Fig. 10.1
A 70-y/o male with significant peripheral vascular disease with distal ischemia who presented after revascularization with ankle osteomyelitis. (a, b) X-ray imaging shows diffuse osteopenic changes with nonspecific periosteal reaction in the distal tibia and fibula. (c) Patient underwent 3 debridements with talectomy (d, e). Tibial calcaneal arthrodesis with application of circular frame external fixation. (f) Healed tibial calcaneal arthrodesis with healed skin graft after negative pressure wound therapy with wound reconstruction. Patient was able to walk without limitations 5 months after initial procedure
Whether single-stage or multiple-stage surgical procedures are utilized; a key principle to surgical treatment of DFOs is to remove all infected soft tissue and bone. Intraoperative specimens can be sent for histology to ensure free margins at the time of primary intervention or subsequent procedures in the case of delayed results [9, 10, 13, 29]. In a study by Atway et al., 81.8 % of patients with positive bone margins after intervention had poor long-term outcomes. The routine standardized bone margin culture should be obtained in all patients with reinterventions [30]. The evidence reveals that when adequate soft tissue coverage remains after debridement, excellent long-term healing can be achieved. Patients who present with bone involvement can undergo internal and external fixation, separate or in combination for stabilization and simultaneously to allow for eradication of infection and subsequently produce a long-term functional extremity (Fig. 10.2).
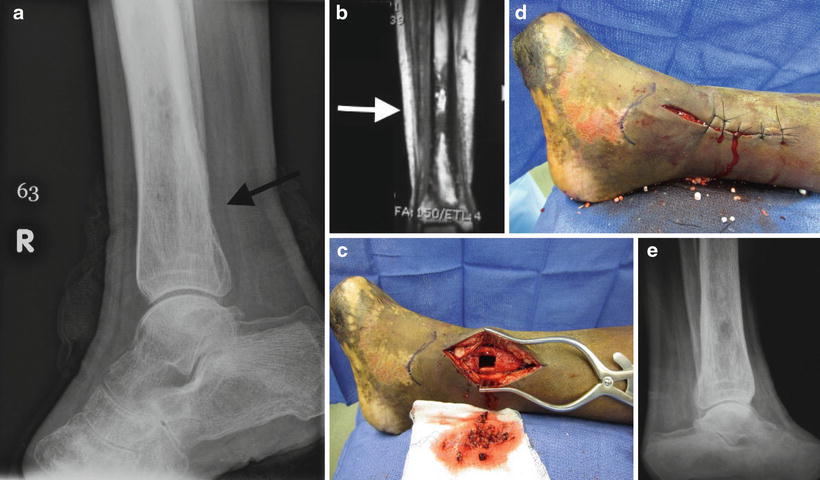
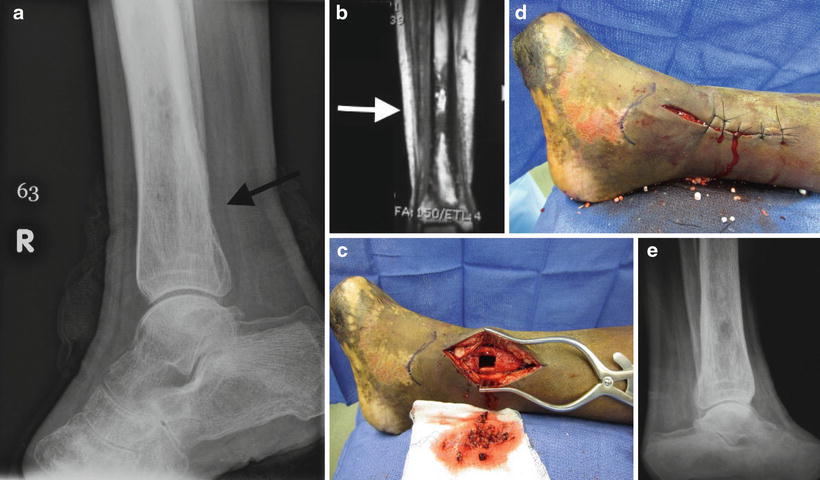
Fig. 10.2
Patient was a 26-year-old female with leukemia who developed hematogenous osteomyelitis after MRSA bacteremia. (a) Preoperative X-ray showed a permeative lesion with endosteal scalloping within the distal tibial diaphysis and metaphysis with associated periosteal reaction, suspicious of osteomyelitis. (b) MRI confirmed tibial osteomyelitis. (c) Underwent single-stage resection of tibial osteomyelitis with window created for packing Stimulan antibiotic beads. (d) Primary closure over defect. (e) Follow-up X-ray, patient completely healed and able to utilize for walking
Tissue Reconstruction
The surgical approach to osteomyelitis of the diabetic foot and ankle can be dependent upon closure and reconstructive options. Numerous factors impact these complex reconstructive strategies. Surgery still can minimize adverse events with respect to the patient and their outcomes. The reconstructive ladder, a concept familiar to plastic surgeons, provides a framework for this advanced reconstructive decision-making [31]. Several iterations of the reconstructive ladder have been proposed; however one of the most recent versions, created by Janis et al., incorporates the traditional model with new wound healing strategies using negative-pressure wound therapy (NPWT), dermal matrices and increased utilization of local flaps [31]. The base of the ladder is primary closure with the transition to closure by secondary intention, negative pressure wound therapy, skin graft, dermal matrices, local flaps, distant flaps, tissue expansion, and free flaps as a last option. The reconstructive hierarchy created is an obvious simplification of complex decision-making process between the surgeon and patient. The algorithm can guide surgical planning and focus on restoration of limb function [32] (Fig. 10.3).
Fig. 10.3
Reconstructive ladder
A successful surgical debridement can lead to complete primary wound closure which is the base of the reconstructive ladder. Garcia Morales et al. looked at 46 patients with DFO who underwent bone and soft tissue debridement and had either primary surgical closure [33] or were allowed to heal by secondary intention [14]. They found that primary surgical closure was associated with a reduced average healing time and no increase in postoperative complications [34]. However, in patients with DFOs that have extensive infection or late presentations, the preservation of soft tissue during surgical debridement and primary closure may not be possible. Significant tissue loss poses a challenge for reconstruction of the subsequent skeletal and soft tissue defects. These patients may be candidates for alternative soft tissue coverage using sking grafts, local/free muscle flaps or skeletal restoration and stabilization with bone grafts.
Primary closure or closure by secondary intention may not be an option and therefore a new addition to the reconstructive ladder was first described by Morykwat et al. in 1997 [35]. The success of NPWT in aiding wound healing is due to several different factors. Morykwat et al.’s original research on animal models noted an increased formation of granulation tissue in wounds treated with NPWT [35]. Zoch et al. then looked at the effect of NPWT on tissue perfusion in diabetic foot infections. They found a 31 % increase in perfusion to the wound and a 14 % increase in perfusion of surrounding tissue during NPWT therapy [36]. Additionally, Kamolz et al. concluded that NPWT had a reduction in peripheral edema, as a result of fluid removal [37]. These factors play a role in the therapeutic benefit of NPWT for wound closure. Some of the other alternative treatments for wound therapy include advanced moist wound therapy (AMWT), bioengineered tissue or skin substitutes, growth factors, and electric stimulation. In 2008 Blume et al. looked at the safety and efficacy of NPWT compared to AMWT specifically [38]. Their study was a multicenter randomized control trial, which enrolled 342 diabetic patients with foot ulcers who were followed up to 9 months. Findings showed a greater proportion of foot ulcers achieved complete closure with NPWT than with AMWT (43.2 % vs 28.9 %, p = 0.007). The NPWT group also had significantly fewer secondary amputations (p = 0.035). They concluded that NPWT is safe and more efficacious than AMWT. This study looked at diabetic ulcer healing and not specifically at patients with osteomyelitis. A Cochran Review published in 2013 evaluating the effects of NPWT compared with standard care echoed the results of Blume’s study. They concluded that there is evidence to suggest that NPWT is more effective in healing postoperative foot wounds and ulcers of the foot in people with DM compared with moist dressings [39]. NPWT has not been directly compared to closure by secondary intention. There are many expanded therapeutic benefits in wounds beyond the scope of standard NPWT which can aid in healing of poorly vascularized tissue such as bone or tendon. These tissues are at increased risk to break down after closure by secondary intention and skin grafting leading to suboptimal results with thin, unstable coverage. Lee et al. published a small case series looking at 16 ankle wounds that had exposed bone and tendon. They were able to successfully granulate and graft 15 wounds with NPWT [40]. Bollero et al. similarly, described a series of 37 complex, high-risk, lower extremity wounds which were successfully reconstructed using NPWT [41]. Wound size, unfortunately still plays a limiting factor on the utilization of NPWT, with larger defects often requiring flap coverage for complete healing.
With large, complex wounds that are not amenable to primary closure or aided closure with NPWT, local flaps, and perforator flaps are the next sequential step up the reconstructive ladder. Local muscle flaps appeared in the late 1960s and were used exclusively for foot and ankle reconstructions until the late 1970s when microsurgical free flaps gained popularity [42]. Patients with large soft tissue defects that require aggressive bone resection in order to create an adequate soft-tissue envelope for primary closure can result in a mechanically unstable foot and ankle, which can be prone to future breakdown and tissue loss. The goal of limb preservation does require adequate coverage especially at anatomic sites at risk of failure such as weight bearing areas and mobile joints. Fasciocutaneous flaps are often inadequate due to limited size, mobility, and durability, while intrinsic muscle flaps are well-vascularized alternatives that are versatile and have shown to hold up better over time [43]. There are many muscle flaps that provide coverage for foot and ankle reconstruction. These include the abductor hallucis brevis for medial midfoot, heel and ankle defects; the abductor digiti minimi for lateral ankle and calcaneal defects; the flexor digiti minimi for midfoot defects; the flexor digitorum brevis for plantar heal defects; and the extensor digitorum brevis for anterior ankle defects [33, 44, 45]. There are many advantages for the use of intrinsic or local muscle flaps. They can be harvested with a simple ankle block, minimizing the anesthetic risk, and the donor site can almost always be closed primarily. A study by Ducic et al. looked at the effectiveness of pedicled muscle flaps in patients with diabetes for complex foot and ankle reconstruction. In this analysis, 32 patients received 34 pedicled muscle flaps with results showing a 91 % (31/34) success rate, and a 94 % limb salvage rate. Overall, only 15 complications were reported at the completion of all 45 reconstructive procedures. Compared to historical controls of nondiabetic patients, they did not find any difference in wound healing rates, flap success, limb salvage, or ambulatory status. There was a slight difference in the number of operations and healing times, with diabetic patients requiring twice as many operations and twice as long to heal as nondiabetic patients. Diabetic patients also had slightly decreased long-term survival; however, it was still far superior to the long-term survival rates of amputees. Additional advantages of local muscle flaps include increased blood supply, improved oxygen transport, and direct delivery of host defense mechanisms or antibiotics. Also, vascularized tissue from these flaps are able to conform to a variety of spaces, eliminating dead space and decreasing local bacterial counts [44, 46]. Local or pedicled flaps, however, are handicapped by the pedicle which carries the blood supply and assures viability thus restricting their area of reach and arc of rotation. In conclusion, local tissue flaps have a significant utility in reconstruction of defects in patients with DFO (Fig. 10.4).
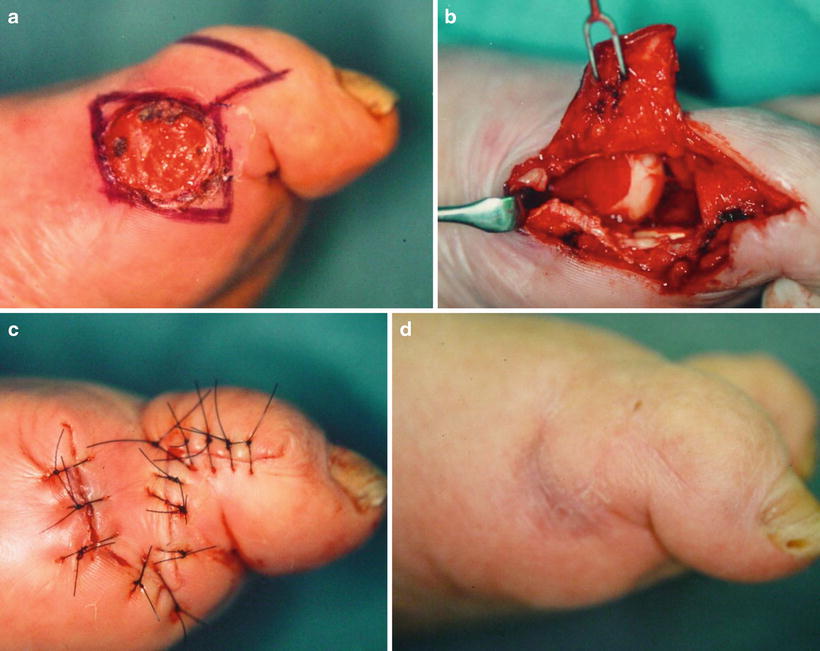
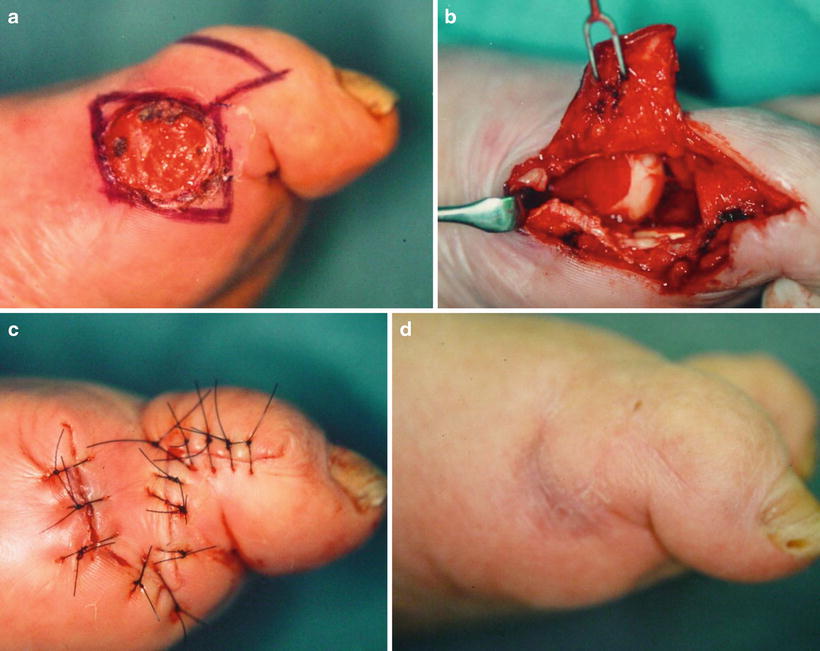
Fig. 10.4
(a) Osteomyelitis of first metatarsal phalangeal joint. (b–d) Single-stage resection approach including local flap reconstruction with biomechanical preservation
Although there are many advantages of using local flaps, each anatomic region of the foot and ankle has special reconstructive requirements that may preclude their use. The dorsum of the foot and ankle require thin, pliable, soft tissue for coverage of exposed tendons. Conversely, the skin over the plantar aspect must be flexible allowing for freedom of motion and enough durability in order to withstand constant pressure and force [47]. Free muscle flaps have provided an alternative method of tissue coverage to address these multiple considerations and sit at the top of the reconstructive ladder. Over four decades ago the first successful free composite tissue transfer was performed by McLean and Buncke in 1972 [48]. This was followed a year later by both Daniel and Taylor as well as O’Brien with the first transfer of island flaps from the groin to reconstruct traumatized lower extremities [49, 50]. The development and successful utilization of free-tissue transfer is especially important when planning intervention for patients with DFO, who require coverage after more radical excision of infected soft tissue and bone. Free flaps are highly vascularized via their own blood supply, enhancing the revascularization of a critically ischemic angiosome through the development of vascular connections between the flap and native tissue. Several different donor free flaps have been described in the literature. These include the lattismus dorsi perforator flap, antecubital flap, forearm flap, scapular flap, anterior lateral thigh flap, medial thigh flap, gracilis flap, and the deep inferior epigastric artery perforator flap (DIEP) [51–54]. Ohta et al. in 2006 reported on a small case series of 4 patients with DFO treated with free DIEP flaps. Their results showed that out of the four flaps, 3 took completely without any complications and one flap took with partial necrosis that healed with ointment treatment. Postoperatively, all patients were able to walk without difficulty [55]. In another small series by Omer et al., 13 patients with complications of DFO were treated with various free flaps. All reconstructed flaps survived well postoperatively, however they did have two major amputations reported due to persistent osteomyelitis. The overall limb salvage rate was 83 % [56]. In 2011, a meta-analysis and systematic review of free-tissue transfer in 528 diabetic patients with nonhealing wounds (55 % patients with specific mention of the presence of osteomyelitis) was reported by O’Conner et al. [57]. From the 18 studies evaluated, they found the overall flap survival rate was 92 % (primary patency rate was 86 %), and overall limb salvage rate was 83.4 % over a 28-month follow-up period. Only 16 studies reported on ambulation rate with a mean rate of 76 % (69.8–83.9, CI 95 %). In this review, the major cause of flap failure was infection, reinforcing the necessity for eradication of osteomyelitis as the priority in this population prior to reconstruction. Even though this review demonstrated successful wound healing and good functional outcomes after free-tissue transfer, it did not address the long-term impact on survival in patients with DFO. In 2012 Suk Oh et al. looked specifically at 5-year survival rates and preoperative risk factors affecting outcomes after free-flap reconstruction in patients with diabetes [58]. Out of 121 cases, 111 Free-tissue transfers were successful (flap survival rate of 91 %). Limb preservation was 84.9 % and the 5-year survival was 86.8 %. Risk factors associated with higher rate of flap failure included history of one or more angioplasty procedures (OR 17.59, p < 0.001), history of peripheral arterial disease (10.21, p = 0.032), and patients using immunosuppressive agents after renal transplant (4.86, p < 0.041). Patients who were treated for preoperative osteomyelitis did not show a statistically significant increased risk for flap failure in this series (OR 1.056, p = 0.935). Free flaps do allow for closure of complex wounds but often complicate function of the limb due to size and type of tissue transformed. The paradigm shift in reconstructive strategies for these patients has really changed to focus on eradication of bone infection with local tissue reconstruction, with free flaps as a last resort (Fig. 10.5).
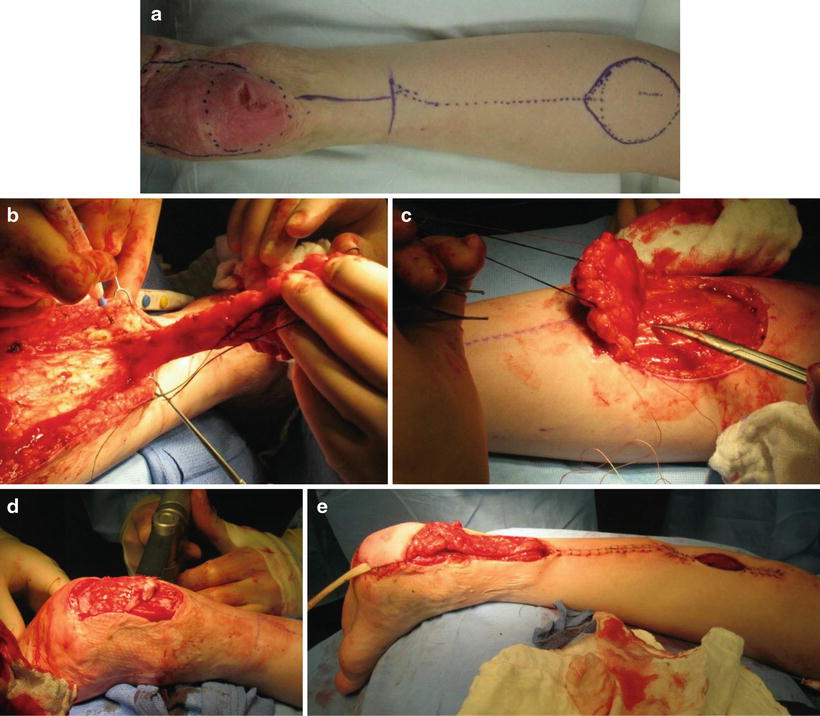

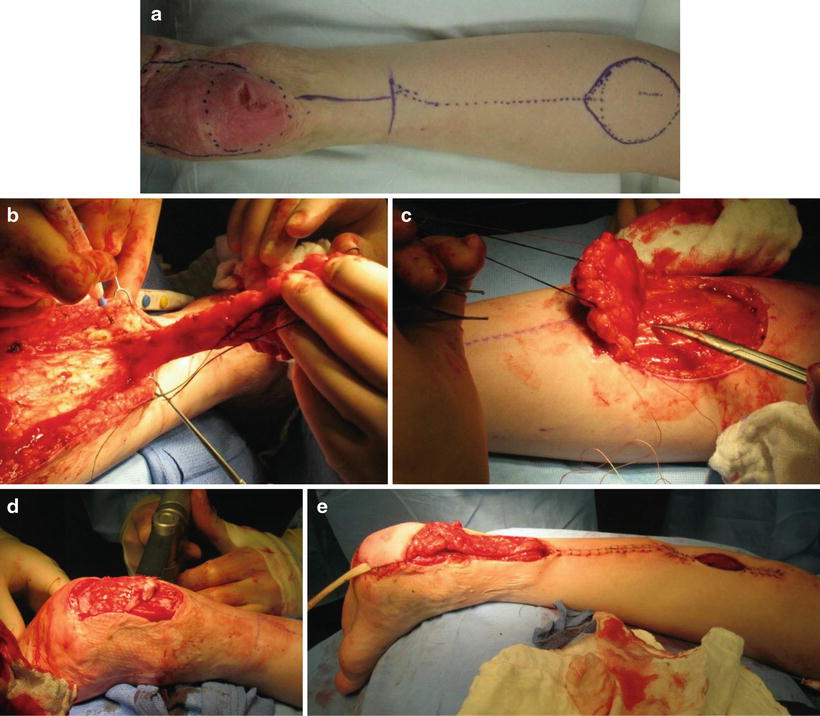

Fig. 10.5
(a–h): (a) Calcaneal osteomyelitis. (b–f) Resection and debridement of calcaneal osteomyelitis with Achilles tendon resection and reverse sural flap reconstruction. (g) External fixation placed for offloading. (h) Healed flap with mechanical preservation
The strong evidence that supports tissue reconstruction in patients with DFO is based on the aforementioned concepts of debridement with eradication of infection. It is paramount that these patients have a suitable vascular supply to provide adequate blood flow to the tissue. The approach to revascularization in patients with foot wounds or ischemic ulcerations was traditionally based on the “best vessel” approach, with surgical techniques focusing on getting blood flow from a proximal blood vessel to the best available distal vessel regardless of location. Several studies however have reported high rates of unhealed wounds despite patent bypasses or restored in-line flow via endovascular methods [59, 60]. This evidence has supported investigation in a new model of revascularization based on angiosomes. Angiosomes are three-dimensional blocks of tissue fed by source arteries with functional vascular connections between muscles, fascia, and skin. The foot and ankle are composed of six distinct angiosomes with the main arteries having numerous direct arterial–arterial connections to provide alternative routes of blood flow if the direct route is disrupted [61]. An angiosome based revascularization strategy attempts to reestablish flow to the source artery of a lesion, rather than focusing on the most suitable artery as the target for revascularization. A systematic literature review was published by Sumpio et al. in 2013 to evaluate this strategy [62]. They found 11 papers to include in their outcomes analysis, most of which were retrospective case series or reviews of prospectively kept databases. Ten of these studies compared direct revascularization (angiosome model) to indirect revascularization (best vessel model). Of these, five reported significant increase in limb salvage rates with direct revascularization. In addition 5 out of 8 studies that reported wound-healing rates found a significant increase in healing when following the principles of the angiosome revascularization strategy. Even though there is a limited amount of data available, these results support the ideal of attempting direct revascularization to the affected angiosome. Perhaps this is even more important in patients with diabetic foot wounds where they often have patchy atherosclerotic lesions, and destruction of collaterals, which will inhibit wound healing by indirect revascularization methods [63]. Another revascularization strategy for patients with significant peripheral arterial disease and inadequate inflow, is the use of combined vascular reconstruction and free-flap transfer for limb salvage. Vermassen et al. reported on 45 diabetic patients who underwent a combination of arterial revascularization and free-flap transfer [64]. The indications for all procedures were the presence of extensive gangrenous defects of the foot or lower leg with the exposure of bones or tendons. Patients were excluded in which treatment with a simple wound closure or split-thickness skin graft (STSG) wound have been possible or in whom postoperative ambulation wound not have been expected. In 45 patients, a total of 53 arterial reconstructions were performed, 37 of which the distal anastomosis was on a pedal or tibial vessel with either greater saphenous vein or cryopreserved homologous saphenous vein. Operative technique in these patients included a side-to-side anastomosis with the native vessel leaving a free end of the arterialized saphenous vein for an end-to end anastomosis with the flap artery. Venous anastomosis were performed on the concomitant deep veins in 38 patients with 3 patients having a superficial vein used as a second outflow, and 9 patients having superficial vein or mobilized lesser saphenous vein as primary outflow vessel. The remaining patients underwent a combination of two different levels either with bypass or percutaneous transluminal angioplasty plus bypass. At the conclusion of the study, reintervention was performed on 14 patients resulting in 5 flap losses (2 of which treated with new free flap, 3 were amputated), and 3 early postoperative deaths. Thirty-nine out of 45 patents (87 %) were discharged amputation free and 32/39 patients achieved independent ambulation. At 1-year follow-up, combined survival and limb-salvage rate was 84 % after 1 year. Subsequently in 2009 Random et al. published a similar study evaluating results and complication of combined simultaneous arterial revascularization and free-flap transfer in patients with critical limb ischemia and large soft-tissue defects. Only 70.5 % of their population was diabetic with 38 % presenting with osteomyelitis. They reported superior limb salvage at one year of 93 % decreasing to 71 % at 5-year follow-up. Combined 1-year limb salvage and survival was similar to Vermassen et al.’s results at 85 %. Some of the benefits of this combined approach is that free-flap transfer offers additional outflow to the bypass; as poor outflow and increased vascular resistance is a major cause for overall distal bypass failure. Lorenzetti et al. specifically investigated this concept and found that the low-resistance outflow bed of transferred muscle could increase graft flow by up to 50 % [65]. Based on these results, combined revascularization and tissue transfer in complicated diabetic patients with large defects not amenable to other reconstructive options, is a preferable option over primary major amputation with acceptable long-term survival and limb salvage rates. Whether a direct revascularization strategy based on an angiosome model or revascularization with combined tissue transfer is used, the importance of adequate blood flow available for wound healing cannot be stressed enough.
Adjuvant Agents
Total eradication of infection and reconstruction in patients with DFO was traditionally accomplished solely with surgical intervention as previously described. In many of these patients, however, there has been increasing evidence to support the addition of a few select adjuvant therapies in order to eradicate bone infection. Several adjunct treatments will be discussed including, super-oxidized solution, granulocyte colony-stimulating factor and antibiotic composites.
In addition to antibiotics and surgical debridement, the use of an antiseptic agent such as a stable super-oxidized solution (SOS) has been proposed to aid in treatment of osteomyelitis in diabetic foot infections. The use of antiseptics in tissue infections has historically been controversial due to sparse evidence available to support effective antibacterial activity, and reports of a few formulations which actually caused native tissue damage [66]. However, in 1996 Yahagi et al. looked at SOS, a new formulation of antiseptic, which was effective against bacteria but not on eukaryotic cells [67]. One limitation of Yahagi’s research was that most of the solutions available were short acting making broad clinical application difficult [68]. Dermacyn wound care (DWC; Oculus Innovative Sciences, Petaluma, CA) subsequently appeared on the market as the first reported SOS that is stable at room temperature for up to 1 year [69]. Aragon-Sanchez et al. evaluated 14 patients who underwent conservative surgery for DFO, in whom clean bone margins could not be assured and had histopathologic confirmed osteomyelitis [70]. Intraoperatively, each patient received copious irrigation with DWC as well as daily irrigation with DWC either through a catheter inserted in the surgical cavity, between sutures, or via placing gauzes soaked with DWC over the open wound. All patients also received culture-directed antibiotic therapy. There were no reported side effects of the treatment and 100 % limb salvage was achieved in treated patient over an average healing period of 6.8 weeks. Later in 2010, Piaggesi et al. published a randomized controlled trial evaluating the safety and efficacy of DWC [71]. Forty patients with postsurgical lesions which were left open to heal by secondary intention were randomized into two groups: A, locally treated with DWC and B, povidone iodine as local medication. Both groups received systemic antibiotic therapy and surgical debridement if needed. Patients were then followed weekly for 6 months. At the conclusion of their study, healing rates were significantly shorter in group A (90 %) than in group B (55 %; p < 0.01). Time taken for cultures to become negative and duration of antibiotic therapy were also significantly shorter in group A than in group B. The number of interventions were also significantly higher in group B (p < .05) as well as reinfections (p < 0.01). Based on current evidence, SOS antiseptics appear to be a safe and effective adjuvant to surgical debridement and antibiotic therapy creating an unfavorable environment for bacteria and assisting with accelerated wound healing. Nevertheless, additional research for their specific use in DFO is needed to completely understand their full therapeutic benefit and role in treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








