CHAPTER 9 Support surfaces
1. List three limitations to the reliance of capillary closing values for support surface evaluation.
2. List four factors to consider when interpreting the significance of interface tissue pressure readings.
3. Define pressure redistribution, immersion, and envelopment.
4. Explain the difference between a reactive and an active support surfaces.
5. Compare the advantages and disadvantages of support surface categories and features.
6. List factors to consider for appropriate selection of a support surface.
A support surface is a specialized device for pressure redistribution designed for the management of tissue loads (NPUAP, 2007). Depending on the composition of the support surface and its mechanism of action, additional therapeutic functions may include reduction of shear, friction, and moisture. Support surfaces are available in different sizes and shapes and are made for chairs as well as for horizontal surfaces, such as mattresses, examination and procedure tables, operating room (OR) surfaces, and, more recently, emergency and transport stretchers or gurneys.
Although there is insufficient evidence to specify a particular brand of support surface (NPUAP and EPUAP, 2009; Whitney et al, 2006; WOCN Society, 2003, 2010), a variety of pressure-redistribution devices can help lower the incidence of pressure ulcers up to 60% (Cullum et al, 2004; Whitney et al 2006). This chapter reviews factors to consider for the (1) evaluation of support surfaces, (2) selection/evaluation of support surfaces based on individual patient assessment, and (3) creation/evaluation of a facility- or agency-wide support surface formulary. General guidance for the care of the patient requiring a support surface is given in Box 9-1.
BOX 9-1 General Guidance for Care of Patient Requiring a Support Surface
• Support surfaces alone neither prevent nor heal pressure ulcers and should be incorporated into a comprehensive individualized care plan.*
• Patient with or at-risk* for pressure ulcers should be placed on a support surface rather than a standard hospital mattress.
• Patient with or at risk* for pressure ulcers who sits should have a chair cushion and a sitting plan* that specifies frequency, duration, posture, and positioning needs.
• Support surfaces must be compatible with the care setting while meeting the individual needs of the patient.
• Support surfaces function best with minimal linens and pads under the patient.
• Patient must be able to assume a variety of positions on the selected surface (bed or chair) without bottoming out.
• Patient should be turned and repositioned regardless of support surface features.
• Multiple factors determine the frequency of repositioning* and must not be based solely on the features of the support surface.
• Use positioning devices and continence pads compatible with the support surface.
• A support surface that dissipates moisture (low air loss) may be indicated when skin barriers and dressings do not adequately protect the skin from moisture/incontinence.
• A reactive support surface with features and components such as low air loss, alternating pressure, viscous or air fluids should be considered for patients who:
• An active support surface (alternating pressure) should be considered when effective repositioning is determined by an MD to be medically contraindicated (frequent re-evaluation should be documented).
Interface tissue pressures: past and present
Interface tissue pressure is the force per unit area that acts perpendicularly between the body and the support surface and is measured by a sensor placed between the skin and support surface. This process is also known as pressure mapping (Figure 9-1). A review of 29 randomized controlled trials concluded that these measurements do not reliably predict support surface performance (Cullum et al, 2004). However, pressure mapping continues to be used to (1) produce images for product literature that appears to show pressure redistribution, (2) compare measurements from the same patient on two different surfaces, (3) assist with adjusting inflation of a chair cushion, or (4) teach a chairbound patient what type of position change will decrease pressure over an ischial tuberosity. Box 9-2 summarizes factors to consider when reviewing literature that includes interface tissue pressures (Reger et al, 1988; WOCN Society, 2003).

FIGURE 9-1 Pressure mapping device (XSensor pressure mapping system).
(Courtesy the ROHO Group, Belleville, IL.)
BOX 9-2 Capillary Closing and Interface Tissue Pressures
• Capillary closing values are based on measurements obtained from the fingertips of young healthy males.
• Pressure is three to five times greater at the bone than at the surface of the skin.
• Lower capillary closing pressures have been reported in older patients.
• Tissue interface pressures do not ensure that blood flow through the capillaries is unimpeded.
• Population tested (healthy subject will demonstrate lower pressure readings than debilitated subjects because normal muscle mass supports and distributes weight more effectively)
• How often equipment was recalibrated (sensors are fragile and may malfunction)
• Number of readings conducted per site (range based on multiple readings is more reliable than one single reading per site)
• Factors known to affect results:
Historically, support surfaces have been categorized by comparing interface tissue pressure measurements obtained on a support surface to a standard capillary closing value. Surfaces were then placed into categories called pressure reduction and pressure relief based on how close the interface tissue pressures were to the standard capillary closing value; these terms are now considered invalid (NPUAP, 2007). However, because the concept of a standardized capillary closing pressure is affected by many variables (Box 9-2) and is unlikely to exist (Le et al, 1984), attempting to employ such a simplistic scheme to guide a process as complex as support surface selection is flawed. It is more useful to formulate a framework for support surface selection that is based on such traits as physical concepts, therapeutic functions, medium, forms and features.
Physical concepts and therapeutic functions
Physical concepts are performance-related terms used to provide standard discussions about how support surfaces perform (Christian and Lachenbruch, 2007). Life expectancy refers to the period of time during which a product is able to effectively fulfill its purpose. It may be impacted by fatigue or a reduced capacity to perform due to intended or unintended use and/or prolonged exposure to chemical, thermal, or physical forces (NPUAP, 2007). Both of these factors will impact the ability of the support surface to redistribute pressure and control friction and shear.
Pressure redistribution (immersion and envelopment)
Support surfaces are designed to prevent pressure ulcers and, through pressure redistribution, provide an environment more conducive to pressure ulcer healing. Support surfaces redistribute interface pressure by conforming to the contours of the body so that pressure is redistributed over a larger surface area rather than concentrated on a more circumscribed location. The therapeutic function of pressure redistribution is accomplished through immersion and envelopment. Immersion refers to the depth of penetration or sinking into the surface allowing the pressure to be spread out over the surrounding area rather than directly over a bony prominence. Immersion is dependent on factors such as the stiffness and thickness of the support surface and the flexibility of the cover. Envelopment refers to the ability of the support surface to conform to irregularities (e.g., clothing, bedding, bony prominences) without causing a substantial increase in pressure (Brienza and Geyer, 2005; Christian and Lachenbruch, 2007; NPUAP, 2007). In contrast to the therapeutic functions of immersion and envelopment, “bottoming out” occurs when the depth of penetration or sinking is excessive, allowing increased pressure to concentrate over one area or bony prominence. Whitney et al (2006) define bottoming out as less than 1 inch of material between the surface and the skin when feeling under a support surface with the palm of a hand. Factors that may lead to bottoming out include (1) weight exceeds manufacturer’s recommendations; (2) disproportionate weights and sizes, such as with bilateral lower extremity amputation; (3) tendency to keep the head of the bed greater than 30 degrees; and (4) inappropriate support surface settings, such as over or underinflation. All support surfaces function best with less linen between the patient and the surface.
Friction and shear reduction
Friction and shear are physical concepts associated with pressure ulcer formation. Shear stress refers to force on the tissue; shear strain refers to the resulting deformation (Christian and Lachenbruch, 2007). A support surface reduces shear and friction by strategic placement of mediums and covers that allow for low-friction positioning without excessive sliding. However, the best support surface cover will not eliminate the need for additional interventions to minimize friction and shear as described in Chapters 5 and 8.
Microclimate (temperature and moisture) control
Microclimate control is a therapeutic function some support surfaces may provide. Excess moisture of the skin is a well-known factor associated with pressure ulcer development. Control of temperature at the interface surface (patient–bed boundary) helps to maintain normal skin temperature, which in turn inhibits sweating and lowers skin hydration (Mackey, 2005). A support surface should be designed to help maintain normal skin hydration and temperature (Brienza and Geyer, 2005). Porous covers help reduce moisture by allowing air to transfer between the skin and surface so that moisture and body heat can dissipate. Some mediums may be nonpermeable and prevent liquid or air to escape, whereas others interact with the body to effect microclimate, such as with continuous pumped air flowing across the skin.
Components
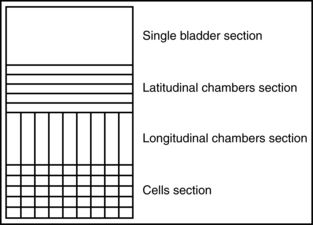
Components of a support surface are manufactured from various mediums as a means of creating pressure redistribution. Mediums are solid, fluid, and air used alone or in combination. The means of encapsulating the medium is considered another component of the support surface and is called cell or bladder (NPUAP, 2007). Multiple cells can be individual or interconnected, configured in a longitudinal or latitudinal pattern (Figures 9-2 and 9-3).
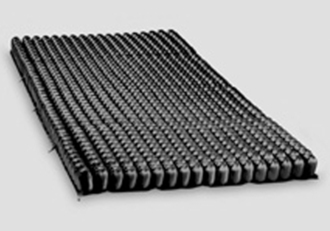
FIGURE 9-3 Nonpowered static air support surface consists of hundreds of individual air cells.
(Courtesy the ROHO Group, Belleville, IL.)
Foam
Foam can be closed cell or open cell. Closed-cell foam is a nonpermeable formulation in which a barrier between cells prevents gases or liquids from passing through the foam (NPUAP, 2007), potentially increasing skin temperature by preventing dissipation of body heat (Nicholson et al, 1999). Open-cell foam is higher-specification foam that is more effective in preventing pressure ulcers than is closed-cell foam. Examples of higher-specification foams are elastic and viscoelastic. There is no evidence that one type of high-specification foam is better than another (NPUAP and EPUAP, 2009).
Elastic foam.
Elastic is high-specification foam made of porous polymer material that conforms in proportion to the applied weight. Air enters and exits the open-cell foam rapidly due to its greater density (NPUAP, 2007). The surface continues to conform until the resistance to compression exceeds the weight being applied (Christian and Lachenbruch, 2007). The combination of density and hardness determines compressibility and conformity, ultimately establishing the ability of the support surface to mechanically redistribute loading force. Density describes foam weight, reported as either pounds per cubic foot or kilograms per cubic meter. Greater density provides more durability.
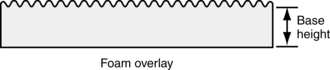
A foam overlay is a single-user form of support surface placed on a mattress. If used for pressure redistribution, an overlay should have a base height of at least 3 inches measured from the base (or bottom) to the lower level of convolution (Figure 9-4), suitable density to ensure durability (1.3–1.6 lb/ft3), IFD of 30, and ideally a ratio of 25% to 40% for compression of 2.5 or greater (Whittemore, 1998).
Viscoelastic (memory) foam.
A viscoelastic is another high-specification open-cell foam made of porous polymer material that conforms in proportion to the applied weight. Air enters and exits the foam cells slowly, which allows the material to respond slower than elastic foam. Viscoelastic foams are a subset of urethane polymer foams that exhibit a slow recovery (memory) property. A viscoelastic foam product generally has a higher density and a lower IFD. Because of their fluid nature, when an object is placed on a viscoelastic support surface, the viscoelastic tends to displace quickly and conform to the shape of the object, with low resistance. Viscoelastic foam is available in many grades and qualities, each having properties that affect pressure redistribution and microclimate performance in unique ways. Some viscoelastic foams are engineered to change hardness within a specific temperature range. These materials tend to get softer as the material warms to body temperature, resulting in conformation similar to that of a gel. Viscoelastic support surfaces are often used in the OR (AORN, 2008) and have been shown to effectively decrease the incidence of pressure ulcers in high-risk elderly patients with fractures of the neck and femur (Cullum et al, 2001). One study of 838 patients at risk for pressure ulcers found a significantly lower pressure ulcer incidence when patients were turned every 4 hours on a viscoelastic surface compared to patients who were turned every 2 hours on a standard mattress (Defloor et al, 2005).
Gel
Gel contains a network of solid aggregates, colloidal dispersions, or polymers that may exhibit elastic properties (NPUAP, 2007). Some gel products are called viscoelastic gel because they respond similarly to viscoelastic foam. Gel support surfaces are intended for multiple-patient use. Because of the consistency of the medium, gels have been found to be especially effective in preventing shear. Other advantages include easy cleaning and no electricity. Disadvantages of gel support surfaces are that they tend to be heavy and are difficult to repair. Skin humidity can increase due to the nonporous nature of the gel and the lack of air flow. Although the gel is cool upon initial contact, skin temperature may increase after hours of constant contact. Gel must be carefully monitored, and the material must be manually moved back to the areas under bony prominences if it has migrated (Brienza and Geyer, 2005).
Fluids (viscous fluid, water, air)
Viscous fluid.
Viscous fluid contains materials such as silicon elastomer, silicon, or polyvinyl (Brienza and Geyer, 2005). At first glance, viscous fluid can be mistaken for gel. Although many of its advantages and disadvantages are similar to those of gels, viscous fluid is free flowing and has a similar pressure-redistribution response as air or water. Compared to air and water, viscous fluid is thicker, with a relatively higher resistance to flow (NPUAP, 2007).
Water.
Water is a moderate-density fluid with moderate resistance to flow (NPUAP, 2007). Studies have demonstrated that water-filled support surfaces provide lower interface pressure than a standard mattress (Cullum et al, 2001). Although popular at home, water mattresses are undesirable in the hospital or long-term care setting due to multiple management concerns including the following:
Air.
Air is a low-density fluid with minimal resistance to flow (NPUAP, 2007). Air may be the sole redistribution medium, or it may be combined with other mediums (NPUAP, 2007). Support surfaces that incorporate air are available as chair cushions, overlays, mattresses, and bed systems. Most air support surfaces are easy to clean and can be reused. Air products have the potential to leak if damaged and require adequate inflation so that the body can immerse into the product. Air mattresses and overlays have the advantage of being lightweight and easy to clean.
Categories and features
Categories of pressure redistribution support surfaces include overlays, mattress replacements, integrated bed systems. Pressure redistribution may be purchased in the form of a chair cushion, transport, procedure, emergency room, or perioperative surface. All of these surfaces may be powered or nonpowered, active or reactive. Features or functional components such as low air loss, air fluidization, lateral rotation, and alternating pressure may be used alone or in combination. A variety of pressure-redistribution capabilities can exist in single or multi-zoned surfaces. A zone, is a segment with a single pressure redistribution capability. Therefore, a multi-zoned surface has different segments with different pressure redistribution capabilities (NPUAP, 2007).
Mattress overlays
The mattress overlay is a support surface that is placed on top of an existing mattress (Christian and Lachenbruch, 2007; NPUAP, 2007). Gel, water, and some air-filled overlays are intended for multiple-patient use and have the advantage of requiring much less storage space than mattresses and bed systems. Other overlays, such as foam and some air products, are for single-patient use and present environmental concerns relative to disposal of the product. Overlays are thinner than mattress replacements, so there is potential for the patient to bottom out onto the mattress below. Because they are applied over an existing mattress, mattress overlays increase the height of the bed and may complicate patient transfers, alter the fit of linens, or increase the risk for patient entrapment and falls (U.S. FDA, 2006).
Mattresses
A mattress is composed of any medium or combination of mediums that is placed on an existing compatible frame. Mattresses reduce some of the high-profile–related disadvantages experienced with overlays and appear to have fewer issues with bottoming out. When first introduced, the majority of support surfaces were rented integrated support surfaces or overlays that were rented or purchased. When support surfaces called “replacement mattresses” entered the marketplace, many facilities realized improved skin and wound outcomes by replacing their standard mattresses with replacement mattresses (Cullum et al, 2004; Gray et al, 2001). This investment reduced lead time and labor by eliminating the need to wait for delivery of bed systems or for staff to help move the patient once risk or pressure ulcers were identified. Today, some companies no longer make mattresses that do not redistribute pressure, so their standard mattress is a support surface. Mattresses may include a variety of therapeutic functions such as shear and friction reduction.
Transport, procedure, emergency room, and or mattresses.
Chapter 8 provides information related to unique risk factors specific to patients in the OR. A perioperative guidance document for pressure ulcer prevention can be found in Appendix C. The international guidelines recommend that the at-risk individual in the OR should have a mattress with pressure-redistributing properties greater than those of the standard OR mattress (AORN, 2008; NPUAP and EPUAP, 2009). However, a review of the literature suggests that, due to uncontrolled variables (e.g., reaction to anesthesia, discoveries leading to longer surgery), all surgical patients should be considered at risk and placed on a mattress with pressure-redistributing properties greater than those of the standard OR mattress (Walton-Geer, 2009). A standard OR mattress is defined as a 2-inch foam surface covered with a vinyl or nylon fabric (AORN, 2008).
A number of support surface options are available for the OR, including air, gel, and high-specification foam mattresses. The best OR surface for preventing pressure ulcers has not been determined. Therefore, selection of a support surface in the OR requires careful analysis of a number of factors to ensure the product provides pressure redistribution while demonstrating compatibility with the facility’s most common surgical positions, safety procedures, transfer equipment, and budget (Box 9-3).
BOX 9-3 AORN Selection Recommendations for Operating Room Support Surfaces
• Facilitates ability to hold patient in desired position
• Available in variety of shapes and sizes
• Ability to support maximum weight requirements
• Evidence that it can disperse skin interface pressure
• Low risk for moisture retention
• Low risk of harboring bacteria
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree