Heterodigital Arterialized Flap
Shian Chao Tay
Lam Chuan Teoh
Indications/Contraindications
Hand trauma that results in exposed bone, tendon, joint, or neurovascular structures requires some type of flap coverage. Defects located around joints and web spaces may also require flap coverage to avoid contractures that could occur following split thickness grafting. The location and size of these defects can often preclude the use of small rotation or advancement flaps. Free flap coverage is an option, but the presence of surrounding infection or a wide zone of trauma may make the recipient vessels’ dissection difficult. In such situations, a heterodigital arterialized (HTA) flap may be the best option.
The HTA flap is raised from the lateral side of a donor finger together with the digital artery and a dorsal digital vein. Unlike Littler’s neurovascular island flap, or Hueston’s extended neurovascular island flap, the heterodigital arterialized flap’s main function is to provide non-sensory reconstruction of skin defects in the hand or fingers. Thus, this flap is never harvested with the finger pulp or the digital nerve of the donor finger. This is an important feature that serves to reduce morbidity to the donor finger. The inclusion of the digital dorsal vein into the flap improves venous drainage of the flap and reduces the incidence of venous congestion, which is a well-documented complication of the classic Littler flap.
The heterodigital arterialized flap is a thin flap. In this aspect it is ideal for reconstruction in the hand and fingers as it provides near like-to-like reconstruction. The other advantages of this flap is that being regional, it obviates the need to prepare a separate surgical site and allows for almost immediate motion of the reconstructed finger. The reconstruction can be performed as a single-stage procedure (as compared to the cross-finger flap or groin flap).
In our experience, the heterodigital arterialized flap has been used to reconstruct volar, lateral, or dorsal defects in the fingers proximal to the distal interphalangeal joint, web spaces, palm, dorsum of the hand, and the thumb. The average flap dimensions are 4.1 cm (range, 1.5 to 5.5 cm) in the longitudinal axis and 2.1 cm (range, 1.0 to 3.5 cm) in the transverse axis. The HTA flap is thus a useful option to consider when faced with the problem of a relatively large defect in the hand or finger that requires non-sensory flap reconstruction. The HTA flap has been used for reconstruction of defects following infection, trauma, post-replantation of digits, electrical burns, chemical burns, and high-pressure injection injuries.
In terms of flap mobility, the reach of the heterodigital arterialized flap is limited to coverage of defects in the adjacent fingers or thumb or adjacent parts of the hand. This is principally due to the combined limitations in the reach of the dorsal vein and the digital artery of the flap. In situations where a greater reach is required, it is possible to divide the dorsal vein of the flap over the dorsum of the hand and reanastomose it in a region of healthy tissue after flap transfer. With this maneuver, the flap should have the ability to reach defects two to three fingers away, much like the traditional reach of Littler’s neurovascular island flap, when pivoting at the common digital artery’s offshoot at the superficial palmer arterial arch.
The HTA flap is absolutely contraindicated if there is only one functioning digital artery in the donor finger and when the vascular viability of any other adjacent fingers is threatened by flap harvesting.
It is also relatively contraindicated if the functional prognosis of the finger to be reconstructed is judged to be so poor that it might be better to amputate it. However, we recognize that social or cultural practices may still dictate reconstruction for the purpose of cosmesis or the maintenance of the “whole” self. Conversely, if there is a rare situation wherein a need to perform a digital amputation exists in a hand containing a defect requiring flap reconstruction, the HTA flap can be used as a fillet flap from the amputated finger for defect reconstruction. In such a situation, the HTA flap is very useful in spare parts surgery as there is no concern for donor finger morbidity. If the defect occurs beyond the reach of the flap or in the contralateral hand, a free fillet HTA flap can be created from the finger to be amputated provided the conditions at the recipient finger allows for a free flap.
It is also relatively contraindicated if the functional prognosis of the finger to be reconstructed is judged to be so poor that it might be better to amputate it. However, we recognize that social or cultural practices may still dictate reconstruction for the purpose of cosmesis or the maintenance of the “whole” self. Conversely, if there is a rare situation wherein a need to perform a digital amputation exists in a hand containing a defect requiring flap reconstruction, the HTA flap can be used as a fillet flap from the amputated finger for defect reconstruction. In such a situation, the HTA flap is very useful in spare parts surgery as there is no concern for donor finger morbidity. If the defect occurs beyond the reach of the flap or in the contralateral hand, a free fillet HTA flap can be created from the finger to be amputated provided the conditions at the recipient finger allows for a free flap.
Preoperative Planning
All practical options available for reconstruction should be considered by the surgeon before deciding on the HTA flap. Risks of heterodigital donor finger morbidity should be carefully weighed against benefits of reconstruction. Often, the location, size, and nature of the defect will preclude other reconstructive options, leaving the HTA flap as the most viable option with the highest flap survival rate.
The choice of donor finger is often dictated by the location of the defect and is often an adjacent finger. The outside borders of the index and little fingers are not used as donor sites to preserve hand cosmesis and to maintain native skin for protection and sensation. This requirement is not absolute; however, we prefer the use of the middle finger, ring finger, and the ulnar border of the index finger. Theoretically, the radial border of the little finger can be used as a donor site but this is rare as the little finger is small, providing little skin, and the remaining ulnar digital artery is often absent or vestigial.
A digital Allen’s test must be performed on the intended donor finger to ensure that both digital arteries are sufficiently patent. In addition, the Allen’s test should also be performed on the finger that is adjacent to the donor site as this would dictate if the digital artery mobilization can proceed proximal to the point of bifurcation of the common digital artery. More often than not, a longer reach is required and ligation and division of the neighboring branch of the digital artery to the adjacent finger would need to be performed to create an arterial pedicle of sufficient length.
If the donor site is just next to the defect in the adjacent finger, also known as the contiguous or near side of the adjacent finger (e.g., defect on ulnar side of index finger with donor site on radial side of middle finger), the pivot point can be at the bifurcation of the common digital artery, as a short pedicle would be sufficient. This pivot point can be approximately landmarked in the intermetacarpal space at the level of the distal palmer crease. The distance from this pivot point to the proximal edge of the defect can then be measured to determine the reach needed by the flap and hence the location of the proximal margin of the flap. If the flap is not coming from the contiguous side of the adjacent finger, it is likely that a more proximal pivot point would be required to ensure sufficient reach of the flap. The most proximal point would be the superficial palmer arterial arch, which can be approximated to the level of the proximal palmar crease in the relevant intermetacarpal space. In such situations, as mentioned previously, it will be necessary to ligate and divide the neighboring digital artery of the common digital artery that supplies the adjacent finger to maximize the reach of the flap.
Experience has shown that the reach of the flap increases by 10% once the digital artery is adequately mobilized. However, in the interests of safety and ensuring minimum tension in the pedicle, a 1:1 ratio should still be maintained for the length of the arterial pedicle during preoperative planning of flap surgery.
The timing for reconstruction depends on the pathology. As far as possible, early reconstruction (within 1 week) is preferred as it minimizes overall hand stiffness from prolonged disuse. For traumatic conditions, the reconstruction is ideally performed within 1 week. For post-replantation surgery with residual skin defects, the resurfacing is performed within 10 to 15 days when re-endothelialization of the vascular anastomoses is completed. Infection cases are ideally resurfaced within 4 to 7 days when the surrounding cellulitis and edema have subsided. In order to achieve this time line in infective cases, infection reversal should be achieved within one to two formal definitive excisional debridement surgeries in conjunction with appropriate intravenous antibiotics.
The surgery can be performed under general or regional anesthesia with sedation. The patient’s general condition and coagulation profile should be optimized as per any reconstructive surgery. The
patient should be consented and counseled as to the surgery, the postoperative course, and the duration of stay following surgery.
patient should be consented and counseled as to the surgery, the postoperative course, and the duration of stay following surgery.
Surgery
Patient Positioning
The patient should be in the supine position, and care should be taken to protect bony prominences with suitable pressure-relieving bolsters. The upper limb with the hand requiring reconstruction should be abducted to not more than 80 degrees at the shoulder to prevent excessive stretch to the nerves in the axilla. The elbow should be flexed slightly so that the forearm can be placed transversely on a stable hand table. A pneumatic tourniquet should be applied to the most proximal part of the upper arm, and the upper limb should be cleaned and draped as far proximal until the distal edge of the tourniquet. If the surgery is expected to last more than 2 hours, urinary catheterization should be considered.
Technique
The surgery is performed under tourniquet control, which should be inflated with the upper limb elevated but not exsanguinated. This is to facilitate identification and mobilization of the digital artery and the digital dorsal vein. The defect should be thoroughly debrided and irrigated. A template of the defect is made. At this point, the digital Allen’s test can be repeated to confirm the adequacy of both digital arteries in the donor finger, and also in the adjacent finger if the flap is not taken from the contiguous side of the finger adjacent to the defect.
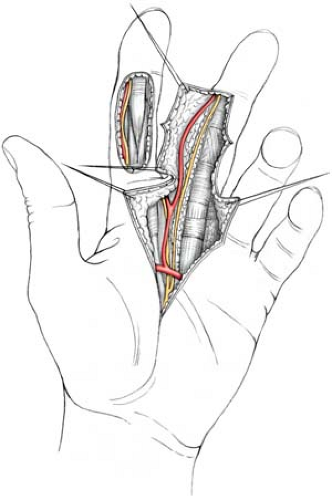
Using the template created, the appropriate dimension of the flap is then transferred onto the donor site. The flap should be centered on the lateral or dorsolateral side of the finger, depending on the width of flap required, to ensure the inclusion of the digital artery and a dominant digital dorsal vein. The maximum width of the flap should not exceed the mid-palmer line and the mid-dorsal line (a width of approximately 3 cm). The maximum length of the flap is from the base of the finger to the distal interphalangeal joint crease (usually 4 to 5 cm depending on the size of the finger). If necessary, the flap length may be extended 0.5 cm distal to the distal interphalangeal joint crease. Next, a palmar Z incision is drawn, biased to the respective side of the finger to access the proximal part of the digital artery. This incision is carried into the palm to the level of the common digital artery. The location of the dominant dorsal digital vein is then verified and marked to ensure that it will drain the flap. Once this is completed, the flap is ready to be harvested.
Heterodigital arterialized flap harvesting is performed with the aid of loupe magnification. The flap is first raised from its palmar margin (Fig. 21-1). If the palmar margin of the flap crosses any digital palmer flexion creases, a mini-z cut can be made at these creases, to break up the resultant scar line. Superficial palmer veins can be carefully cauterized with bipolar electrocautery and divided. As one proceeds deeper, the dissection follows the digital artery from proximal to distal starting from the bifurcation of the common digital artery. The angle of dissection toward the neurovascular bundle is an oblique plane skiving dorsal to the digital nerve, which is more central and superficial compared to the digital artery. As far as possible, the nerve should be left undisturbed in its bed with a collar of fat kept around it. Besides ensuring that the nerve is not traumatized, the collar of fat also provides additional cushioning and enhances the take of the full-thickness skin graft at the donor site. Ideally, a collar of fat or soft tissue should also be kept around the digital artery to preserve the venae comitantes. Fortunately, in the HTA flap, this is not as critical, as the dorsal vein would provide the main conduit for venous drainage.
At this point, an intraoperative occlusion test can be performed using non-traumatic microsurgical vascular clamps to determine the integrity of the contralateral digital artery in the donor finger. If mobilization of the digital artery to the level of the superficial palmer arch is necessary, a similar occlusion test should be performed on the bifurcated digital artery supplying the adjacent non-donor finger to ensure that it also has a healthy contralateral digital artery.
As mobilization of the digital artery progresses, the transverse palmer arches of the digital artery will be encountered. These are rather large and short. Sufficient room is developed and the arches can be carefully cauterized with bipolar electrocautery before division. Care should be taken to ensure that the bipolar electrocautery is applied at least 2 mm from the parent artery to prevent compromising flow in the main digital artery.
Dorsal dissection is performed next with proximal to distal dissection and mobilization of the dominant dorsal digital vein to ensure inclusion of the vein in the flap. The flap is dissected free from the extensor tendons in the plane superficial to the paratenon. Care should be taken not to damage the dorsal skin branches of the digital artery supplying the flap. At the distal margin of the flap, the distal end of the dominant dorsal vein is ligated and divided, and the same is performed for the digital artery on the palmer side.
At this stage, the flap should be detached from distal to proximal. The adherent fibrous septa and Cleland’s ligaments are divided. At the base of the digit, some dissection may be necessary to complete the division of subcutaneous tissues attached to the flap. The natatory ligament at the web space may also be divided to prevent kinking of the dorsal vein and lengthen the reach of the flap.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree