Suprascapular Nerve Release
Recently, there has been increased interest in disorders of the suprascapular nerve. While the suprascapular nerve provides sensory branches to the acromioclavicular (AC) and glenohumeral joints, its primary function is to innervate the supraspinatus and infraspinatus muscles. During its convoluted course from the upper trunk of the brachial plexus to its distal infraspinatus branches, the nerve may be compressed at either the suprascapular notch or the spinoglenoid notch (Fig. 17.1).
As the suprascapular nerve enters the supraspinatus fossa, it passes through the suprascapular notch, medial to the base of the coracoid and under the transverse scapular ligament. Although many anatomic variations have been described, the suprascapular artery (SA) and vein classically pass superficial to the transverse scapular ligament, while the suprascapular nerve travels under the transverse scapular ligament. The course under the ligament limits excursion of the nerve and predisposes to traction injury at the suprascapular notch. As it crosses the floor of the supraspinatus fossa, the nerve provides motor branches to the supraspinatus muscle and progresses toward the spinoglenoid notch.
The spinoglenoid notch is formed by the lateral aspect of the base of the scapular spine and is roofed laterally by the spinoglenoid ligament. Because of its distal attachment to the posterior capsule, tension of the spinoglenoid ligament is a dynamic function. The ligament is most taut with the arm in adduction and internal rotation. After it passes the spinoglenoid ligament, the suprascapular nerve turns sharply medially and innervates the infraspinatus muscle with several terminal motor branches.
During its course, the suprascapular nerve is particularly vulnerable to injury at regions where local anatomy limits its excursion. While various etiologies may exist (e.g., fracture, dislocation, hardware, prominent veins, traction), the most common neuropathies encountered in clinical practice are associated with paralabral cysts and large or massive rotator cuff tears.
Suprascapular neuropathy frequently occurs in association with a superior or posterosuperior labral tear. In this scenario, labral detachment forms a one-way synovial valve creating a paralabral spinoglenoid ganglion cyst. While no critical size limit has been described, presumably the larger the cyst, the greater the mass effect and the more likely suprascapular nerve compression may result. Since the nerve compression is usually distal to supraspinatus innervation, only the infraspinatus muscle is affected. In this situation, arthroscopic treatment of the mass effect along with labral repair is all that is required (i.e., arthroscopic spinoglenoid cyst decompression combined with labral repair), and formal suprascapular nerve decompression is unnecessary (1). Aspiration alone, however, does not reliably prevent cyst recurrence and is associated with inferior outcomes compared to labral repair (2).
While suprascapular neuropathy in association with spinoglenoid cysts has been recognized for several years, recent interest in the presence of suprascapular neuropathy in association with large or massive rotator cuff tears has emerged. In contrast to compression at the spinoglenoid notch, primary suprascapular nerve entrapment at the suprascapular notch affects both the supraspinatus a nd the infraspinatus muscles. In a cadaveric rotator cuff tear model, progressive medial retraction of the rotator cuff led to increased traction and angulation of the suprascapular nerve indicating potential nerve compression (3). Recent clinical studies have suggested that suprascapular neuropathy as documented by electromyography (EMG) and nerve conduction velocity (NCV) studies may be present in nearly 30% of large to massive rotator cuff tears and contribute to both pain and muscular atrophy (4). This has led some authors to perform routine suprascapular nerve decompression at the suprascapular notch in patients with massive rotator cuff tears.
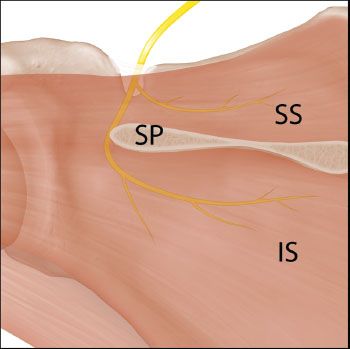 >
>Figure 17.1 Schematic of the path of the suprascapular nerve as viewed from posterior. The nerve passes through the scapular notch beneath the transverse scapular ligament and provides innervation to the supraspinatus muscle. The nerve then courses around the scapular spine to provide innervation to the infraspinatus muscle. IS, infraspinatus; SP, scapular spine; SS, supraspinatus.
SURGICAL TREATMENT
It is important to remember that not all patients with suprascapular neuropathy require surgical decompression. Most patients with neuropathy secondary to traction or overuse with no focal mass lesion, may respond well to a course of nonoperative treatment. In contrast, patients with mass lesions or massive tears of the rotator cuff may benefit from early surgical intervention to maintain muscular strength and prevent progression of muscle atrophy. Although spontaneous resolution of paralabral ganglions has been reported, only a short course of nonoperative treatment should be considered if significant neurologic deficit is detected.
It is important to remember, however, that in patients with a paralabral cyst or with a rotator cuff tear, the treatment of the primary pathology is usually all that is necessary and formal release of the suprascapular nerve may be unnecessary. For example, in patients with isolated infraspinatus involvement with a paralabral cyst secondary to a posterior or posterosuperior labral tear, arthroscopic glenohumeral decompression of the cyst, with labral repair will usually suffice. Formal decompression of the nerve is only required if EMG/NCV testing detects addition pathology (e.g., supraspinatus involvement) or if symptoms persist despite cyst decompression.
Some authors have recommended routine suprascapular nerve release in conjunction with repair of a massive rotator cuff tear based on the high prevalence of suprascapular neuropathy on EMG/NCVs in these patients. However, the benefit of this remains unproven at the time of this writing. It is our experience that routine suprascapular nerve release is unnecessary (Fig. 17.2). In fact, nerve recovery has been documented following arthroscopic rotator cuff repair without formal nerve release (4,5). Furthermore, routine suprascapular nerve release was rarely performed in conjunction with open or mini-open rotator cuff repair and its popularity has increased only recently with the description of a relatively easy arthroscopic technique. Therefore, due to the potential risk of iatrogenic nerve injury, we perform suprascapular nerve release in association with rotator cuff repair only in cases of persistent postoperative suprascapular neuropathy, or in some cases where only partial repair of the rotator cuff is possible (i.e., infraspinatus and supraspinatus are largely irreparable) and nerve traction may potentially persist. Even so, we hardly ever perform suprascapular nerve release in the case of a partial repair of a massive rotator cuff tear.
SURGICAL TECHNIQUE
Suprascapular Nerve Release at the Transverse Scapular Notch
Although once mastered arthroscopic suprascapular nerve release is a relatively quick and safe procedure, this should not be used as an endorsement for irresponsible indications for arthroscopic release. We have seen cases of severe neuropathic pain after suprascapular release and recommend judicious use of this procedure.
When indicated, we decompress the suprascapular nerve at the suprascapular notch through a subacromial approach. The subacromial space is initially viewed through a posterior subacromial portal and a standard lateral portal is established. All bursal and fibrofatty tissue is cleared off the surface of the supraspinatus and the undersurface of the acromion, and the scapular spine is exposed (Fig. 17.3). The AC joint is identified and confirmed by palpation or by using a spinal needle (Fig. 17.4A). A modified Neviaser portal is then established posterior to the AC joint (Fig. 17.4B).
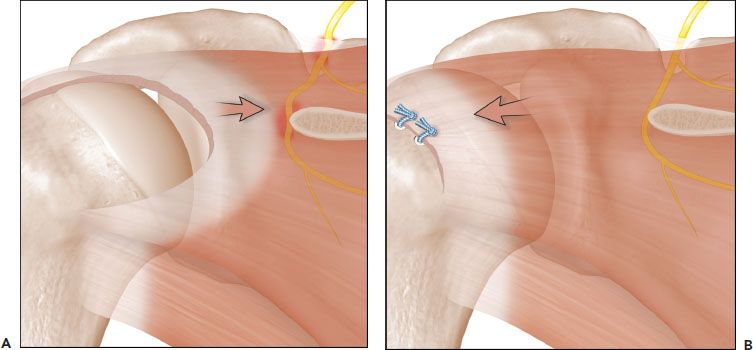
Figure 17.2 A: A massive retracted rotator cuff tear can result in compression of the suprascapular nerve at the scapular notch and at the base of the scapular spine. B: Repair of the rotator cuff tear relieves the medial compression of the nerve. The arrows denote that the muscular forces resulting in suprascapular nerve compression (A) have been reversed by cuff repair (B), thereby relieving the nerve compression.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







