The Pedicled Soleus Muscle Flap for Coverage of the Middle and Distal Third of the Tibia
Salvatore C. Lettieri
Steven L. Moran
Soft tissue defects involving the middle and lower third of the leg may occur following trauma, tumor extirpation, and osteomyelitis. Anteriorly the skin and subcutaneous tissue overriding the middle third and lower third of the tibia are thin and exposed bone and tendon may result from soft tissue injury or open fractures. Historically, middle third defects have been covered with the pedicled soleus muscle flap, while attempts have been made more recently to extend to soleus flap to cover defects of the lower third of the leg.
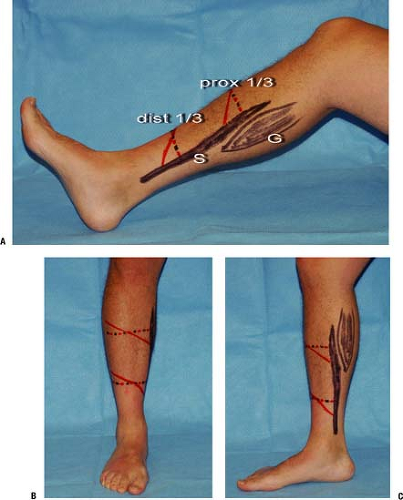
The soleus muscle, according to the Mathes and Nahai schema, is a type II muscle, containing dominant pedicles from the popliteal, peroneal, and posterior tibial arteries and minor segmental pedicles from the posterior tibial artery. The muscle lies in the superficial posterior compartment extending the entire length of the lower leg. The soleus originates from the posterior surface of the tibia, the interosseous membrane, and the proximal third of the fibula. The muscle runs deep to the gastrocnemius muscle in the upper third of the leg (Fig. 28-1). In the middle third of the leg, the muscle joins with the gastrocnemius muscle and is adherent to the calcaneal tendon. The soleus is a bipennate muscle with the medial and lateral muscle bellies each receiving an independent neurovascular supply; this allows the lateral and medial portions to be mobilized independently while preserving some function within the remaining soleus muscle. The medial head originates from the tibia and receives the majority of its blood supply from the posterior tibial artery. The lateral head originates from the fibula and receives the majority of its blood supply from the perineal artery, although 16% of muscles may be nourished entirely by the posterior tibial artery. The lateral and medial heads are fused proximally while a septum divides the muscle distally. This septum is an extension of the calcaneal tendon and soleus tendon. Dividing the muscle longitudinally at the level of the septum allows for the elevation of the medial and lateral hemi soleus flaps.
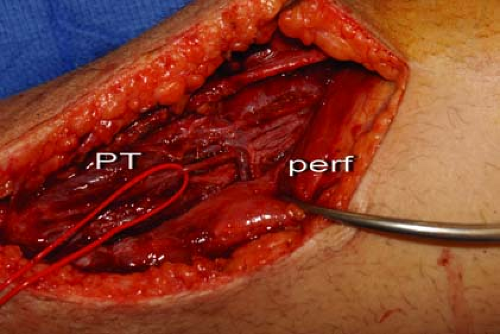
In the distal one third of the muscle, the soleus receives segmental arterial perforators from the posterior tibial artery (Fig. 28-2). These distal perforators may be absent in up to 26% of patients; in these cases distal perfusion to the muscle is provided by axial blood flow from more proximal perforators. The diameter and position of these distal perforators is variable but, if present and of large enough caliber, these perforators can allow for a portion of the muscle to be harvested in a reverse
fashion. The muscle may then be rotated 90 to 180 degrees, based on its distal perforators, allowing coverage of the lower third of the tibia and ankle region.
fashion. The muscle may then be rotated 90 to 180 degrees, based on its distal perforators, allowing coverage of the lower third of the tibia and ankle region.
The soleus functions to stabilize the ankle and assist in plantar flexion. The muscle works synergistically with the gastrocnemius and tibialis posterior muscle to provide plantar flexion, while the flexor hallucis longus, flexor digitorum longus, and tibialis posterior all help to provide ankle stability and resist dorsiflexion.
Indications/ Contraindications
The primary indication for the use of the soleus muscle flap is coverage of soft tissue defects in the middle third of the leg. Distal third defects have historically been covered with a free flap; however for small defects and in patients with significant comorbid disease, which would prohibit prolonged anesthesia times, a reverse soleus muscle flap may be considered as an alternative to free tissue transfer.
There are several factors which may prohibit the successful transfer of the soleus muscle and these are:
Size of the defect
Status of the muscle
Status of surrounding tissue and bone
Size and location of existing perforators
Size of the Defect
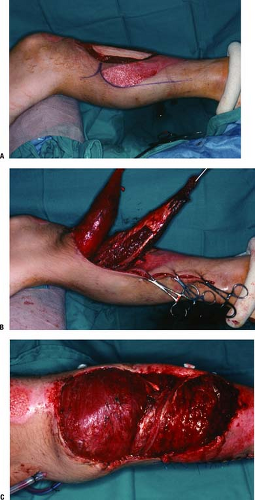
The soleus muscle has a limited surface area and a limited arc of rotation (Fig. 28-3). Large defects occupying the majority of the middle third and lower third of the leg are best covered with free tissue transfer. In addition, the distal aspect of the muscle can be unreliable if it must be stretched or inset under significant tension. In such cases, alternative methods of closure should be considered or the soleus may be used in conjunction with another flap.
The soleus can be used in conjunction with the medial or lateral gastrocnemius muscles for larger defects spanning the upper aspect of the lower leg, but this will compromise remaining plantar flexion (Fig. 28-4). When the defect is so large as to require more than just the soleus and medial gastrocnemius flaps, a free flap should strongly be considered as a means of soft tissue coverage and preservation of remaining posterior compartment function. Defects which are to be covered with a reversed soleus muscle flap should be less than 50 cm2 while the standard soleus flap can cover most defects under 75 cm2.
Status of the Muscle
Because the soleus muscle is closely adherent to the deep posterior surface of the interosseous membrane, tibia, and fibula, it can often be significantly traumatized following comminuted fractures of the tibia and fibula. During initial wound evaluation and debridement the muscle can often be inspected through the soft tissue defect. If the muscle is significantly lacerated by fracture fragments or contains a significant amount of intramuscular hematoma, it is most prudent to use another flap for soft tissue coverage. In addition, any associated injury to the popliteal, peroneal, or posterior tibial arteries can adversely affect the survival of the soleus muscle.
Status of Surrounding Tissue and Bone
Preexisting damage to the surrounding skin and deeper tissue of the middle third of the leg are also a relative contraindication to soleus muscle flap use. A history of previous radiation therapy, previous surgery, or penetrating trauma to the area surrounding the middle third of the leg should alert the surgeon to potential problems with the use of this flap. The soleus muscle has been shown to provide a source of collateral arterial flow between the posterior tibial and perineal arterial systems. In patients with vascular occlusions of the perineal or posterior tibial arteries, use of the soleus muscle may further compromise limb vascularity.
Size and Location of Existing Perforators
Indications for use of the soleus for distal third defects are based on the work of Pu and include (a) defect size less than 50 cm, (b) defects located over the anterior or medial portion of the distal tibia,
(c) the presence of large perforators in distal 4 cm to 5 cm of muscle and (d) a soleus muscle which is nontraumatized on initial exploration (4,5,6). If these factors are met a reversed hemi soleus flap may be attempted for lower third defects, otherwise a free flap is chosen for distal third defects. In addition, patients who have a smoking history, peripheral vascular disease, and history of lower leg radiation therapy should be considered high risk for a reversed soleus muscle flap.
(c) the presence of large perforators in distal 4 cm to 5 cm of muscle and (d) a soleus muscle which is nontraumatized on initial exploration (4,5,6). If these factors are met a reversed hemi soleus flap may be attempted for lower third defects, otherwise a free flap is chosen for distal third defects. In addition, patients who have a smoking history, peripheral vascular disease, and history of lower leg radiation therapy should be considered high risk for a reversed soleus muscle flap.
Preoperative Planning
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree