Chapter 63 Surgery of the Patellofemoral Joint
Proximal Realignment
Disorders of the patellofemoral joint are numerous and are of great importance because they seriously limit patients’ function. Treatment of these conditions is highly dependent on an accurate diagnosis and determination of the correct cause.55 Within the spectrum of disorders of the patellofemoral joint, one of the more common is patellar instability, which will be the focus of this chapter. Instability can present with a variety of symptoms that mimic other pathology of the knee, such as pain, mechanical “clicking,” feelings of instability or “giving out,” weakness, and limited range of motion. We begin with a review of the presentation and pathophysiology of patellofemoral disorders, including patellofemoral instability. We then review physical examination of the patellofemoral joint, imaging modalities, and the surgical technique of proximal realignment.80 The techniques of patellofemoral arthroplasty and distal patellar realignment are beyond the scope of this chapter and are discussed elsewhere in the text. A review of the biomechanics of the patellofemoral joint is recommended in conjunction with this chapter.
Pathophysiology of Patellar Instability
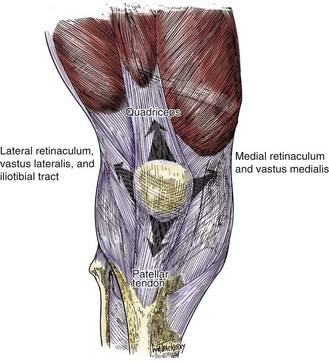
The stability of the patellofemoral joint is dependent on many factors. Specifically, it depends on the congruence of the trochlea and patella, static ligamentous stabilizers, and dynamic stabilizers. Bony and cartilaginous constraint is determined by the shape of the trochlea and the patella, which can be extremely variable. For example, a hypoplastic lateral condyle or a shallow trochlea can predispose to acute patellar dislocation after trauma, or can lead to chronic subluxation and dislocation. In addition to bony and cartilaginous constraints are the static ligamentous constraints. We now understand that the medial patellofemoral ligament (MPFL) is the greatest static stabilizer for lateral translation of the patella.24,33,34,95 Finally, and perhaps most important, is the quadriceps mechanism. The coordinated contraction of the quadriceps mechanism centralizes the patella in the trochlea throughout a range of motion (Fig. 63-1). It is well known now that the vastus medialis obliquus (VMO) is the primary dynamic stabilizer of the patellofemoral joint (Fig. 63-2). Dysfunction of the VMO, whether by trauma or by atrophy, may lead to patellar instability. It is interesting to note that as we learn more about the anatomy of medial restraints, we are learning to appreciate the important relationship between the MPFL and the VMO.91 The sum of these factors defines the ultimate stability of the joint. If any single factor or multiple factors are deficient or dysplastic, the remaining structures must compensate. The ability of these factors to collectively stabilize the joint determines the stability or instability of the joint. In the remainder of this chapter, we will describe how the history, physical findings, and radiographic studies are used to determine the relative contribution of each of these factors to the instability of the patellofemoral joint.
Physical Examination
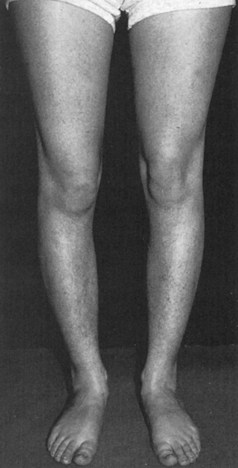
The examination begins with the patient standing with the feet together. Genu varum or valgum can be observed readily, as can rotatory malalignment such as in-facing or “squinting” of the patellae in patients with an increased quadriceps (Q) angle and hip anteversion (Fig. 63-3). Quadriceps tone and development can be appreciated in the standing position or during a half-squat. Hypoplasia of the VMO should be noted. Normally, the vastus medialis inserts on the upper third or half of the medial border of the patella. In knees with patellofemoral dysplasia, the muscle belly may end a few centimeters short of the superior patellar margin. The presence of quadriceps atrophy implies decreased dynamic muscle control on the patella.
The position of the foot also deserves attention. Eversion at the subtalar joint is accompanied by compensatory internal tibial torsion, which increases the Q angle and consequently stress on the patellofemoral joint. The subtalar joint is a single-axis joint that acts like a hinge connecting the talus to the calcaneus. The axis of the subtalar joint deviates an average of 23 degrees medially and anteriorly to the long axis of the foot and 41 degrees inferiorly and posteriorly in relation to the horizontal plane. Therefore, internal rotation of the leg causes eversion of the heel and depression of the medial side of the foot. External rotation of the leg produces the opposite effect.22 Subtalar joint eversion may be primary or secondary, as in knees with varus alignment or tibia vara, wherein compensatory subtalar joint eversion is required to produce a plantigrade foot. This phenomenon is probably more important in long-distance runners.62 Eversion of the heel (heel valgus) is readily appreciated by looking at the patient in the standing position from the back side. Abduction of the forefoot is evaluated in the standing position by palpation of the talar head on the anterior aspect of the ankle. The neutral position is defined when the head of the talus can be equally palpated on the medial and lateral sides. During weight bearing, a normal foot is in mild pronation, and additional pronation should still be possible.18
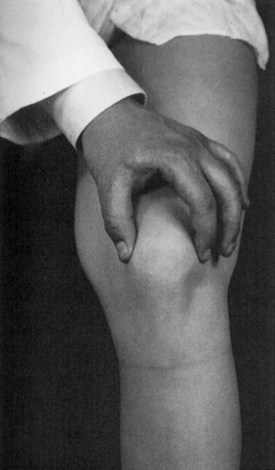
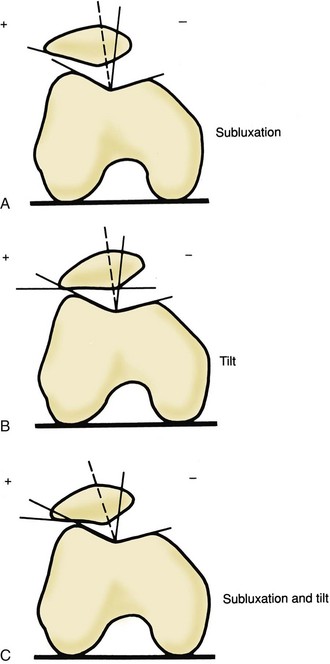
Ficat and Hungerford36 stress the importance of observing the entrance and exit of the patella into and out of the sulcus between 10 and 30 degrees of flexion. They describe four common abnormalities in patellar tracking. Normal patellar tracking is present when the patella glides smoothly into the sulcus, and only minimal lateral displacement may be appreciated in the final extension when the patella exits the trochlear groove. We define more marked lateral displacement as lateralization, whereas greater degrees of pathologic tracking are defined as subluxation or dislocation. This finding is also called the J sign because the path resembles an upside-down J. (See video on the website.) Furthermore, evaluation of the tilt of the patella should be attempted. In normal knees, the medial border of the patella should be at the same level as the lateral border, with a minor lateral tilt in full extension. It should be noted that most abnormalities in patellar tracking involve lateral displacement and lateral tilt of the patella in extension, which reduces in flexion. Therefore, we find it useful to roughly estimate patellar subluxation and tilt during the physical examination (Fig. 63-4) and to verify this later with radiographic axial views or computed tomography (CT). Other abnormalities in patellar tracking, including medial dislocation or subluxation of the patella in flexion (after over-release of the lateral structures and excessive medial displacement of the tibial tuberosity) or lateral dislocation in flexion (as in habitual or permanent dislocation), may be encountered more rarely.
Hughston and Walsh51 described a lateral position of the patella in the flexed knee for which they coined the term frog-eye patella. This seems to be associated with patella alta, which can be suspected clinically when the fat pad is unusually prominent. In fact, the fat pad may, on inspection, be mistaken for the patella because it occupies the femoral sulcus with the knee in extension while the patella is situated in the supracondylar pouch.
The Q Angle (Quadriceps Angle)
The Q angle is measured by drawing an imaginary line connecting the center of the patella and the anterior superior iliac spine to produce a surface marking that approximates the line of pull of the quadriceps tendon (Fig. 63-5). A second line drawn from the center of the patella to the center of the tibial tubercle indicates the direction of the patellar tendon. The intersection of these two imaginary lines forms the Q angle. Because this measurement is affected by rotation of the hip, an effort is made to note the position of the medial border of the patient’s foot during walking and to reproduce this position during measurement.
Active pronation or supination of the foot should be avoided because, as mentioned earlier, these movements are associated with internal and external rotation of the leg, respectively,91 and consequently increase and decrease the Q angle.
Aglietti and associates measured the Q angle in 150 normal subjects and found it to be 15 degrees (range, 6 to 27 degrees; standard deviation [SD], 3 degrees) (Table 63-1).3 It was lower in men (14 degrees; SD, 3 degrees) than in women (17 degrees; SD, 3 degrees), and the difference was significant (P = .001). Only 11 subjects, all women, had Q angles greater than 20 degrees (7%). Therefore, it seems that a Q angle greater than 20 degrees may reasonably be considered abnormal. The Q angle was also measured in a group of pathologic knees, including 53 patients with patellar pain and 37 with recurrent subluxation or dislocation. In the knees with patellar pain, the Q angle was significantly increased to 20 degrees; this was true for both men and women. In contrast, the Q angle was not significantly different from normal in knees with recurrent subluxation or dislocation (average, 15 degrees), and the same applied to both men and women. In patients with patellar subluxation or dislocation, the Q angle is usually underestimated for at least two reasons: first, the patella is displaced laterally in extension; second, the quadriceps tendon frequently lies more lateral than predicted when the superior iliac spine is used as the surface marking (Fig. 63-6).
Table 63-1 Measurement of Quadriceps Angle and Radiographic Measurements of Patellar Height and Patellofemoral Congruence
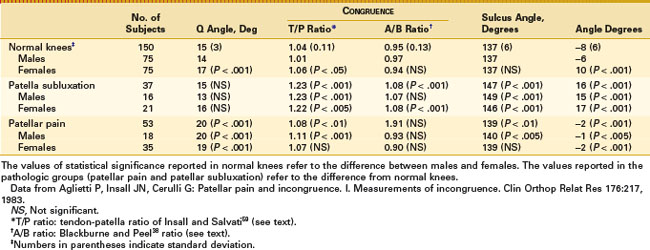

Figure 63-6 The quadriceps tendon often lies more laterally than the surface marking of the Q angle predicts.
To overcome the problem of lateral patellar displacement and consequent underestimation of the Q angle, Fithian and colleagues37 measured the Q angle with the knee in 30 degrees of flexion. They simultaneously applied a posteriorly directed force so that the patella symmetrically contacted the trochlea. With this method, the Q angle was 12 degrees in control subjects (11.2 degrees in men and 13.4 degrees in women). A significantly higher value was found in a group of knees with patellar dislocation (average, 19.2 degrees). The contralateral knee of patients suffering from patellar dislocation also showed an increased value of the Q angle (average, 18.4 degrees).
It is debated whether the Q angle is better measured in the supine or the standing position. Woodland and Francis118 measured the Q angle in the supine and standing positions in a large number of normal men78 and women.76 Average values in the supine position were 12.7 degrees for men and 15.8 degrees for women. Changing to the standing position increased the Q angle 0.9 degree in men and 1.2 degrees in women. The difference was statistically significant but probably is less significant clinically. It is relevant to note that the values determined by Woodland and Francis118 are close to those detected by Aglietti and coworkers.3
It has been suggested that the Q angle should be measured at 30 degrees of knee flexion and with maximum external tibial rotation107 because this position would give a more reliable measurement of the maximal valgus vector imposed on the patella. However, the difficulty involved in achieving standardized knee flexion and hip rotation makes the reproducibility of this measurement less reliable.
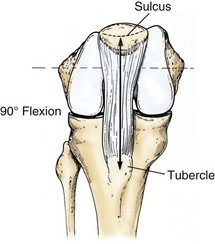
We recommend measurement of the tubercle-sulcus angle (TSA), as described by Kolowich and coworkers.65 The TSA is measured with the knee at 90 degrees of flexion (Fig. 63-7). This allows the patella to engage in the sulcus and highlights any rotational abnormalities. It is defined as the angle formed by a line perpendicular to the transepicondylar axis and a line from the tibial tubercle to the center of the patella. The normal value for the TSA is 0 degrees, and values greater than 10 degrees are considered pathologic. However, consistent identification of the transepicondylar line is not easy, especially in obese patients.
In the supine position and with the knee in extension, the patient is asked to contract the quadriceps, and upward movement of the patella is noted (lateral pull test). In a normal knee, the patella is pulled predominantly upward with an associated minor lateral displacement. The lateral pull test result is considered abnormal if lateral displacement is excessive.65
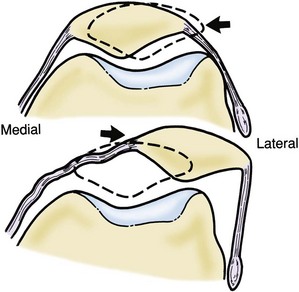
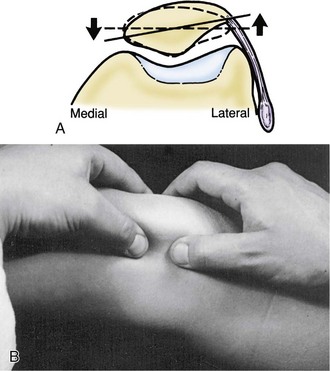
Patellar mobility should be evaluated with the knee in full extension and at 30 degrees of flexion. With the knee in extension, the patella is out of the trochlear groove and may be easily displaced medially and laterally. Gross hypermobility, as seen in patients with patella alta and a dysplastic extensor apparatus, is easily detected in this position. With the knee flexed 20 to 30 degrees, the patella is normally drawn into the trochlear groove and stabilized. Excessive displacement in the lateral direction indicates laxity of the medial retinaculum, or vice versa. On the other hand, reduced medial mobility indicates the presence of a tight lateral retinaculum. Kolowich and colleagues65 suggested that patellar mobility is best evaluated by dividing the patella into longitudinal quadrants (Fig. 63-8). With the knee at 20 to 30 degrees of flexion, mobility in the medial or lateral direction should not exceed two quadrants. A medial glide of one quadrant or less suggests a tight lateral retinaculum, which may also be investigated by trying to lift the lateral border of the patella with the knee in extension (passive patellar tilt) (Fig. 63-9). If the transverse axis of the patella cannot be elevated beyond the horizontal plane, a tight lateral retinaculum is demonstrated.65
Medial and lateral displacement of the patella has been measured with a displacement transducer37 or axial radiographs.112 Fithian and associates37 used a displacement sensor to record motion in the coronal plane with the knees bent at 30 degrees. Forces of 2.5 and 5 lb were applied with a hand-held force applicator with a load cell. Under a 5-lb force, medial patellar displacement averaged 9.2 ± 3.5 mm, and lateral displacement was 7.7 ± 2.6 mm in a group of 188 normal knees. In a group of 22 patients with symptomatic lateral patellar dislocation, medial displacement at 5 lb was 8.3 ± 4.5 mm, and lateral displacement was 11.5 ± 4.7 mm. Using the lateral minus medial displacement index, control knees had an average value of −2.1 ± 2.8 mm. Symptomatic knees had a lateral minus medial displacement of 3.2 ± 3.4 mm. The difference was statistically significant. In summary, total mediolateral displacement of the patella in normal knees under a 5-lb force was close to 17 mm in normal knees and almost 20 mm in knees with patellar instability. The lateral minus medial displacement was useful for differentiating between normal and unstable patellae. Medial displacement was larger than lateral displacement in 81% of control subjects. In unstable patellae, lateral displacement was larger than medial displacement. Asymptomatic knees in patients with unilateral patellar dislocation could not be used as controls because they showed abnormal patellar mobility, similar to symptomatic knees. The authors offered the concept of balance between medial and lateral structures. A normal knee should have greater medial than lateral displacement. If lateral displacement exceeds medial displacement, the restraining structures are unbalanced.
Teitge and colleagues112 evaluated medial and lateral patellar mobility with an axial radiograph at 30 to 40 degrees of flexion and a spring-loaded scale to apply a 16-lb force (7.3 kg). In a group of 20 asymptomatic knees, medial displacement averaged 11.1 ± 3.6 mm, and lateral displacement was 11.6 ± 8.1 mm. These values are higher than those reported in the study by Fithian and coworkers,37 but the displacing force was also greater (16 lb vs. 5 lb). In a group of knees with lateral instability, medial displacement was comparable (11.6 mm on average), whereas lateral displacement was highly increased to 21.9 mm on average.
Turner and Smillie114 measured tibial torsion in 836 patients with a tropometer. They found an average lateral tibial torsion of 19 degrees in control knees, which was increased to 24.5 degrees in knees with patellofemoral instability, and to 24 degrees in those with chondromalacia. Because increased tibial rotation was also noted in Osgood-Schlatter disease, this finding does not seem to be specific for patellofemoral joint disorders.
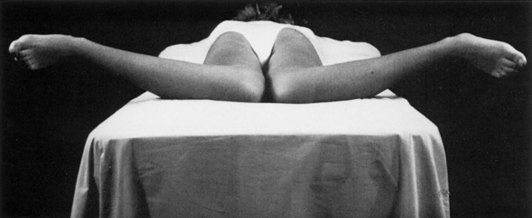
The amount of femoral neck anteversion has often been indirectly estimated by measuring the proportion of internal to external rotation of the hips in extension (Fig. 63-10), which would be its major determinant.9,109,110 Carson and colleagues18 suggested that if internal rotation of the hip in extension exceeds external rotation by more than 30 degrees, femoral neck anteversion is increased. Insall and colleagues58 suggested that increased femoral neck anteversion may be present in knees with patellofemoral malalignment. Hvid and Andersen52 measured the Q angle and internal rotation of the hip in 29 patients with patellofemoral complaints. They found that both the Q angle and internal hip rotation were higher in women than in men. A significant correlation between the Q angle and hip rotation was noted, thus suggesting that the Q angle is in fact increased because of excessive femoral neck anteversion. Other authors,35 however, have failed to identify any significant differences in Q angle, genu valgum, and anteversion of the femoral neck between normal adolescents and adolescents or adults with anterior knee pain. They concluded that because those affected by knee pain are also those most interested in sports activities, the probable cause is chronic overloading rather than faulty mechanics.
Dejour and associates30 reported CT measurements of femoral anteversion and tibial torsion in normal controls and in knees with instability of the patella. They found that femoral neck anteversion was increased in knees with patellofemoral instability (15.6 degrees) as compared with controls (10.8 degrees). Tibial torsion was a less important factor. It was 33 degrees in the control group and 35 degrees in the knees with patellar instability.
Summary of Physical Examination for Patellofemoral Instability
The TSA is measured with the knee at 90 degrees of flexion. The patella is engaged in the sulcus. The angle is formed by a line perpendicular to the transepicondylar axis and a line from the tibial tubercle to the center of the patella. The normal TSA is 0 degrees, and an abnormal TSA measures greater than 10 degrees (see Fig. 63-7).100
Atrophy of the quadriceps muscle, especially the VMO, is noted.
Tightness and laxity of the medial and lateral soft tissue restraints are assessed. With the knee flexed to 20 to 30 degrees, the patella is displaced medially and laterally. Medial displacement of less than one quarter of the patella, or 5 mm, indicates a tight lateral retinaculum. Lateral displacement of more than three quadrants indicates medial soft tissue incompetence (see Figs. 63-8 and 63-9). Inability to tilt the patella past horizontal is indicative of a tight lateral retinaculum.65
Patellar tracking is assessed throughout a range of motion. A J sign,36 in which the patella is tracking in an inverted J pattern, represents the patella that is tracking centrally and then shifts laterally as the knee is extended. (See video on the website.) At 90 degrees, the patella should be centered between the femoral condyles in a normal patellofemoral joint.
Radiographic Studies in the Diagnosis and Treatment of Patellofemoral Instability
Radiography
Lateral View
Patellar position is related to the length of the patellar tendon. Patella alta, in particular, is associated with patellar instability, dislocation, and abnormalities of the trochlear groove. Patella alta, in particular, has been identified as a strong contributor to patellofemoral instability. Several methods of measurement have been described, including those reported by Blumensaat,15 Insall and Salvati,59 Blackburne and Peel,14 Caton et al,20 Rünow,93 and Grelsamer and Meadows.42
Blumensaat’s Line
Blumensaat15 states that on a lateral radiograph with the knee flexed 30 degrees, the lower pole of the patella should be on a line projected anteriorly from the intercondylar notch (Blumensaat’s line). It is difficult to obtain routine radiographs with the knee flexed exactly the required number of degrees; this limits the usefulness of the method. Blumensaat’s method is also inaccurate. Of 44 radiographs of the knee that were flexed exactly 30 degrees, in no case did the lower pole of the patella lie on Blumensaat’s line; rather, the patella was positioned above this line (Fig. 63-11).
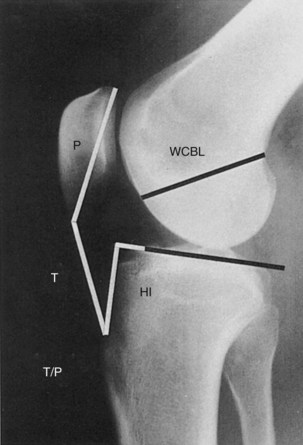
Insall-Salvati Method
Insall and Salvati59 sought a method that would fit the following requirements: (1) simple and practical, as well as accurate; (2) applicable to the range of knee positions used during routine radiography, which in the lateral view is usually 20 to 70 degrees of flexion; and (3) independent of the size of the joint and the degree of magnification of the radiograph. Because the ligamentum patellae is not elastic, its length determines the position of the patella, provided that the point of insertion into the tibial tubercle is constant.
Insall and Salvati59 describe an expression for normal patellar height in terms of the length of the patellar tendon. Measurements were made on 114 knees in which the diagnosis of a torn meniscus had been clearly established by clinical history and examination, by positive arthrographic results, and by the finding of a meniscal tear at arthrotomy. Any case in which the slightest doubt existed was excluded, and it was assumed that the joints examined were structurally normal before a traumatic episode produced a torn meniscus. All patients were adults, and none showed radiologic evidence of osteoarthritis. The following measurements were taken (see Fig. 63-11):
Measurements were repeated on bilateral knee radiographs in 50 asymptomatic volunteers by Jacobsen and Bertheussen,61 who confirmed a similar degree of accuracy. Agletti and associates also measured patellar height according to the Insall-Salvati method in a group of 150 normal knees3 (see Table 63-1). The T/P ratio was found to be 1.04 on average (range, 0.8 to 1.38; SD, 0.11). The patella was significantly higher in women (1.06) than in men (1.01). In the same group of knees, the distance from the plateau level to the tibial tuberosity and the diagonal length of the patella varied only with sex, with larger values in men than in women. In 53 knees with patellar pain, the patella was slightly but significantly higher than in normal knees, with an average T/P ratio of 1.08 (range, 0.88 to 1.29; SD, 0.09). In a group of 37 knees with recurrent subluxation, the average T/P ratio was clearly increased to an average of 1.23 (range, 0.78 to 1.60; SD, 0.18). In conclusion, according to the Insall-Salvati method, an index over 1.2 indicates patella alta, whereas an index below 0.8 indicates a low patella.
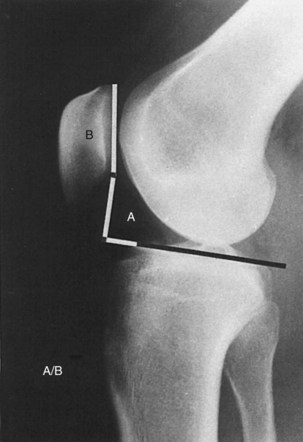
Blackburne-Peel Ratio
Blackburne and Peel14 criticized the T/P ratio on the basis of two observations:
To overcome these difficulties, the authors suggested a ratio between the perpendicular distance from the lowest articular margin of the patella to the tibial plateau (A) and the length of the articular surface of the patella (B) as measured on a lateral view of the knee in at least 30 degrees of flexion (Fig. 63-12). The A/B ratio in 171 normal knees was 0.80 (SD, 0.14). No difference between the sexes was noted.
Aglietti and associates measured the A/B ratio in a group of 150 normal knees3 and found a slightly higher value than the original authors did: an A/B ratio of 0.95 on average (range, 0.65 to 1.38; SD, 0.13), with an insignificant difference between men and women (see Table 63-1). In a group of patients with anterior knee pain, the A/B ratio was 0.91, an insignificant difference from the ratio in control knees. On the other hand, the A/B ratio was significantly increased in knees with recurrent subluxation (average, 1.08; range, 0.76 to 1.89; SD, 0.19).
Modified Insall-Salvati Ratio
Grelsamer and Meadows42 observed that the Insall-Salvati index does not account for the shape of the patella. They found that patients with patella alta and a long distal nose may have a falsely normal Insall-Salvati index. The presence of patella alta in these patients can be easily verified by indices that use the patellar articular surface and the upper part of the tibia as landmarks (the Blackburne and Peel or the Caton ratio). The variable relationship between the length of the patella and the length of the articular surface as expressed by the morphology index43 has been presented in the section on anatomy (Fig. 63-13).
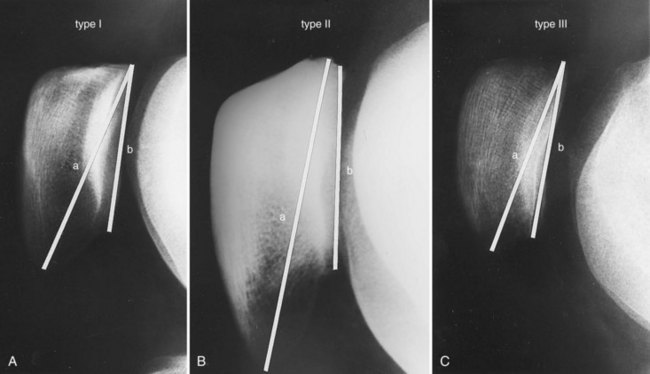
Figure 63-13 Different shapes of the patella in the sagittal plane according to Grelsamer and colleagues.43 Patellar shape is described by the morphology ratio, that is, the ratio of patellar length to length of the articular surface. A, A normal type I patella has a morphology ratio between 1.2 and 1.5. B, Type II patella, with a morphology ratio greater than 1.5, that is, with a long inferior pole (Cyrano appearance). C, Type III patella with a morphology ratio below 1.2, that is, with a short inferior pole.
To overcome the problem of variable morphology of the patella, the Insall-Salvati ratio was modified. It was suggested that the ratio of the distance between the inferior articular facet of the patella and the tibial tuberosity and the length of the articular surface be used (Fig. 63-14). In other words, this method uses the same distal reference point as the Insall-Salvati method (the tibial tuberosity) and the same proximal reference point as the Caton method. In a group of 100 control knees, the modified Insall-Salvati ratio was 1.5 on average (range, 1.2 to 2.1). Ninety-seven percent of control knees had a ratio less than 2.0. Therefore, for practical purposes, a ratio of 2 or more can be used as an index of patella alta.
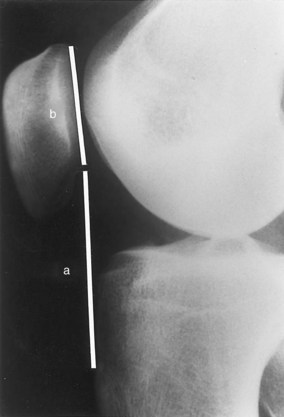
Figure 63-14 The modified Insall-Salvati method as described by Grelsamer and Meadows.42 The distance between the lowest point of the articular surface of the patella and the tibial tuberosity (distance a) is divided by the length of the articular facet (distance b). A value of 2 or more indicates patella alta.
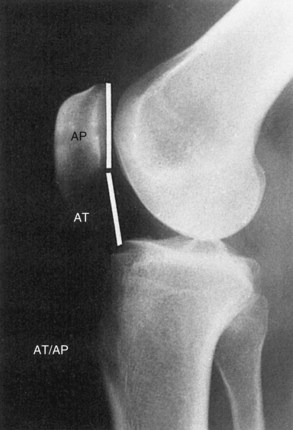
Lyon School
The Lyon School20 criticized the previously existing methods of measuring the height of the patella. Members of this group found it difficult to define the insertion of the patellar tendon into the tibial tuberosity in knees with previous transposition of the tuberosity. They further observed that the use of a tangent to the tibial plateaus in the Blackburne and Peel method14 may be a source of significant error. Perfect superimposition of the tibial plateaus is necessary to draw the line. The posterior slope of the tibial plateaus is not constant and may vary 15 degrees or more in subjects who have undergone anterior tibial epiphysiodesis. To overcome these difficulties, they tried to develop an easy method that could be used on lateral radiographs in flexion between 10 and 80 degrees and that was not influenced by radiographic magnification, by previous transposition of the tibial tuberosity, or by fractures of the tip of the patella. In this method, a ratio is calculated between the distance AT from the inferior point of the articular surface of the patella to the anterosuperior edge of the tibia and the length AP of the articular surface of the patella (Fig. 63-15). The AT/AP ratio was calculated in 141 normal subjects and was found to be 0.9607 in 80 men and 0.9906 in 61 women. Based on these findings, the authors considered the patella to be infera with a ratio of 0.6 or less and alta if 1.3 or more.
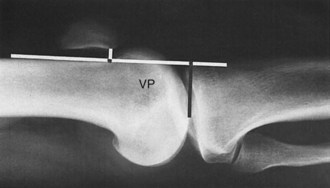
Norman Index
Norman and coworkers89 observed that the Insall-Salvati method does not describe the relationship between the patella and the femoral sulcus, and that proximal or distal transposition of the tibial tuberosity may be performed without affecting the T/P ratio. To overcome these difficulties, Norman and associates described a method wherein a lateral radiograph is obtained with the knee in full extension (hyperextension) and in quadriceps contraction to straighten the patellar tendon. The film–focus distance should be kept constant (1 m) and the cassette placed in contact with the lateral aspect of the knee. Various parameters were measured in this radiograph, including the length of the tendon, patella, and articular facet and the vertical position of the patella—that is, the distance from the lowest point of the articular facet to the joint line. These measurements were related to the height of the patient, and it was found that the vertical position of the patella was constant without sex-related differences (Fig. 63-16). The Norman index, defined as the ratio between the vertical position of the patella (in millimeters) and body length (in centimeters), is 0.21 in a normal knee (SD, 0.02). In patients with recurrent dislocation without associated generalized laxity, the index is 0.23 on average; in patients with associated generalized laxity, it is 0.25.
MRI Method
Biedert13 proposed a different method by which to evaluate patellar height based on MRI scans in extension. Measurements are taken in the central or just lateral sagittal slice, where the articular cartilage is thicker. Patellar articular cartilage is projected on trochlear cartilage, and the height of its projection is calculated. The ratio between trochlear articular cartilage height and patellar articular cartilage height is deemed the patellar index. Normal values are 12.5% to 50%. An index less than 12.5% signifies patella alta, whereas an index higher than 50% indicates patella baja. The main advantage of this method is that it takes into consideration only the articular cartilage very precisely and is not affected by the patellar tendon.
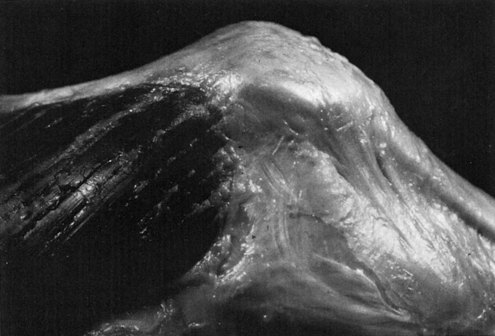
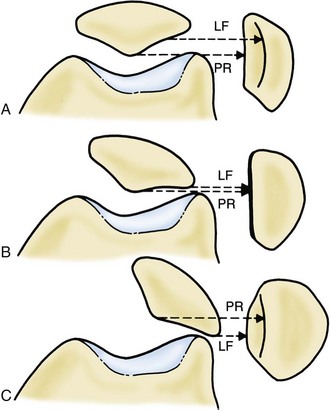
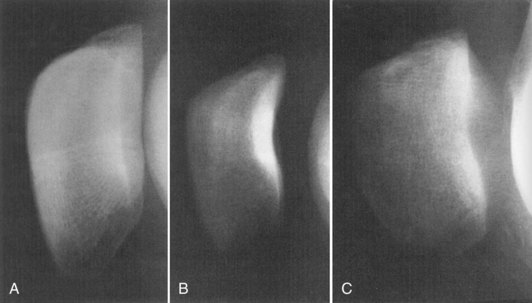
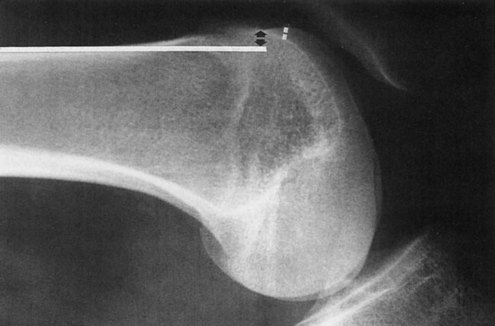
Evaluating for Patellofemoral Dysplasia
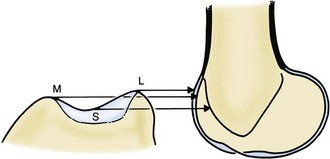
Attention has been drawn to evaluation of the anatomy of the trochlea and subluxation of the patella as seen on the lateral view. Maldague and Malghem74 first described the radiographic appearance of the patella and trochlea femoralis on lateral views of normal knees and knees with patellar instability. It is necessary to obtain lateral views with satisfactory superimposition of the posterior and distal femoral condyles, which requires the use of an image amplifier. In the lateral view of a normal knee, the posterior aspect of the patella is represented by two lines: the most posterior one is the patellar ridge, the other is the lateral facet (Figs. 63-17 and 63-18). In knees with mild lateral tilt of the patella, the two lines superimpose. When the patella is more markedly tilted, the lateral facet overhangs the patellar ridge line posteriorly, and the anteroposterior diameter of the patella is greatly increased. The normal trochlea is composed of three lines: the two anterior lines are projections of the top of the medial and lateral facets of the trochlea; the posterior line, in continuation with the intercondylar roof line, represents the deepest point of the sulcus (Fig. 63-19). The distance between the two anterior lines and the posterior line represents the depth of the sulcus. Maldague and Malghem observed that its depth is normally greater than 1 cm as it is measured 1 cm distal to the upper part of the trochlea. In knees with patellar instability, the depth of the trochlea is reduced throughout the length of the sulcus (totally deficient sulcus) or only in its upper part (focally deficient sulcus). The authors emphasized the importance of the lateral view in patients with clinically suspected patellar instability and axial views showing negative results. Because axial views are often obtained in more than 30 degrees of flexion, a lateral view taken at 15 degrees of flexion allows exploration of the patellofemoral congruence at a degree of flexion that cannot be visualized with conventional axial views.
These concepts have been carried a step farther by the Lyon School.30 Members of this group examined the lateral views of 143 knees with recurrent or acute dislocation of the patella and compared these with the radiographs of 190 control knees. They studied two quantitative measurements—trochlear bump and trochlear depth—and one qualitative sign—the crossing sign.
On a lateral view with superimposition of the femoral condyles, a line is drawn tangent to the last 10 cm of the anterior cortex of the femur. The line of the femoral sulcus may end in front of (positive value), over, or behind (negative value) the line of the anterior cortex. The distance between the anterior cortex line and the sulcus (saille or bump) is measured in millimeters (Fig. 63-20). The bump of the sulcus line in relation to the anterior femoral cortex was found to be highly useful in differentiating between knees with instability (average, +3.2 mm) and normal knees (average, −0.8 mm). A pathologic threshold value for measurement of trochlear bump was identified: 3 mm. Sixty-six percent of knees with patellar instability had anterior trochlear translation of 3 mm or more as compared with only 6.5% of control knees.
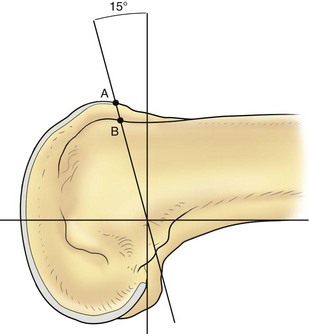
The depth of the trochlea was measured as the distance between the floor of the trochlea and the most anterior condylar contour line. First, a line tangent to the posterior cortex of the femur was drawn. A second line was drawn perpendicular to the posterior femoral cortex line and tangent to the posterior aspect of the femoral condyles. A third line was finally drawn that subtended an angle of 15 degrees to the second line and passed through the intersection of the first and second lines. Trochlear depth was measured along this third line (Fig. 63-21). Trochlear depth was 7.8 mm in the control group and 2.3 mm in knees with patellar instability. A trochlear depth of 4 mm or less was considered pathologic. This value was found in 85% of knees with patellar instability and in only 3% of controls.
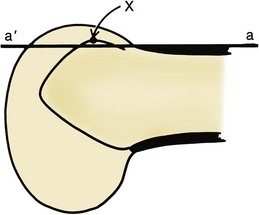
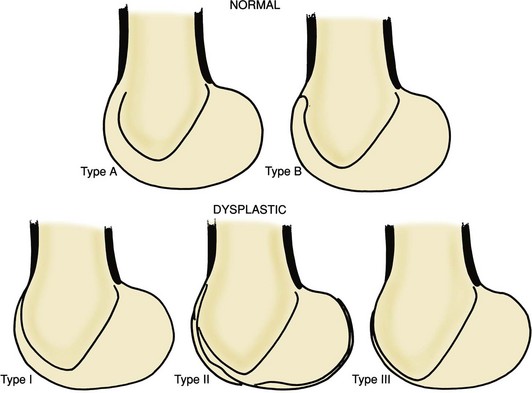
Dysplasia of the trochlea can be divided into three types according to the point at which the sulcus line crosses the lines of the condyles (the croisement, or crossing, sign) The crossing sign is a simple qualitative criterion defined as the crossing between the floor line and the lateral condylar line. At that level, the trochlea is considered flat (Figs. 63-22 and 63-23)31:
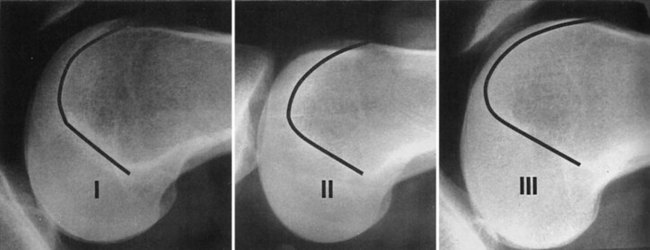
Figure 63-23 Trochlear dysplasia, types I, II, and III. See text for explanation.
(From Dejour H, Walch G, Neyret P, Adeleine P: La dysplasie de la trochlee femorale. Rev Chir Orthop 76:45, 1990.)
Two types of normal trochlea were identified:
Dysplasia of the femoral sulcus, as evidenced by the crossing sign, was present in the majority of knees with patellar instability (96%) (Fig. 63-24); the same was true in only 3% of control knees. In light of this study, the authors concluded that in trochlear dysplasia, the trochlea is flat in a zone of variable length and has a shallow groove more distally. According to the authors, trochlear dysplasia is better evaluated on a lateral radiograph than on CT. Such dysplasia is best recognized with the crossing sign, a qualitative factor that was present in 96% of knees with patellar instability. Two other quantitative measurements, trochlear bump (positive when ≥3 mm) and trochlear depth (positive when ≤4 mm), were both positive in 85% of cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree