and perfused (Franz et al, 2008). The choice of suture technique depends on the type and anatomic location of the wound, the thickness of the skin, the degree of tension, and the desired cosmetic result. For example, absorbable sutures are used to close tissues deeper than the epidermis and to provide tissue support, relieve skin tension, and reduce wound dead space (Hollander, 2003). Continuous sutures are recommended for closure of laparotomy fascial incisions; however, the type of suture does not affect healing. Current evidence indicates that external or internal retention sutures do not prevent dehiscence and that dehiscence is more likely associated with other factors such as comorbidities (e.g., trauma and wound contamination) (Franz et al, 2008). Staples are commonly used to close the epidermis with acceptable healing and cosmetic result and no increase in infection (Hollander, 2003).
Sutures should be removed within 1 to 2 weeks of their placement, depending on the anatomic location: 3 to 5 days for the face; 7 to 10 days for scalp, chest, fingers, hand, and lower extremity; and 10 to 14 days for the back, forearm, and foot (Hollander, 2003; Wu, 2006). Sutures left in too long can lead to suture marks, local tissue reaction, and scarring. Premature suture removal places the wound at risk for reopening (Hollander, 2003; Wu, 2006). With the appropriate equipment, suture and staple removal is not difficult. The suture should be gently grasped by the knot and elevated slightly with forceps. One side of the suture is cut at skin level. With the forceps still grasping the knot, the suture is gently pulled toward the wound or suture line until the suture material is completely removed (Wilson et al, 2000).
Skin adhesives
Tissue adhesives and derivatives of cyanoacrylate and other materials that add strength and flexibility have been used for several years for lacerations and other types of wound closure. A Cochrane review of eight randomized trials enrolling 630 patients compared adhesives to suture used for incision closure and identified no differences in rates of dehiscence or infection (Coulthard et al, 2002). The authors also noted that evaluation of adhesives in patients with healing risk factors and for wounds with high tension requires additional study because these subpopulations were excluded from the trials that were reviewed, therefore the comparative effectiveness is not known. Skin adhesives are not recommended for use with complex lacerations having wound edges that are difficult to approximate (Hollander, 2003). No removal is required for adhesives, although some cannot be exposed to water. Ointments should be avoided because they may loosen the adhesive and cause wound dehiscence (Hollander, 2003). Tissue adhesives slough off 5 to 10 days after they are applied.
Steri-strips.
Wound closure tapes, or Steri-Strips, are reinforced microporous surgical adhesive tape. Steri-Strips are used to provide extra support to a suture line when running subcuticular sutures are used or after sutures are removed. Wound closure tapes may reduce spreading of scar if they are kept in place for several weeks after suture removal. Often they are used with a tissue adhesive. These tapes are rarely used for primary wound closure (Wilson et al, 2000).
Surgical wound assessment
Clinically, there is no single, standard, widely accepted method for assessing healing of acute wounds. Deposition of collagen in the wound begins immediately in the inflammatory phase and peaks during the proliferative phase, approximately 4 to 21 days after wounding. Sufficient synthesis of collagen early during the healing process is critical to successful repair. Wound dehiscence is most likely to occur fairly early after surgery (by postoperative day 5 to 8) in patients in whom normal physiologic healing responses, such as collagen synthesis, lag. However, a method for direct observation of collagen production in acute wounds has not been validated, thus the term healing ridge is not mentioned in the acute wound guidelines and has been deleted from Outcome and Assessment Information Set (OASIS) documentation requirements (Whitney et al, 2008; WOCN, 2010).
Asepsis scoring tool
Acute wound complications can be evaluated on the basis of specific parameters using the ASEPSIS scoring tool. ASEPSIS is an acronym for seven wound assessment parameters that are described within the tool and presented in Box 34-2. The ASEPSIS tool is the most frequently used quantitative tool for surgical wound evaluation (Bruce et al, 2001) and offers a scale for evaluating surgical wounds with greater objectivity and ability to be reproduced. The ASEPSIS method was originally developed in cardiac surgery patients to evaluate characteristics of the surgical incision associated with infection (Wilson et al, 1986a). In a validation study, ASEPSIS was reported to be as sensitive and significantly more specific compared to other clinical indicators of wound problems or to wound assessments made using standard definitions of wound infections (Wilson et al, 1990). Interrater reliability of 0.96 has been reported in patients undergoing general surgery (Byrne et al, 1989). Similar reliability has been shown for sternal and leg wounds of patients after cardiac surgery (Wilson et al, 1986b). Topaloglu et al (2008) noted statistically significant correlations between preoperative wound infection risk indices and ASEPSIS scores. The authors of this study reported ASEPSIS was easy to use, repeatable, and effective as an infection surveillance method. Summed scores over wound assessments performed each day for the first 5 postoperative days indicate severity of infection or complication.
Impediments to surgical wound healing
Although ongoing assessment of the surgical wound is critical, identifying impediments to healing is important so that they may be minimized or eliminated when possible. Box 34-1 lists impediments to surgical wound healing (Franz et al, 2008). Most (perfusion and smoking, nonviable tissue, infection, mechanical factors, obesity, diabetes, malnutrition, and burn injuries) are discussed in great detail in chapters throughout this text.
Hematoma or seroma.
The occurrence of hematoma or seroma in surgical wounds has increased because of greater clinical use of anticoagulants and prophylactic treatments now recommended and implemented for deep vein thrombosis (Franz et al, 2007). When detected, hematoma or seroma requires intervention for removal by needle aspiration or prophylactic drainage (Franz et al, 2008). The presence of fluid collections, seromas, or hematomas delays healing in acute wounds through mechanisms of pressure and ischemia to the wound edges and adjacent tissues (Franz et al, 2008).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree