Surgical Options for Recurrent Carpal Tunnel Syndrome
Loukia K. Papatheodorou
Dean G. Sotereanos
INTRODUCTION
Compression of the median nerve at the wrist, known as carpal tunnel syndrome, is the most common entrapment neuropathy in the upper extremity affecting 10% or more of the general population (1). Even though carpal tunnel surgical release is generally considered efficacious, recurrence of symptoms of carpal tunnel syndrome can occur in up to 30% of patients postoperatively (2,3,4). The persistence of symptoms of carpal tunnel syndrome is commonly associated with incomplete initial release of the transverse carpal ligament, whereas recurrence of symptoms, after a distinct symptom-free period, is usually secondary to cicatrix surrounding of the median nerve (2,5).
Treatment of recalcitrant carpal tunnel syndrome remains a challenging problem. Nonsurgical treatment (splinting, injection, nonsteroidal anti-inflammatory drugs) may temporarily alleviate pain but usually fails to provide a long-term relief of the symptoms. Revision surgery, repeated median nerve decompression, even with external or internal neurolysis, does not always lead to sufficient relief of symptoms. Secondary decompression can cause scar reformation of the median nerve with the surrounding tissue, developing further compression of the nerve, resulting in traction or adhesive neuritis (5).
To manage this complex problem and prevent further adhesion to the median nerve, several techniques including interposition flaps and adhesion barriers, biologic or synthetic, have been proposed to cover or wrap the nerve. These supplementary techniques include various soft-tissue interposition flaps and nerve wrapping (vein wrapping, nerve protectors). The optimal treatment may consist of a combination of procedures. The goal of treatment of recurrent carpal tunnel syndrome is to create an environment for scar-free healing of the neurolyzed nerve, preventing recurrent cicatrix, improving the gliding of the median nerve during wrist motion, and promoting the nerve functional recovery.
TISSUE INTERPOSITION FLAPS
A variety of tissue interposition flaps (fat, muscle, or free flaps) have been used to cover and provide neovascularization to the median nerve in revision carpal tunnel surgery. However, many of these flaps require technically demanding dissection and sacrifice of normal tissue, and the results are not reliably superior to other techniques.
The abductor digiti minimi muscle flap, as described initially by Milward et al. (6) and later by Reisman and Dellon (7), necessitates an extensive dissection with a long arc of rotation and the
sacrifice of an important hypothenar muscle. Although this flap provides a well-vascularized tissue for coverage of the median nerve in recalcitrant carpal tunnel syndrome, residual abduction of the small finger may be noticed postoperatively. Wilgis (8) reported the lumbrical flap as an alternative option, which relies on a small intrinsic muscle. However, this flap does not always ensure adequate proximal coverage of the median nerve at the wrist, and long-term outcomes have not been published.
sacrifice of an important hypothenar muscle. Although this flap provides a well-vascularized tissue for coverage of the median nerve in recalcitrant carpal tunnel syndrome, residual abduction of the small finger may be noticed postoperatively. Wilgis (8) reported the lumbrical flap as an alternative option, which relies on a small intrinsic muscle. However, this flap does not always ensure adequate proximal coverage of the median nerve at the wrist, and long-term outcomes have not been published.
Dellon and Mckinnon (9) described the pronator quadratus muscle flap based on the neurovascular bundle of anterior interosseous artery and nerve. But this flap requires technically demanding dissection and cannot offer sufficient distal coverage of the median nerve further than the proximal wrist flexion crease. Rose et al. (10) proposed the palmaris brevis turnover flap. Nevertheless, this flap frequently leads to insufficient coverage of the median nerve due to small size of the muscle. Additionally, the muscle is absent in at least 2% of the patients.
The reverse radial artery fascial flap according to Tham et al. (11) allows sufficient coverage of the scarred segment of the median nerve. The flap is based on reverse flow through the ulnar artery sacrificing the radial artery. However, the communication between the radial and ulnar artery is absent in approximately 4% of the patients (12). An alternative fasciocutaneous island flap is the posterior interosseous artery flap, which relies on branches of the posterior interosseous artery (13). An intact communication between the anterior and posterior interosseous arteries is required to provide the retrograde flow to the flap. Yet, this communication is absent in 5% of the general population (14).
Free flaps of gliding tissue have also been described for coverage of the scarred median nerve such as the omentum and the adventitial flap based on the thoracodorsal vessels (15). These flaps are far more technically demanding with severe donor site morbidity, and, therefore, they should be used more as salvage procedures for patients with multiple previous procedures.
HYPOTHENAR FAT PAD FLAP
In contrast to the above reported interposition flaps, the hypothenar fat pad flap is not technically difficult, locally available, and expendable. It is a vascularized pedicle flap, which is based on the depth of the vasculature from the ulnar artery to the hypothenar fat. The hypothenar fat pad flap was initially described by Cramer and subsequently modified by Strickland and Mathoulin (16,17). It is the most commonly used flap for recalcitrant carpal tunnel syndrome providing a well-vascularized interposition tissue over the median nerve and the radial leaf of the transverse carpal ligament.
Indications
The hypothenar fat pad flap is indicated as a supplementary procedure to revision decompression of the median nerve in:
Persistence or recurrence of symptoms of carpal tunnel syndrome
Failure of nonoperative treatment (splinting, injection)
Significant median nerve hypersensitivity at the wrist with no damage of the palmar cutaneous branch of the median nerve
Progressive neurologic deficit in median nerve function (thenar muscle atrophy, expanded twopoint discrimination)
Technique
The procedure is performed under regional or general anesthesia and tourniquet control. Previous incisions for carpal tunnel release are used and extended both proximally and distally to identify the compressed median nerve in healthy tissues (Fig. 19-1). After exposure of the nerve to unscarred environment both proximally and distally, the dissection is continued toward the scarred section of the nerve using loupe magnification. The median nerve is released from the surrounding scar tissues and adhesions (Fig. 19-2). Internal neurolysis under operating microscope is performed only when there is severe compression and thinning of the nerve, lack of epineural vascularity, and severe muscle wasting. We routinely perform epineurotomy for severe nerve compression. Internal neurolysis is performed concomitantly if scar is noted between fascicules. Rarely is an entire epineurectomy performed.
To harvest the hypothenar fat pad flap, the Guyon’s canal can be initially released and the ulnar nerve and artery are identified and protected throughout the dissection of the flap (Fig. 19-3). The fat flap is raised by sharp subcutaneous dissection from the hypothenar eminence. Care is taken to maintain the vascularity of the hypothenar skin flap to avoid skin necrosis postoperatively. The harvesting proceeds from the distal wrist crease to midpalm, and while mobilizing the fatty tissue, care
is taken to avoid injury of the digital nerves to the ring and small fingers, which are often buried in the fat. Deep mobilization of the flap can be achieved by excising a segment of the ulnar leaf of the transverse carpal ligament.
is taken to avoid injury of the digital nerves to the ring and small fingers, which are often buried in the fat. Deep mobilization of the flap can be achieved by excising a segment of the ulnar leaf of the transverse carpal ligament.
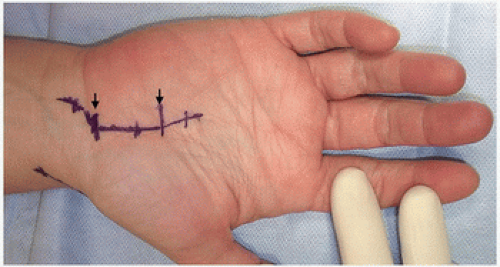 FIGURE 19-1 Previous carpal tunnel release incision (black arrows) is extended proximally and distally. |
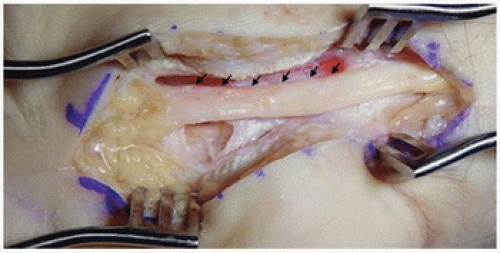 FIGURE 19-2 Median nerve after exposure and neurolysis. Note lack of epineural vasculature (black arrows). |
When an adequate fat flap has been harvested, the flap is mobilized to determine whether it can be easily advanced over the median nerve to the radial remnant of the transverse carpal ligament (Fig. 19-4). If sufficient mobilization is not achieved, additional dissection is carried out preserving the ulnar pedicle of the flap. Once the harvesting is complete, the flap is hinged like a book cover over the median nerve and is sutured to the radial remnant of the transverse carpal ligament (Fig. 19-5). Attention should be paid to suture the flap without tension placing the sutures from the radial edge of the flap to the radial edge of the transverse carpal ligament. Gentle compression of the radial and ulnar sides of the hand can facilitate to secure a tension-free flap. The tourniquet is deflated, and meticulous hemostasis is performed. After routine skin closure, the wrist is immobilized in short arm splint.
 FIGURE 19-5 The hypothenar fat pad flap (HFPF) is sutured to the radial remnant of transverse carpal ligament (black arrows
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|







