Surgical Procedures of the Hallux
Albert E. Burns
HALLUX OSTEOTOMIES
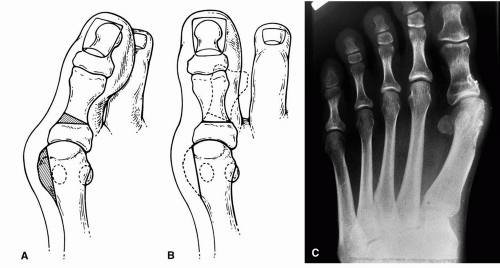
Osteotomy of the hallux for the correction of hallux abducto valgus was first proposed by Akin in 1925 (1). The original procedure included resection of the medial eminence of the first metatarsal head, resection of the proximal medial base of the proximal phalanx, and cuneiform osteotomy of the phalanx (Fig. 1). No specific criteria were provided for use of the procedure. Experience has shown that this is not a primary procedure to be used for the repair of hallux abducto valgus deformity because the hallux osteotomy does not directly address an increased intermetatarsal angle or proximal articular set angle (PASA) (2,3).
More important, the inappropriate use of the classic Akin procedure for the repair of hallux abducto valgus deformity may result in further lateral displacement of the first metatarsophalangeal joint and recurrence of the deformity (2, 3, 4, 5, 6, 7). Although the clinical alignment of the hallux may appear improved, if a significant increase in the intermetatarsal angle or PASA is not addressed, then the functional center of the first metatarsophalangeal joint will be lateral to the midline of the first ray. In the presence of this structural and musculotendinous imbalance, one may anticipate an even greater lateral subluxation or luxation of the first metatarsophalangeal joint that leads to a rapid recurrence of the original condition (Fig. 2).
Therefore, the Akin osteotomy is considered an adjunctive procedure that is usually performed concomitantly with a first metatarsal osteotomy and, occasionally, with a tendoncapsule balancing hallux valgus repair. Clinical experience has shown that this is a useful technique for straightening the hallux. Some surgeons may employ the procedure to realign the long flexor and extensor tendons into a more central location over the hallux and first metatarsophalangeal joint. Theoretically, this would reduce the retrograde forces that may otherwise tend to result in further lateral stress at the first metatarsophalangeal joint. However, if the intermetatarsal angle is reduced and joint congruity is restored, then it appears that the additional Akin osteotomy would have a negligible effect.
Evaluating the need for an Akin osteotomy may best be performed intraoperatively once the primary surgical procedures have been completed. Should lateral deviation of the hallux persist in spite of a congruous joint and reduction of more proximal structural deformities, then one must consider that further deformity persists within the hallux itself (2,3,8). Most commonly, this condition is a result of a hallux abductus interphalangeus or an increased distal articular set angle (DASA). It may be further appreciated when the medial side of the proximal phalanx is longer than the lateral side. Although capital osteotomies are classically indicated for the correction of PASA deformities, in some patients osteotomy in the first metatarsal head may be impeded by bone cysts, iatrogenic deformity, or the need to perform multiple procedures. In this instance, an Akin procedure may be used to assist in compensating for the PASA. Although it is not at the apex of the deformity, the hallux osteotomy may be close enough to provide a satisfactory clinical and functional result (2).
Dissection
The surgical approach used most often for an Akin procedure is a dorsomedial linear incision, which may be an extension of the dorsomedial incision used for the bunionectomy. A medial longitudinal incision at the juncture of the dorsal and plantar skin is also a popular approach. Other modifications of the incisional approach may be employed to facilitate exposure and to create better wound relaxation. Two others include a serpentine incision at the hallux interphalangeal joint and the addition of a transverse segment to the dorsomedial linear incision over the interphalangeal joint simply to create an L-shaped configuration (9) (Fig. 3). To some degree, the incision selection may be based on the type of osteotomy to be performed and the fixation that the surgeon anticipates will be required to stabilize the bone adequately for optimal healing.
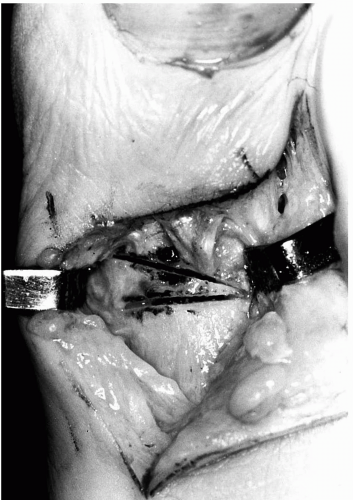
Sharp and blunt dissection techniques are used to continue the dissection through the superficial fascia, with care taken
to avoid the dorsomedial and lateral neurovascular structures. Once the deep fascia or extensor hood fibers are identified, then separation of the superficial fascia is extended medially and laterally to provide a clear definition of the deep fascia and periosteum over the proximal phalanx. At this stage, several different methods may be employed for the additional steps in the dissection process. The deep fascia and periosteum may be incised linearly just medial to the extensor tendon. Dissection is usually facilitated by a Freer elevator, except at the metaphyseal area of the phalanx,
where a scalpel is typically required because of the adherence of ligamentous and capsular fibers.
to avoid the dorsomedial and lateral neurovascular structures. Once the deep fascia or extensor hood fibers are identified, then separation of the superficial fascia is extended medially and laterally to provide a clear definition of the deep fascia and periosteum over the proximal phalanx. At this stage, several different methods may be employed for the additional steps in the dissection process. The deep fascia and periosteum may be incised linearly just medial to the extensor tendon. Dissection is usually facilitated by a Freer elevator, except at the metaphyseal area of the phalanx,
where a scalpel is typically required because of the adherence of ligamentous and capsular fibers.
Alternatively, the periosteum may be incised transversely at the level of the anticipated osteotomy. In this manner, less periosteum needs to be reflected to perform the surgery, but additional freeing and retraction of the long extensor tendon are required. Although the traditional approach is to reflect the periosteum, this layer is thin at this level, and reflecting the tissue as one unit may be difficult. Therefore, one may elect to leave the periosteum intact during the osteotomy.
Proximal Akin Osteotomies
As commonly performed, the Akin osteotomy is a medially based transverse wedge resection located at the base of the proximal phalanx. Ideally, the cuts are located in metaphyseal bone, where the bone is wider, the lateral cortical hinge is less likely to fracture, and the overall bone quality is superior. As a general guide, the osteotomy is located between 0.5 and 1.0 cm distal to the articular surface (7,10,11), with the specific distance influenced by the type of fixation to be employed. Typically, the lateral cortex is left intact to function as a hinge for rotation. This also imparts an added measure of stability to the osteotomy.
The axis of the osteotomy may be altered to achieve different forms of correction with the procedure. If the axis is perpendicular to the weight-bearing surface, then closure of the osteotomy will maintain the alignment of the phalanx in the weight-bearing plane. An axis that is tilted laterally may result in elevation of the distal portion of the bone as the osteotomy is closed. This feature may be advantageous in patients with some element of hallux limitus. Tilting the axis distally, while maintaining neutrality in the frontal plane, reduces valgus rotation of the hallux as the osteotomy is closed.
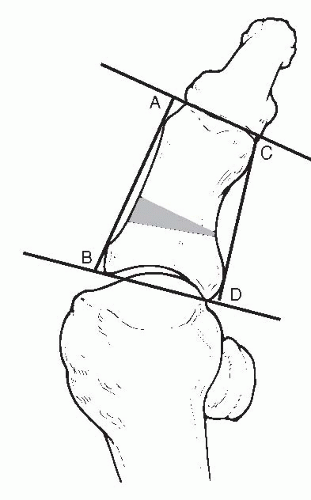
Numerous methods exist for determining the amount of bone that should be resected. As a general guideline, attempts are made to reduce the distal articular set angle to 0 degrees. Conceptually, enough wedge is being removed to make the two articular surfaces of the proximal phalanx parallel to each other. During a transverse type of osteotomy, the surgeons wants to orient the proximal cut so it is parallel to the joint surface. Then a better estimate may be derived regarding the amount of bone to resect when the distal cut is performed. Some investigators have suggested that constructing a preoperative template on the radiograph may be one way to estimate the amount of wedge necessary to achieve the desired correction (8). Another method is to measure the medial and lateral length of the proximal phalanx and to determine how much wedge removal is necessary, taking the base from the long side, to create a parallel relationship between the proximal and distal articular surfaces of the phalanx (12) (Fig. 4).
Distal Akin Osteotomies
Excessive abduction of the hallux may result from a primary deformity within the head of the proximal phalanx, the interphalangeal region, or a general asymmetry of the proximal phalanx. This last source of abductus is more common than a deviated DASA. In these patients, an osteotomy performed at the distal aspect of the phalanx, closer to the apex of maximum deformity, proves more effective in providing correction. Daw described an opening wedge osteotomy to correct the deformity at this level (13). However, most surgeons prefer to perform a closing wedge osteotomy at the distal metaphysis of the phalanx.
The distal Akin procedure may also be used to correct lateral deviation of the hallux arising proximally. Because the distal metaphysis of the proximal phalanx corresponds to the digital sulcus, adduction at this level provides a hallux that appears straight clinically, although radiographically the hallux may appear skewed (2) (Fig. 5).
On the other hand, some surgeons would argue that the end result of both the proximal and distal procedures is to realign the two articular surfaces of the proximal phalanx parallel to each other. For this reason, the proximal Akin procedure has been advocated for the correction of both an increased DASA and an increased hallux abductus interphalangeus (6,10,14,15). Although the proximal Akin procedure realigns the distal and proximal articular surfaces in the latter condition, it creates a slight Z shape of the proximal phalanx, which may not be as accurate in realigning the extensor and flexor tendons as a distal Akin procedure.
Performing a distal Akin osteotomy may offer some potential advantages over the proximal counterpart. The distal Akin procedure involves a shorter lever arm, which results in the transmission of less weight-bearing force across the osteotomy and is associated with less potential for disruption.
Performing the procedure at a more distant site from the metatarsophalangeal joint may also enhance the performance of range-of-motion exercises because there will be less tendency to disrupt the osteotomy at the more distal level with the application of this type of stress.
Performing the procedure at a more distant site from the metatarsophalangeal joint may also enhance the performance of range-of-motion exercises because there will be less tendency to disrupt the osteotomy at the more distal level with the application of this type of stress.
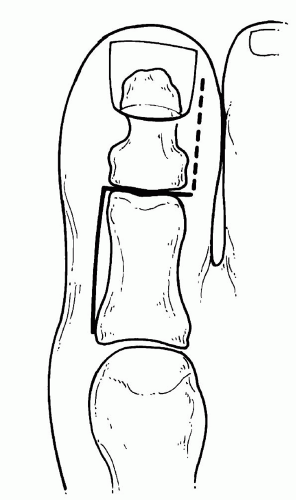
The prototypical procedure is a transverse wedge osteotomy in the distal metaphyseal bone 0.5 to 1.0 cm proximal to the hallux interphalangeal joint (Fig. 6). The wedge osteotomy has its apex laterally and its base medially, and the amount of bone to be removed may be determined using similar methods described for the proximal Akin osteotomy. Clinically, one may make the distal portion of the osteotomy parallel to the interphalangeal joint or to the proximal nail fold. The proximal cut may then be performed perpendicular to the long axis of the proximal phalanx. The axis guide concepts apply here also, and it is more common to use the axis guide to address any valgus rotation of the hallux at this level than with the proximal Akin osteotomy.
Modifications of the Akin Osteotomy
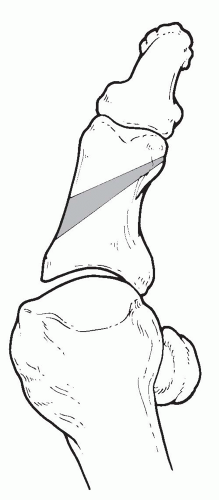
The main modification that has been described for the proximal Akin osteotomy is to perform the wedge resection in an oblique manner to use screw fixation (3,9). For a proximal Akin procedure, instead of placement of the osteotomy transversely, it is angled from proximal lateral to distal medial (Fig. 7). To provide adequate space for wedge removal and to accommodate screw fixation, the osteotomy usually traverses most of the length of the proximal phalanx. For this reason, some authorities have advocated this procedure for the correction of both an abnormal DASA and an abnormal hallux abductus interphalangeus (6,14, 15, 16). An axis guide pin may be used in the same fashion as a traditional
proximal Akin osteotomy. The distal Akin procedure may also be modified in an oblique fashion to facilitate screw fixation. The osteotomy is angled from distal lateral to proximal medial with the apex on the lateral side approximately 0.5 cm from the hallux interphalangeal joint (Fig. 8).
proximal Akin osteotomy. The distal Akin procedure may also be modified in an oblique fashion to facilitate screw fixation. The osteotomy is angled from distal lateral to proximal medial with the apex on the lateral side approximately 0.5 cm from the hallux interphalangeal joint (Fig. 8).
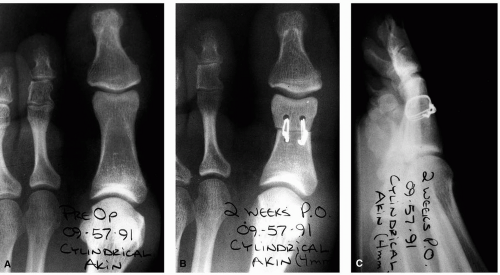
An excessively long hallux may be treated by removing a cylinder of bone from the proximal phalanx (3,6,8,17) (Fig. 9). When this is accomplished, it is referred to as a cylindric Akin procedure. This is most commonly used in patients with hallux limitus or when the hallux is so long relative to the adjacent digits that it creates a problem with shoe wear. Ideally, enough bone is removed so the hallux is of equal length or is slightly shorter than the second digit. Realignment of the articular surfaces of the proximal phalanx may be simultaneously accomplished by the removal of a trapezoidal wedge of bone. Alternatively, one may choose to use matching chevron osteotomies to perform the shortening. This technique provides locking segments that may enhance the overall stability of the procedure (Fig. 10A and B).
A shortening sagittal Z-osteotomy has also been described, particularly as an alternative to the enclavement procedure at the phalangeal base. Investigators proposed that shortening of an otherwise long hallux would tend to reduce excessive retrograde forces at the first metatarsal head and would thereby enhance motion. Screw fixation was used to stabilize the osteotomy (18) (Fig. 10C).
The complete transverse osteotomy without wedge or bone resection may also be employed to provide for derotation of significant deformity within the hallux. Because these types of procedures are complete through-and-through osteotomies, adequate fixation is important. Correction of valgus rotation of the hallux can also be accomplished by changing the direction of the axis guide of the hinge of the osteotomy
(19,20). The closer the axis guide of the hinge comes to lying within the transverse plane, the more frontal plane correction can be accomplished. By angulating the axis guide of the osteotomy hinge in the lateral cortex from dorsodistal to plantar proximal, the closure of the osteotomy will reduce the valgus rotation of the hallux. This technique results in both cosmetic and functional benefits. Derotation of the hallux may also be accomplished by sacrificing the lateral cortical hinge, aligning the hallux in the desired position, and applying two points of fixation.
(19,20). The closer the axis guide of the hinge comes to lying within the transverse plane, the more frontal plane correction can be accomplished. By angulating the axis guide of the osteotomy hinge in the lateral cortex from dorsodistal to plantar proximal, the closure of the osteotomy will reduce the valgus rotation of the hallux. This technique results in both cosmetic and functional benefits. Derotation of the hallux may also be accomplished by sacrificing the lateral cortical hinge, aligning the hallux in the desired position, and applying two points of fixation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree