Surgical Exposure of the Elbow Following Bony and Soft Tissue Trauma
Emilie V. Cheung
Nathan A. Hoekzema
Scott P. Steinmann
Indications/Contraindications
The soft tissue surrounding the elbow is thin and pliable, yet durable enough to withstand constant flexion and extension. Optimal functional recovery in traumatic elbow injuries requires early and, in many cases, immediate motion. Skin slough, delayed healing, and dehiscence of skin flaps following treatment of elbow fractures can adversely affect elbow rehabilitation, delaying motion and increasing the risks of infection and nonunion. Properly planned incisions can allow for excellent exposure of the elbow while maximizing skin flap vascularity, minimizing the risks of postoperative wound complications.
Surgical exposures of the elbow typically involve a ‘universal’ posterior incision. This allows circumferential access by the creation of full-thickness skin flaps medially and laterally as needed. This allows for all intraoperative possibilities and avoids the creation of skin bridges if further surgery is needed in the future. Alternatively, separate medial and lateral skin incisions may be performed for isolated medial and lateral exposure. Prior surgical procedures should be carefully noted preoperatively. Previous incisions may need to be incorporated in order to avoid creating narrow skin bridges which are susceptible to skin necrosis and potential wound complications.
Surgery
Patient Positioning
In our practice, the patient is routinely placed in the supine position with a small stack of towels placed underneath the ipsilateral scapula, and the arm draped across the chest after sterile preparation. The operating table should be slightly tilted away from the surgeon to help with visualization and exposure. This positioning is optimal for fixation of distal humeral fractures, radial head fractures, and medial or lateral ligament reconstruction. For medial ligament or coronoid fracture fixation, the supine position is used, but a sterile Mayo stand is utilized to position the arm more accurately for medial elbow exposure. Intraoperative fluoroscopy, if indicated, is placed on the ipsilateral side, and the elbow may be brought out laterally from the chest for the fluoroscope intermittently during the procedure. A sterile tourniquet is usually used in all elbow approaches. This allows for ease of removal if more proximal exposure of the humerus is needed. Hip rests or a bean bag may provide additional stability.
Posterior Approaches
Indications
Triceps repair
Combined medial and lateral approach
Distal humerus ORIF
Total Elbow Arthroplasty
Contraindications
Prior medial or lateral incisions.
Incision
The bony landmarks, including the olecranon process and the subcutaneous border of the proximal ulna, are marked (Figs. 9-1,9-2,9-3,9-4,9-5,9-6). The incision starts about 5 centimeters proximal to the olecranon process centered on the triceps tendon. It is then taken distally to either the lateral or medial side of the olecrenon, according to surgeon preference, and finishes distally following the subcutaneous border of the ulna. Full-thickness skin flaps are then developed, kept as thick as possible with the deep plane being the triceps fascia and epitenon proximally, and the forearm fascia and ulnar periosteum distally. If most of the surgical procedure will be on the medial side of the elbow, then the posterior incision should be placed to that side. Likewise, if a radial head fracture is being exposed, then the posterior incision should be made on the lateral side of the olecranon. If one chooses to err on the medial side of the olecranon, the incision should not be placed directly over the cubital tunnel, to avoid injuring the ulnar nerve.
Deep Dissection
The ulnar nerve is most easily found proximally between the medial intermuscular septum and the medial head of the triceps muscle. If the nerve is going to be transposed, it should be freed from proximal to distal in order to minimize damage to the nerve branches. Articular branches usually need to be sacrificed, but the first motor branch should be identified, mobilized,
and preserved. The leading edge, about 1 cm, of the distal medial intermuscular septum is removed to prevent tethering of the nerve after being anteriorly transposed. The nerve is then placed into a subcutaneous pocket anterior to the medial epicondyle. A suture is placed in the subcutaneous tissue and secured to the fascia to create a sling and prevent posterior subluxation of the nerve. If the nerve is not going to be transposed, care should be taken to avoid destabilizing the nerve in the cubital tunnel by leaving the soft tissue constraints of Osborne’s fascia intact.
and preserved. The leading edge, about 1 cm, of the distal medial intermuscular septum is removed to prevent tethering of the nerve after being anteriorly transposed. The nerve is then placed into a subcutaneous pocket anterior to the medial epicondyle. A suture is placed in the subcutaneous tissue and secured to the fascia to create a sling and prevent posterior subluxation of the nerve. If the nerve is not going to be transposed, care should be taken to avoid destabilizing the nerve in the cubital tunnel by leaving the soft tissue constraints of Osborne’s fascia intact.
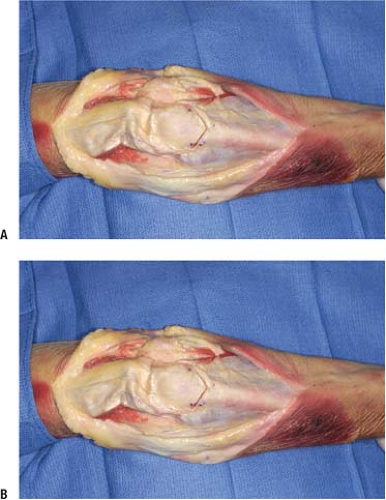
 FIGURE 9-3 The medial and lateral sides of the triceps muscle are released in order to fully visualize the posterior fossa and the ulnohumeral articulation. |
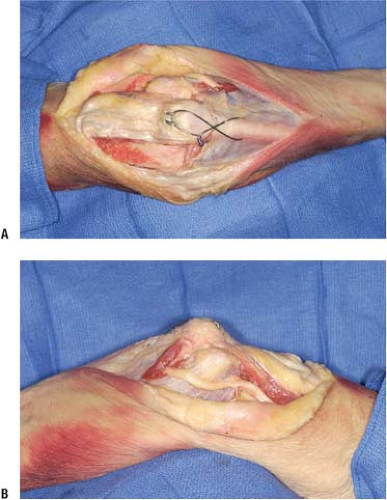
 FIGURE 9-5 The osteotomied olecranon is retracted with the triceps tendon demonstrating near full visualization of the articular spool. |
Olecranon Osteotomy
An olecranon osteotomy may be performed to gain full visualization of the articular surface of the distal humerus.
After identification and protection of the ulnar nerve, a capsulotomy is made at both the medial and lateral sides of the olecranon at the apex of the greater sigmoid notch to locate the olecranon “bare area.” This is the area of the olecranon where the articular cartilage narrows and is the optimal location for the osteotomy. A lap sponge may be threaded under the olecrenon to protect the distal humeral articular cartilage from inadvertent damage. The osteotomy is created in a Chevron configuration, with the apex usually pointed distally using an oscillating saw. The saw is used for one-third of the bone cut, the second third is made with an osteotome, and the last third is cracked or fractured open with an osteotome to create the completed osteotomy. Once the osteotomy has been made, the anconeus needs to be taken off the lateral side of the olecranon fragment. Transection of the anconeus will denervate it. To avoid this problem, one technique is an anconeus flap transolecranon approach (AFT) which involves detaching the anconeus as a flap distally to proximally until the osteotomy site is reached. The osteotomy is then performed and the olecranon fragment and the anconeus are retracted proximally together to expose the distal humerus. Alternatively, the anconeus may be elevated from the proximal fragment of the olecranon osteotomy and elbow region with its distal attachment on the ulnar shaft left intact. The anconeus is then retracted laterally while the proximal fragment of the olecranon osteotomy is retracted proximally, which allows ample visualization of the distal humerus. The osteotomy site has been reported to heal reliably with few complications.
It is advantageous to place the hardware on the proposed olecranon fragment (if using a cannulated screw or Kirschner wires) prior to making the osteotomy so that the tract of the hardware is created anatomically, which will facilitate optimal alignment of the osteotomy site at the end of the procedure. We use either two Kirschner wires or a 6.5 or 7.6 mm cannulated screw and washer, with an 18 gauge tension band wire. The drill hole for placement of the wire is placed at an equal distance from the olecranon osteotomy as the distance of the osteotomy site to the tip of the olecranon. The osteotomy should be repaired by advancing the K-wires into the anterior ulnar cortex distal to the coronoid. After the K-wires have reached the anterior cortex, they are backed out about 5 mm and bent 180 degrees and tapped back until buried under the triceps tendon. The triceps may then be sutured over the wires to discourage backing out. Alternatively, a precontoured olecranon plate may be utilized for fixation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree