Surgical Management of Proximal Fifth Metatarsal Fractures
Jeannie Huh
Mark E. Easley
DEFINITION
The fifth metatarsal is the most frequently fractured metatarsal bone. Of these, proximal fractures are the most common.8
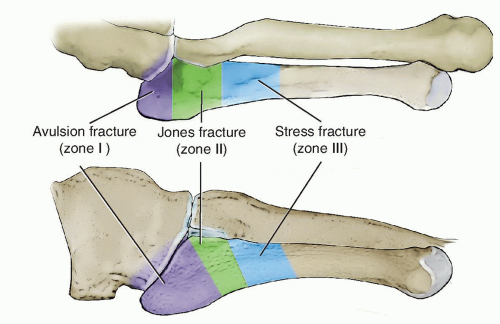
Proximal fifth metatarsal fractures are traditionally classified into three types, based on the zone or location of the fracture (FIG 1):
Zone I: tuberosity avulsion fracture that may extend to the fifth metatarsal-cuboid articulation
Zone II: classic “Jones fracture” at the metaphyseal-diaphyseal junction that extends into, but not beyond, the fourth and fifth intermetatarsal articulation
Zone III: proximal diaphyseal stress fracture
Identifying the correct zone is important because the healing characteristics and management differ for fractures occurring in each.
ANATOMY
The fifth metatarsal consists of a head, diaphysis, metaphysis, and tuberosity.
The tuberosity is the most proximal and plantar structure of the fifth metatarsal.
Proximally, the fifth metatarsal has articulations with the cuboid and fourth metatarsal.
There are four main soft tissue attachments to the proximal aspect of the fifth metatarsal:
The peroneus brevis tendon inserts on the dorsolateral tuberosity.
The peroneus tertius tendon attaches on the dorsal aspect of the metaphysis.
The lateral band of the plantar fascia attaches to the plantar aspect of the fifth metatarsal base.
Dorsal, plantar, and interosseus ligaments attach between the bases of the fourth and fifth metatarsals.
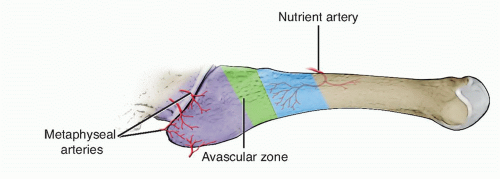
Blood supply to the proximal fifth metatarsal is derived from two sources (FIG 2):
Metaphyseal vessels supply the tuberosity.
An intramedullary nutrient artery enters from the medial cortex at the proximal diaphysis and flows retrograde, terminating at the metaphyseal-diaphyseal junction.
The region at which these blood vessels converge corresponds to a relatively avascular watershed area, making it a tenuous area for healing.13
The dorsolateral branch of the sural nerve usually lies approximately 2 to 3 mm proximal to the tuberosity and often courses at the incision site used for surgical fixation.4
The peroneus longus courses lateral to and then plantar to the cuboid, immediately proximal to the fifth metatarsal base (FIG 3).
PATHOGENESIS
Different mechanisms of injury have been associated with the different fracture zones:
Zone I (tuberosity) fractures result from forces exerted on the peroneus brevis tendon or the lateral band of the plantar fascia with foot inversion.
Zone II (Jones) fractures result from an indirect, large adduction force applied to the forefoot with the ankle in plantarflexion.
The ligaments at the base of the fourth and fifth metatarsals are resistant to displacement, resulting in fracture just distal to them, at the level of the fourth and fifth intermetatarsal joints.
Zone III (diaphyseal stress) fractures result from overuse or overload injuries.
These injuries may be acute or chronic.
Underlying hindfoot varus alignment has been implicated in overloading the lateral foot and is considered a predisposing factor for proximal fifth metatarsal fractures as well as nonunion and refracture if not addressed at the time of surgical stabilization.11
NATURAL HISTORY
Zone I (tuberosity) fractures nearly always heal with conservative management alone. Although patients can expect to return to their preinjury level of function, recovery may take 6 months or longer.5
Zones II (Jones) fractures are notorious for a high incidence of delayed union and nonunion (up to 28%)1 when treated conservatively and is thought to be due to their tenuous location:
Relatively avascular watershed zone
The peroneus brevis and the lateral band of the plantar fascia cause continued motion at the fracture site despite immobilization.
Zone III (diaphyseal stress) fractures are also notorious for their protracted healing time and risk of nonunion (shown to develop in up to 25% of nonoperatively treated cases).2
PATIENT HISTORY AND PHYSICAL FINDINGS
History
Usually entails injury to the foot during sports activity, especially basketball or football
In the nonathlete, tripping off a curb with the foot inverted is a common mechanism.
In the setting of an overuse injury, the patient may describe prodromal symptoms.
The patient will complain of painful weight bearing and tenderness over the lateral border of the foot that is reproducible with direct palpation.
Physical examination
Swelling and ecchymosis over the lateral border of the foot is often present.
Pain and/or weakness with eversion may be noted.
Evaluate for potential sources of lateral foot overload (ie, hindfoot varus), which can have implications on healing after fixation of a proximal fifth metatarsal fracture, if not simultaneously addressed.
Assess for signs of Lisfranc injury with direct palpation over the tarsometatarsal joint complex and presence of plantar ecchymosis.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior (AP), lateral, and oblique radiographs of the affected foot are sufficient to diagnose a proximal fifth metatarsal fracture (FIG 4A-C).
If there is suspicion for Lisfranc injury, weight-bearing radiographs of the affected foot should be obtained.
Computed tomography (CT) scan is rarely indicated but may assist in differentiating between acute and chronic fractures and degree of union after treatment (FIG 4D,E).
DIFFERENTIAL DIAGNOSIS
Cuboid fracture
Fifth metatarsal shaft fracture
Lisfranc injury
NONOPERATIVE MANAGEMENT
Conservative treatment is typically reserved for the following:
Zone I fractures
Patients of low activity demand with a zone II or III fracture
Patients with medical comorbidities that preclude surgery
Zone I fracture: weight bearing as tolerated in a hard-soled shoe or boot (6 to 8 weeks)
Zone II/III fractures: six weeks of cast immobilization and non-weight bearing, followed by an additional 6 weeks of boot immobilization with gradual advancement of weight bearing
SURGICAL MANAGEMENT
The indications for surgical fixation of proximal fifth metatarsal fractures remain.
Surgical treatment is indicated in the following:
Zone I fractures with symptomatic delayed union/nonunion
Preoperative Planning
Determine the appropriate type and method of fixation.
Percutaneous intramedullary screw fixation is the most widely used technique.
A variety of screw options exist and each have their advantages and disadvantages (ie, solid vs. cannulated, stainless steel vs. titanium, fully threaded vs. partially threaded vs. variable pitch).
Although the biomechanical properties of various screws have been shown to vary, no single type of screw has clinically been shown to be superior.
Recently, low-profile, precontoured proximal fifth metatarsal fracture plates have become popularized as an alternative fixation option. These plates have tines or “hooks” at one end, which serve to engage the proximal fracture fragment and provide rotational control. Indications for plate fixation may include the following:
Comminuted zone II fractures (FIG 5)
Osteoporotic bone
Revision cases after failed intramedullary screw fixation
Cases in which intramedullary screw fixation is less than optimal (ie, loss of cortical integrity, canal diameter too small to accommodate a minimum 4.5-mm screw)
Symptomatic delayed union or nonunion of zone I fractures
Determine if bone graft is desired.
We typically use bone graft harvested from the ipsilateral calcaneus in cases of comminution, osteoporotic bone, delayed and nonunions.
Determine if an underlying source of lateral foot overload (ie, hindfoot varus, chronic lateral ankle instability, etc.) is present and ensure that it is addressed, either surgically or conservatively (ie, orthotics, bracing), in conjunction with stabilization of the proximal fifth metatarsal fracture.
Positioning
The patient is placed supine with a bolster under the ipsilateral hip to internally rotate the leg, providing better access to the lateral foot.

FIG 5 • Non-weight-bearing AP (A), oblique (B), and lateral (C) radiographs of the foot of a 34-year-old female with a displaced and comminuted zone II fracture of the fifth metatarsal base.
Place the surgical foot at the lateral edge of the operating table. This facilitates use of a mini-fluoroscopy unit that will serve as a lateral extension of the table for portions of the case.
A calf tourniquet is used to avoid bleeding that may obscure structures at risk in the surgical field. Ensure it is placed distal to the fibular head to avoid pressure on the common peroneal nerve.
TECHNIQUES
▪ Percutaneous Intramedullary Screw Fixation
Incision and Dissection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree