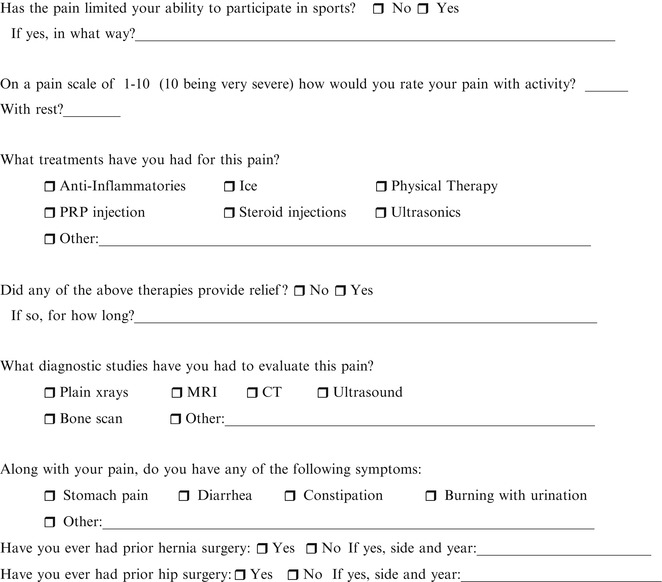
Fig. 11.1
Athletic groin history patient information form used at the Washington University School of Medicine
The physical exam should be comprehensive and include a careful abdominal exam, assessment for inguinal hernia (and in females, femoral hernia), and testicular exam in males with palpation through the external inguinal ring to assess for a bulge and laxity in the ring. Assessment of the pubic symphysis for tenderness and pubic instability is done as well. The examiner should palpate for tenderness in the medial inguinal floor/distal rectus insertion both with the athlete supine and during a sit-up (Fig. 11.2). Tenderness limited to this area is an important positive finding that supports the diagnosis of a sports hernia type injury. Oblique testing with resistance is also done (Fig. 11.3). Lower extremity muscle strength is assessed for hip flexors both with straight leg raising and hip flexion and adduction with and without resistance with the leg both extended and in a frog leg position. Movements that trigger pain are noted. The upper adductor longus tendon and any other areas of pain should be palpated directly. Finally, a hip exam should be done to rule out a hip etiology as has been described previously.



Fig. 11.2
Inguinal floor and distal recuts palpation during a sit-up. Tenderness at this site with either the athlete supine or during a sit-up is one of the signs consistent that can be associated with a sports hernia pubalgia diagnosis

Fig. 11.3
Abdominal oblique testing. The patient rotates their shoulder toward the opposite iliac crest against resistance
The preferred imaging modality by this author is a pelvic MRI under “pubalgia protocol” sequences (see Chap. 8) using a multi-coil pelvic array coil centered over the lower pelvis. MRI sequences obtained under this protocol include coronal T1 and STIR (short T1 inversion recovery) sequences, transverse T1 and T2 with fat suppression, and sagittal high resolution 3 mm thick sequences through the pubic bones and symphysis. If an adductor problem is suspected, then oblique transverse T2 sequences with fat suppression are included. Findings on MRI that support a diagnosis of an athletic pubalgia type injury include a tear in the distal rectus abdominus aponeurosis insertion at the pubis, parasymphyseal edema, a secondary cleft, and combined rectus-adductor aponeurosis tear. These findings have been described in detail in Chap. 7.
The criteria for operation for suspected athletic pubalgia injuries include a combination of lower abdominal/inguinal pain that limits athletic performance, failure to resolve with 6–8 weeks of conservative management, and exclusion of other diagnoses (e.g., hip pathology) as a primary source of the pain. In some cases, an athletic pubalgia type injury and hip pathology (labral tear, impingement) may co-exist, in which case a discussion between the orthopedist and general surgeon should ensue to determine which repair should be undertaken first. Supporting evidence for a pubalgia injury should be present from the MRI, although the absence of such findings does not necessarily preclude proceeding with surgical repair if the symptoms and exam are consistent with the diagnosis and extended conservative treatments and rest have failed.
Role of Mesh in Inguinal Hernia Repair
In the early 1990s tension-free approaches to inguinal hernia repair began to replace primary tissue repairs. The principal reason for this shift was that primary sutured repairs were often associated with tension on the suture line and, consequently, a high recurrence rate and increased postoperative pain [4]. In addition, the use of a tension-free mesh approach allowed patients to resume physical activities and labor much sooner than after a sutured repair [5]. In 2003 it was estimated that 93 % of inguinal hernia repairs utilized mesh, and the Lichtenstein method was the most common approach done [6]. Since primary tissue repairs are infrequently performed now in most surgical training programs, the current generation of surgeons has little if any experience with these techniques in surgical practice. Moreover, the unique aspects of the primary repairs done in athletes by advocates of these approaches differ from standard Bassini and other conventional primary repairs and have not been taught or disseminated into the mainstream surgical community.
A variety of meshes have been used for inguinal hernia repair that include heavyweight bilayer mesh, lightweight polypropylene mesh, and polytetrafluoroethylene (PTFE) or Goretex mesh (W. L. Gore Associates, Newark, DE). Lightweight meshes have generally been preferred in this location because of ease of use, low cost and because they have been associated with less pain, stiffness, and foreign body sensation in the inguinal floor compared to heavyweight meshes [7]. Inguinal floor repair and stabilization using an open mesh technique can be achieved in athletes that are appropriately selected for operation.
Operative Technique
The preferred approach that the author has taken to repair of the inguinal floor for athletes with a sport’s hernia pubalgia has been a lightweight tension-free mesh repair. While this approach is taken for the reasons outlined above, there are circumstances in which the use of an open mesh approach may not be appropriate or preferred. Young athletes who have not completed their growth cycle and particularly young females are better served by one of the open primary tissue repairs as have been described elsewhere (see Chaps. 10 and 13). In addition, for athletes who have had a prior open inguinal hernia surgery or even in some cases a prior failed “sport’s hernia” repair, the author has used a laparoscopic preperitoneal mesh repair as described in Chap. 12.
The operative approach for the open tension-free mesh repair utilizes a slightly oblique incision placed over the inguinal canal as for a standard inguinal hernia repair. This approach is most commonly done under local anesthesia with sedation unless an accompanying adductor procedure is done, in which case general anesthesia is typically used. A mixture of 1 % lidocaine and 0.5 % bupivacaine local anesthetic are injected into each successive layer as the dissection proceeds.
One of the typical operative findings is a markedly attenuated external oblique aponeurosis (Fig. 11.4). The external oblique is opened widely through the external ring and the cord structures are encircled. A search is made for the ilioinguinal nerve which is left within its sheath. The base of the cord is opened to search for an indirect hernia sac which is rarely present. The inguinal floor is often markedly attenuated and even bulging in some cases as shown in Fig. 11.5. The floor is reconstructed by suturing a lightweight polypropylene mesh to the transversalis aponeurosis and rectus sheath medially (Fig. 11.6) using interrupted nonabsorbable 0-nylon suture. The lateral side of the mesh is then sutured to the inguinal ligament with a 2–0 running polypropylene suture, and the mesh is split and the two ends are brought together and sutured to the inguinal ligament. The tails of the mesh are sutured to the inguinal ligament and around the cord in effect reconstructing the internal ring not because the pathology is at the internal ring, but in order for the mesh to lie smoothly and evenly across the floor and provide the support needed to take the tension off the rectus and the pubis (Fig. 11.7).
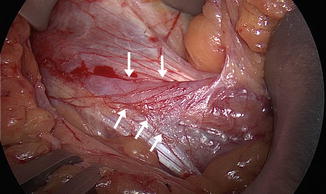
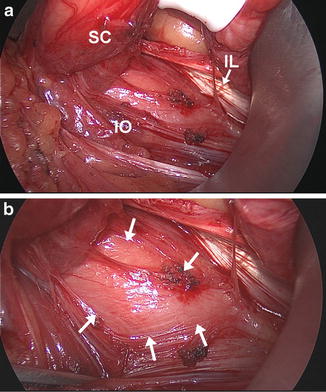
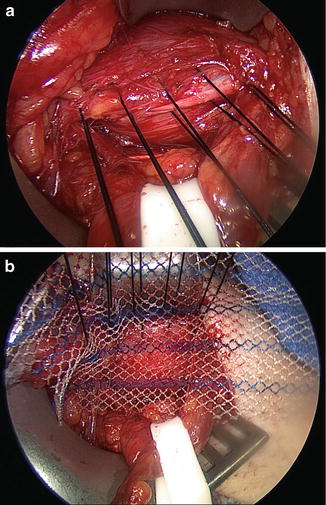
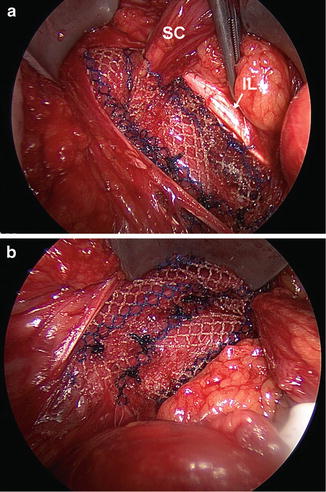
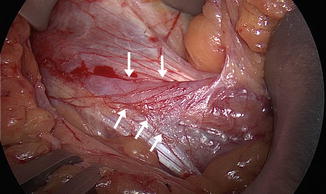
Fig. 11.4
Attenuated external oblique aponeurosis in an athlete undergoing sports hernia repair
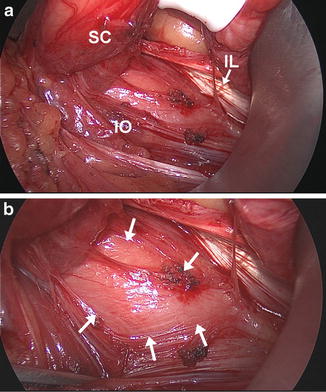
Fig. 11.5
Weak and bulging posterior inguinal floor seen during a left sided sports hernia pubalgia repair. (a) IO internal oblique, IL inguinal ligament, SC spermatic cord; (b) close up view. Arrows outline area of floor weakness
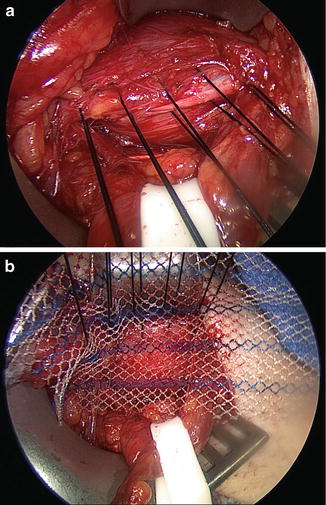
Fig. 11.6
Sutures used to anchor the mesh to the medial transversalis aponeurosis and rectus sheath. (a) Interrupted suture placement in the transversalis aponeurosis; (b) sutures through the aponeurosis and lightweight polypropylene mesh
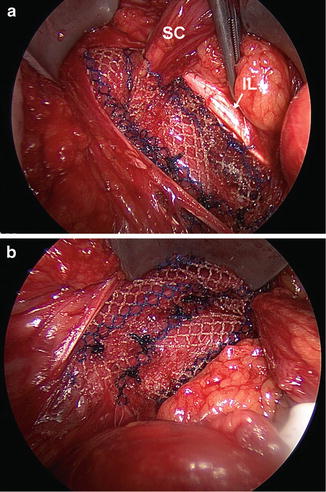
Fig. 11.7
Completed mesh repair. (a) Shown is the mesh anchored to the inguinal ligament (IL) laterally and the split limbs of the mesh sewn to the inguinal ligament above the internal ring; (b) medial side of the repair
Other tension-free mesh approaches have also been used including bilayer polypropylene mesh [8] and PTFE materials [9]. Biologic mesh has also been used but via a laparoscopic approach [10] and is considerably more expensive and lacking in reported outcomes. Brown and colleagues [9, 11] in Montreal use a PTFE patch that is anchored to the external oblique aponeurosis using interrupted polypropylene sutures to repair the torn margins of the external oblique fascia. The external oblique is then closed loosely over the patch.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







