Surgical Technique of Proximal Tibia Megaprosthesis
Mario Mercuri
Costantino Errani
The proximal tibia is the second most common site involved with primary tumors of the skeleton. En bloc resection is a limb-sparing option for low-grade and most high-grade bone sarcomas, for selected cases of stage 3 benign tumors (e.g., giant cell tumor), and occasionally for metastatic lesions. Surgical options for reconstruction include megaprosthesis, osteoarticular allograft, allograft-prosthesis composite, and rotationplasty. Modular prosthetic replacement is a relatively simple technique and has become the method of choice for reconstruction after bone tumor resection at the proximal tibia. However, the long-term survival of megaprostheses is poor; mechanical failure and infection remain the major problems. A gastrocnemius transposition flap is necessary to obtain soft tissue coverage and reconstruction of the extensor mechanism to reduce risk of infection and rupture of the patella tendon (1).
Resection for lesions of the proximal tibia can be classified into intra-articular and extra-articular. If the tumor does not involve the joint, an intra-articular resection is indicated; otherwise, an extra-articular resection can be performed (2).
INDICATIONS
All patients with tibial sarcomas should be considered potential candidates for limb-sparing procedures.
Indications for endoprostheses depend on age, site, type of resection, life expectancy, and the patient’s functional demands.
This reconstruction technique is indicated in adult patients and adolescents at the end of growth.
Expandable prostheses can be used in pediatric age (7 to 12 years) and may be lengthened over time, thus correcting limb-length discrepancy (3).
CONTRAINDICATIONS
Contraindications to resection include pathologic fractures, neurovascular involvement, contamination from a poorly performed biopsy, and local sepsis.
When a limb-sparing procedure is possible, endoprostheses are not indicated in patients under 7 years old (4).
PREOPERATIVE PLANNING
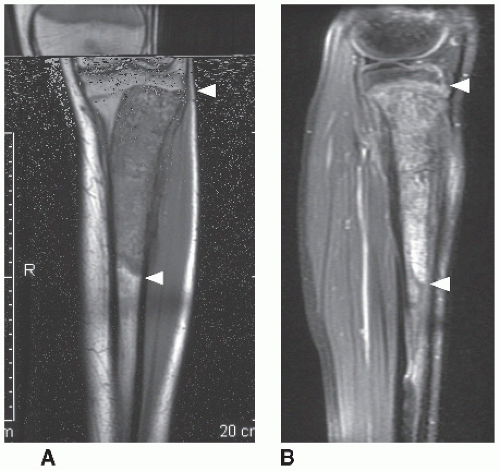
Resection of proximal tibia requires the careful analysis of the preoperative staging studies. An accurate preoperative staging of the tumor by plain film radiographs, computed tomography (CT), magnetic resonance, and bone scintigraphy is mandatory before surgery to determine resectability by evaluating the exact extent of the lesion and its relationship to neurovascular bundles (Figs. 20.1, 20.2, 20.3).
 FIGURE 20.1 A,B: Typical radiograph picture of osteosarcoma of the left proximal tibia in a boy aged 15 years (arrowheads). |
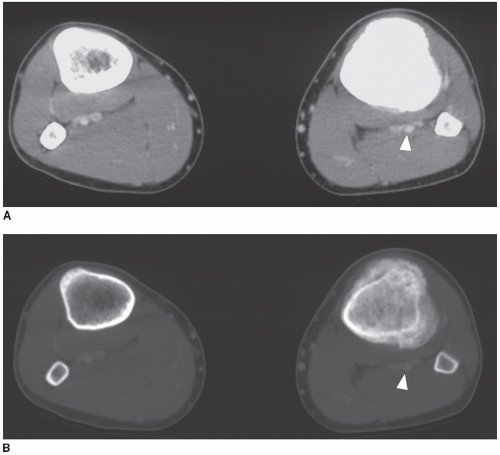 FIGURE 20.2 A,B: Axial CT scan for bone and soft tissue of the left proximal tibia show a relationship between tumor and neurovascular bundles (arrowheads). |
THE TECHNIQUE
Surgeons must meticulously follow the principles of oncologic surgery: the tumor must be removed en bloc with noncontaminated surgical margins (wide-margin resection).
Position and Draping
The patient is placed supine on the operating table and the entire extremity is prepared and draped. A bloodless field should be obtained with a tourniquet after exsanguination by gravity; however, it is important not to squeeze or manipulate the lesion using elastic wrappings when preparing the patient. The tourniquet must be removed after excision of the lesion but before closing the tissue planes.
Incision and Dissection
An anteromedial longitudinal incision is used just proximal to the superior pole of the patella to the distal third of the tibia, including the previous biopsy incision with a 1 cm border between the biopsy scar and the resection incision (Fig. 20.4). The procedure begins by making an arthrotomy to inspect the joint. If the joint fluid is normal and no tumor can be seen within the joint, an intra-articular resection can be continued. If intraarticular tumor involvement is suspected, the capsule should be closed and an extra-articular resection must be performed. Popliteal vessels are identified by detaching the medial gastrocnemius muscle and splitting the soleus muscle (Fig. 20.5). The soleus must be released from its origin on the proximal tibia just distal to the lower border of the popliteus. It is necessary to leave some soleus on the tibia as a soft tissue margin and to pay
attention to the posterior tibial nerve and vessels that are just deep to the soleus. The anterior tibial vessels are branches from the posterior vessels and enter the anterior compartment at the inferior border of the popliteus muscle. If the anterior tibial artery is adjacent to the tumor, it should be ligated at its origin in the posterior compartment (Fig. 20.6). Therefore, the posterior neurovascular bundle should be visualized from the knee joint to as far distally as needed to perform the tibial osteotomy (Fig. 20.7). The popliteal muscle is always sacrificed; patella tendon must be transected from the tibial insertion as far as possible avoiding contamination (Fig. 20.8). The capsule of the knee joint can be sectioned close to the femoral insertion and leaving the menisci
with the proximal tibia tendon. The medial and lateral collateral ligaments and the cruciate ligaments, which pull the tibia anteriorly on the femur, are divided close to the femoral insertion (Fig. 20.9



attention to the posterior tibial nerve and vessels that are just deep to the soleus. The anterior tibial vessels are branches from the posterior vessels and enter the anterior compartment at the inferior border of the popliteus muscle. If the anterior tibial artery is adjacent to the tumor, it should be ligated at its origin in the posterior compartment (Fig. 20.6). Therefore, the posterior neurovascular bundle should be visualized from the knee joint to as far distally as needed to perform the tibial osteotomy (Fig. 20.7). The popliteal muscle is always sacrificed; patella tendon must be transected from the tibial insertion as far as possible avoiding contamination (Fig. 20.8). The capsule of the knee joint can be sectioned close to the femoral insertion and leaving the menisci
with the proximal tibia tendon. The medial and lateral collateral ligaments and the cruciate ligaments, which pull the tibia anteriorly on the femur, are divided close to the femoral insertion (Fig. 20.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree