Fig. 13.1
Marking for incision for right Sportsmen’s groin repair. Arrow points to external ring when palpated through scrotal skin
A sharp incision is performed and electrocautery dissects down through the subcutaneous tissue and Scarpa’s fascia. The external inguinal ring is then identified. In some cases, edema or widening of the external ring is visible at this stage in the operation. The fibers of the external oblique are then carefully divided using care to maintain the integrity of the ilioinguinal nerve. Again, some edema can be encountered at this part of the operation. The spermatic cord and the spermatic vessels should then be identified and evaluated for a possible indirect hernia sac or other abnormality. The spermatic cord and vessels are then circumscribed with a quarter-inch Penrose drain and retracted either inferior-laterally or superior-medially. This will allow a good view of the floor of the inguinal canal and transversalis fascia (Fig. 13.2a, b).
Fig. 13.2
(a) Exposure of floor of inguinal canal. Arrow points to lateral border of rectus muscle. (Published with kind permission of © Ulrike Muschaweck 2013. All Rights Reserved.) (b) Intraoperative view of inguinal canal
At this point, maintaining a bloodless field is paramount. Valsalva maneuver performed directly by the patient (when under local anesthesia) or indirectly by pressing on the abdomen can often delineate the “bulge” in the floor which Muschaweck describes. Careful evaluation for the genital branch of the genital-femoral nerve in this area can then be performed.
There may be some increased vascularity as well as edema in the floor of the canal. If no other relevant pathology is found, the Muschaweck minimally invasive repair can be performed. The transversalis fascia is incised only along the weakened fibers of the bulge. This incision is carried from lateral border of the bulging area medically to include the whole of the area of weakness, using care to avoid venous structures immediately deep to it (Fig. 13.3a, b). The region which has been opened is then closed in a tension free method.
Fig. 13.3
(a) Marking of the “bulge” in the transversalis fascia. (b) Incising the “bulge” in the transversalis fascia. From Minnich J et al. Sports hernia: diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med 2011 Jun;39(6):1341–9. doi:10.1177/0363546511402807. Epub 2011 Apr 19. (b) (Published with kind permission of © Ulrike Muschaweck 2013. All Rights Reserved)
With a running suture in the area of the defect of the transverse fascia, a free fascia flap from the iliopubic tract is sutured to the edge of the upper transverse fascia. This creates another fascia flap for the return suture. The running suture is continued to the lateral edge of the rectus muscle. Then the free flap is incorporated in the running suture laterally to initial knot.
A 2–0 polypropylene suture is run along the length of the opening and a second layer of suture imbricates the tissue on itself (Fig. 13.4). This plicating suture tightens the floor of the inguinal canal. The suture starts in the medial part of the defect, going to the internal ring, taking the free upper fascia flap. The suture line is then anchored to the lateral edge of the rectus muscle. The suture is then run laterally to finish the closure (Fig. 13.5). A crucial aspect of the medial suture line is an anchoring stitch to the lateral border of the rectus muscle (Fig. 13.6).
Fig. 13.4
(a) Closing the defect with a running imbricating suture 2–0 Prolene. (Published with kind permission of © Ulrike Muschaweck 2013. All Rights Reserved.) (b) Operative view of closure
Fig. 13.5
Closing the defect with an imbricating suture. (Published with kind permission of © Ulrike Muschaweck 2013. All Rights Reserved)
Fig. 13.6
A small tail of tissue is taken from the internal oblique muscle to cover the ilioinguinal nerve. From Minnich J et al. Sports hernia: diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med 2011 Jun;39(6):1341–9. doi:10.1177/0363546511402807. Epub 2011 Apr 19. (Published with kind permission of © Ulrike Muschaweck 2013. All Rights Reserved)
Upon completion of this running suture, the bulging area is completely obliterated. Again, careful evaluation of the genital branch of the genitofemoral nerve in this area is performed. If this appears to be fibrotic or involved in the area of inflammation, it is sacrificed and excised. If it is not found, it is likely due to its coursing more superiorly and not in the area of exploration.
The final aspect of the repair incorporates a muscular collar to protect the ilioinguinal nerve from further mechanical irritation. This is created from the muscular part of the internal oblique muscle at the level of the internal ring (Fig. 13.7). This is done to protect an intact ilioinguinal nerve from postoperative irritation or inflammation.
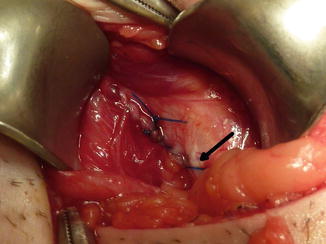
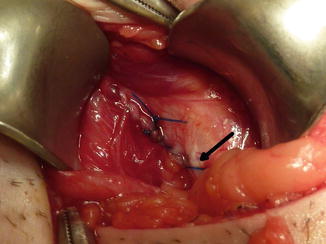
Fig. 13.7
The completed imbricated suture line. Arrow points to the medial aspect of the suture line which is anchored to the lateral border of the rectus muscle. From Minnich J et al. Sports hernia: diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med 2011 Jun;39(6):1341–9. doi:10.1177/0363546511402807. Epub 2011 Apr 19
Local anesthesia is then infiltrated to the depths of the wound and around the pubic tubercle. We use 20 ml Ropivacain 7.5 mg/ml. Because the patients are typically thin and athletic, care must be taken not to instill the anesthetic directly into the femoral nerve. This can lead to a temporary, but distressing, proximal leg weakness postoperatively.
The spermatic cord and vessels are then placed back in their normal anatomic position in the floor of the canal. We loosely reapproximate the external oblique over the spermatic cord using care to maintain the integrity of the ilioinguinal nerve. Individual 3–0 absorbable suture is used for this purpose. Scarpa’s fascia is closed with running suture of 3–0 absorbable suture and the skin is reapproximated using a 4–0 absorbable subcuticular suture. Sterile dressings are placed.
Post-surgical Repair Rehabilitation
It is important to emphasize to the athlete that postoperative rehabilitation contributes to the overall success of surgery. The patient should undergo a stepwise progression of exercises and activities focusing on core abdominal and lower extremity strength stability, flexibility, and balance exercises. Associated adductor weakness or tightness should also be specifically addressed by aggressive pre- and post-activity stretching.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







