Surgical Treatment of Posterolateral Corner Injuries
Bryan T. Hanypsiak MD
Richard D. Parker MD
Historical Review
The history of the posterolateral corner (PLC) can be traced back to 1884.1 The lateral collateral ligament (LCL) was identified and labeled as the “external lateral ligament,” an extension of the peroneus longus. The work of defining and updating the anatomy of the posterolateral corner, however, did not begin in earnest until the late 1950s.2,3,4
It was, however, only after unrecognized injuries to the posterolateral corner were associated with the early failure of cruciate reconstructions that these injuries gained clinical significance.5,6,7,8,9,10,11 In 1994 Veltri and Warren12 determined that the LCL, popliteus, and popliteofibular ligament (PFL) were the major contributors to the stability of the posterolateral corner. It is these structures that must be addressed by surgeons seeking a successful anatomic reconstruction of the posterolateral corner.
Despite our increased understanding of the pathomechanics of the posterolateral corner, the diagnosis and treatment of these injuries has remained difficult. Posterolateral corner tears, which frequently occur in combination with injuries to other ligamentous structures,13 are often undiagnosed, misdiagnosed, or untreated on initial presentation.8 The orthopedic surgeon, therefore, must be prepared to diagnose and treat patients who present with chronic posterolateral corner injuries.
This chapter will address the relevant anatomy, history, physical examination, and repair or reconstructive technique of both acute and chronic posterolateral corner tears.
Indications and Contraindications
Understanding the anatomy of the posterolateral corner and clearly defining the injured structures are the keys to performing a successful repair or reconstruction. The anatomy of the posterolateral corner is complex. The terminology used in the literature is not universal, and with many authors using multiple names for the same structures, it is, at best, confusing. To add to the challenge, the ligaments involved are difficult to identify intraoperatively, and many are not present in all individuals.
An example of the significant anatomic variability of the key elements of the posterolateral corner, the arcuate ligament, and fabellofibular ligaments are both present in only 67% of patients.14 The fabellofibular ligament is present alone in 20% of patients, while the arcuate ligament occurs alone in the remaining 13%. The presence or absence of the fabella on radiographs offers a hint to the anatomic configuration present. An absent fabella suggests an absent fabellofibular ligament, while a large fabella suggests an absent arcuate ligament.15
In preparing for a repair or reconstruction of the posterolateral corner, its complex anatomy warrants a brief review of the key components and their function as it relates to the our preferred technique.
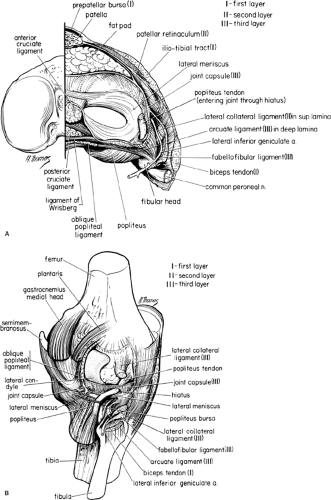
In 1982 Seebacher et al.15 divided the lateral structures of the knee into three layers. Layer I is composed of the iliotibial tract and the superficial biceps femoris. Layer II contains the quadriceps retinaculum anteriorly and patellofemoral ligaments posteriorly. Finally, layer III is made up by the lateral aspect of the capsule, coronary ligament, popliteus, LCL, and the fabellofibular and arcuate ligaments (Fig. 48-1A,B). The anatomy of the posterolateral corner is best understood when organized and reviewed by layer.
Posterolateral Corner Anatomy
Layer I
Iliotibial Band
The iliotibial band (ITB) runs from the femoral supracondylar tubercle to Gerdy’s tubercle of the tibia. The ITB acts as an accessory LCL and is a critical lateral compartment stabilizer. Clinically, it is the ITB that reduces a posteriorly subluxed tibia when a reverse pivot shift test is performed.
In flexion, the ITB externally rotates the tibia and pulls it posteriorly. Because the ITB moves anteriorly with extension, it is often spared in posterolateral corner injuries that result from a varus load to the knee.
Biceps Femoris Tendon
Divided into a short and long heads, the biceps runs posterior to the ITB and inserts primarily on the fibular styloid. A strong lateral stabilizer of the knee, the biceps also acts as an external rotator of the tibia in conjunction with the ITB.16 Unlike the ITB, the biceps is frequently torn in posterolateral corner injuries, eliminating surgical options that describe its use as part of the reconstruction.
Layer II
Both the patellar and quadriceps retinaculum lie anterior to the midline of the knee and play little role in the stability of the posterolateral corner.
Layer III
Lateral Collateral Ligament
The LCL reinforces the posterior third of the joint capsule and is the most important stabilizer of the knee to varus stress. It is dynamically controlled by its attachments to the biceps femoris and acts secondarily to limit external rotation. Isolated injuries to the LCL are uncommon.
Popliteus
The popliteus originates from the posterior tibia, passes through a hole in the coronary ligament, attaches to the lateral meniscus, and inserts on the lateral femoral condyle. It is a dynamic and static stabilizer of the tibia on the femur, a weak knee flexor, and serves as reinforcement to the posterior third of the capsule. The popliteus unlocks the extended knee by rotating the femur on a fixed tibia, or equivalently, by internally rotating the tibia around a fixed femur. The popliteus acts to restrict posterior translation and external and varus rotation of the knee. Injuries to the popliteus cannot occur without weakening the surrounding structures.14,17
Popliteofibular Ligament
Present in 91% of cadaveric specimens,18 the PFL runs from the anterior aspect of the lateral femoral condyle to the posterior aspect of the fibular head. Its anterior and posterior divisions give it the anatomic appearance of an inverted Y.18,19 It provides a direct static attachment of the femur to the tibia and shares the resistance to posterior tibial translation and external and varus rotation.
Arcuate Ligament
It is important to differentiate in the arcuate complex, which Hughston et al.20 defined as the LCL, arcuate ligament, popliteus muscle and tendon, and the lateral gastrocnemius muscle, from the arcuate ligament,13,21 a confluence of capsular structures connecting the lateral femoral condyle to the fibular styloid process. When present, it is always posterior to the fabellofibular ligament and may be indistinguishable from it. The arcuate ligament has been divided into medial and lateral limbs with varying attachments, both limbs act as capsular reinforcements.
Fabellofibular Ligament
The fabellofibular ligament is the distal termination of the capsular arm of the short head of the biceps. It runs between the fabella, an osseous or cartilaginous sesamoid structure in the tendon of the lateral gastrocnemius muscle, and the lateral tip of the fibular styloid, medial to the direct arm of the short head of the biceps femoris. The fabellofibular ligament becomes tight in extension and serves as a capsular reinforcement.
Other Structures
Several other structures act to increase the overall stability of the lateral side of the knee. The lateral meniscus increases the concavity of the tibial plateau; the coronary ligament is a capsular attachment to the outer edge of the lateral meniscus; and the lateral gastrocnemius tendon blends with the arcuate ligament, a lateral capsular thickening. Finally, the popliteomeniscal fascicles connect the inferior surface of the lateral meniscus to the articular cartilage border of the lateral tibial plateau.
Biomechanical Analysis
In an effort to identify an ideal reconstruction, a number of biomechanical studies were undertaken to define the significance of each discrete anatomic structure.22,23,24,25,26,27 Through a series of selective sectionings, the exact contribution of each component of the posterolateral corner has been defined, and the major contributors to posterolateral stability have been identified. Only recently has there been a consensus among authors.
An intact posterolateral corner reduces anteroposterior (AP) translation of the tibia in extension and decreases external and varus rotation forces across the cruciates. The increased loads experienced by grafts placed in a PLC deficient knee led to early failure of both anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL)
reconstructions.5,6,7,8,9,10,11 The following is a brief summary of the role of the PLC in controlling force across the knee:
reconstructions.5,6,7,8,9,10,11 The following is a brief summary of the role of the PLC in controlling force across the knee:
AP translation is restrained by a dynamic interplay between the PCL and PLC. The role of the PLC in stabilizing posterior translation of the tibia decreases as knee flexion increases. Beyond 90 degrees of flexion, the PLC becomes lax and the PCL becomes primarily responsible for controlling posterior translation of the tibia on the femur. Several studies have demonstrated that sectioning of the PLC increases posterior translation of the lateral tibial plateau at 30 degrees, but less so at 90 degrees.14,28,29 Cutting both the PCL and PLC increases the translation of both the medial and lateral tibial plateaus at all flexion angles. To summarize, the PLC is primarily responsible for limiting tibial translation in extension, while the PCL is primarily responsible for limiting translation in flexion.
Varus rotation is restrained by the LCL and secondarily by the popliteus. Sectioning of the LCL results in increased varus rotation from 0 degrees to 30 degrees. Maximum displacement occurs at 30 degrees with an intact PCL.29 Sectioning both the LCL and PCL increases varus rotation at all angles of flexion, with the maximum displacement occurring at 60 degrees.12,29 In summary, the PLC is predominantly responsible for controlling varus rotation near full extension, whereas the PCL has its greatest effect in flexion.
External rotation is restrained by the posterior joint capsule, popliteus, PFL, and secondarily by the LCL. Sectioning of these components of the posterolateral corner leads to increased external rotation in extension. The maximum effect occurs at 30 degrees, the minimum at 90 degrees. Combined cutting of both the PLC and PCL leads to increased external rotation in all flexion angles, with the maximum effect at 90 degrees.12,29 Sectioning the PCL alone has no effect on external rotation at any flexion angle. Again, based on biomechanical studies, the posterolateral corner has its greatest effect near full extension, while the PCL provides secondary stabilization to external rotation in flexion.
Finally, intra-articular pressure in all three compartments is increased by combined sectioning of the PCL and PLC.30 This may form the basis for the development of early osteoarthritis in patients with chronic deficiencies.
Patient History
Patients with an acute or chronically deficient posterolateral corner will often complain of lateral or posterolateral joint pain, difficulty with stairs, ramps, or cutting activities, and a sense of instability with knee extension, such as during the toe off phase of gait. Periodically, a foot drop is associated and may be either transient or permanent. Forty percent of these injuries occur as a result of a sports injury. The most common mechanism is a posterolateral blow to the anteromedial knee in extension or a hyperextension injury with a varus and rotatory force. Both contact and noncontact injuries have been described. Less commonly, a varus load to a flexed knee may result in an injury to the posterolateral corner.31
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree