Chapter 65 Sulcus-Deepening Trochleoplasty
Normal and Pathologic Anatomy
The normal trochlea is located in the anterior aspect of the distal femur. It is composed of two facets divided by a longitudinal groove, the trochlear sulcus. The lateral facet is the largest; it extends more proximally than the medial one, and is more protuberant in the anteroposterior aspect (also referred to as higher). Proximally, the trochlea extends until the junction of the articular cartilage with the femoral anterior cortex, which is covered by adipose tissue and synovium. Distally, it is limited by the condylotrochlear grooves, one in each division of the facets with the correspondent femoral condyle. The trochlear groove extends distally and slightly laterally from the femoral axis.16
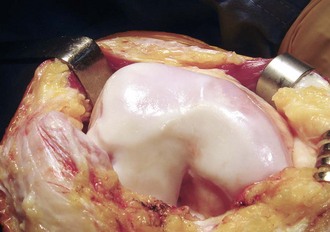
Dysplastic trochleae are shallow, flat, or even convex. It is easier to consider and define their abnormality in terms of function or deviation from the normal pattern. Radiologic features are also easier to define and measure than those observed during surgical procedures. It is common sense, however, that the surgical mark of these trochleae is their abnormal shape. A bump in the superolateral aspect is common (Fig. 65-1).
Radiographic lateral projections of normal trochleae, obtained with perfect superimposition of both femoral condyles, will typically show the contour of the facets and, posterior to them, the line representing the deepest points of the sulcus.11,12 The lateral facet is distinguished from the medial one by its more visible condylotrochlear groove and by the greater opacity to the rays of the lateral condyle. which is more perpendicular than the medial one to the x-ray beam in the lateral projection. The line representing the bottom of the groove is continuous with the intercondylar notch line, and extends anteriorly and proximally. It may end posteriorly to the condyle line (type A) or join the medial condyle line in the superior part of the trochlea (type B).7
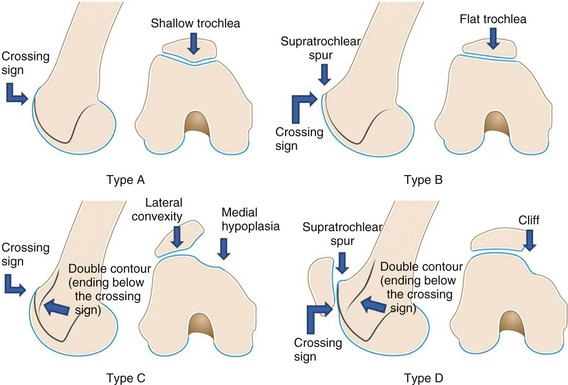
On lateral projections, trochlear dysplasia is defined by the crossing sign, where the radiographic line of the trochlear sulcus crosses (or reaches) the projection of the femoral condyles. The crossing point represents the exact location at which the floor of the trochlear sulcus reaches the same height as that of the femoral condyles, meaning that the trochlea becomes flat in this exact location. The position of the trochlear sulcus floor is also abnormal in relation to the anterior femoral cortex. Although in normal knees it is usually at a mean distance of 0.8 mm posterior to a line tangent to the anterior femoral cortex, in knees with dysplastic trochlea its mean position is 3.2 mm in front of this same line8 (Fig. 65-2).
Two other features are typical of dysplastic trochleae in lateral views, the supratrochlear spur and the double-contour sign. The supratrochlear spur is the same as sometimes visualized during surgical exposure located in the superolateral aspect. It corresponds to an attempt at containing the lateral displacement of the patella. The double contour represents the medial hypoplastic facet, seen posterior to the lateral one in this projection. Based on these signs, trochlear dysplasia may be classified into four types6,18:
Axial views obtained at 45 degrees (Merchant view) will allow the measurement of the sulcus angle. From the point of the bottom of the groove, two lines are drawn, connecting it with the most superior point of each facet. The mean normal value defined by Merchant was 138 degrees (standard deviation [SD] ± 6), and angles superior to 150 degrees are considered abnormal. Dysplastic trochleae will show higher angles, some of which cannot be measured because there is no sulcus. Alternatively, 30-degree flexion axial views will provide those measurements with better trochlear shape assessment.5 The subjective impression of the trochlear shape is important and should be taken in no more than 45 degrees of knee flexion. Greater flexion angles show the lower part of the trochlea, which is more normal. Finally, any signs of patellar instability, such as those evidenced in other projections and with other methods, serve as clues to the dysplasia diagnosis, because 96% of patients with a true patellar dislocation will present with it.8
The computed tomography (CT) scan will aid in visualizing the axial views. Three-dimensional reconstruction can also be obtained for global shape assessment. Magnetic resonance imaging (MRI) is another modality in which dysplasia is well documented. The cartilaginous shape of the sulcus can be evaluated; this is particularly interesting because the cartilaginous anatomy does not follow the underlying bony anatomy exactly.17 In dysplastic trochleae, however, bony and cartilaginous anatomies do match. Another interesting point of view is demonstrated by condylar and sulcus height measurements from the posterior condyles in axial views: the lateral facet seems to have a normal height, whereas the groove and medial facet are protuberant.4
Function and Biomechanics
To understand the principles of modifying trochlear shape, its function must be well understood. The lateral facet of the trochlea is oriented obliquely in both the sagittal and coronal planes. It deviates anteriorly and laterally from the bottom of the groove. The articulating opposed lateral patellar surface follows this orientation. The patella rests in front of the femoral cortex in total extension, but engages the trochlea in early flexion. A posteriorly directed force, the patellofemoral reaction force, pushes the patella against the trochlea and, as a result of the articulating surfaces’ configuration a medial vector is created, directing patellar tracking.2
From this brief biomechanical explanation, one conclusion is obvious—the trochlea guides patellar tracking. Not only is patellar subluxation or lateral displacement dependent on trochlear shape, but also patellar tilt. There is a high statistical correlation between patellar tilt and the type of trochlear dysplasia.18 The higher the degree of dysplasia, the higher the patellar tilt.
Procedures and Options
Three main techniques are described.
Lateral Facet–Elevating Trochleoplasty
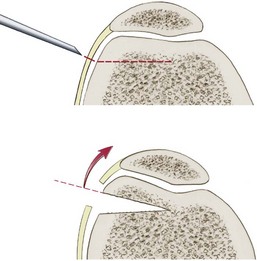
This procedure was pioneered by Albee in 1915.1 It consists of an oblique osteotomy under the lateral facet, where a corticocancellous bone wedge is interposed, with the apex medial and the base lateral. The osteotomy advances to the base of the trochlear groove, but does not disrupt it, producing a hinge in its medial aspect. The result is that it elevates the more lateral aspect of the trochlear lateral facet and also increases its obliquity, thus increasing the containment force acting on the patella. At least 5 mm of subchondral bone should be maintained to avoid trochlear necrosis (Fig. 65-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree