Subtrochanteric Fractures
EPIDEMIOLOGY
Subtrochanteric fractures account for approximately 10% to 30% of all hip fractures, and they can affect persons of all ages.
There is a greater incidence of bimodal distribution in individuals 20 to 40 years of age and in persons older than 60 years of age.
ANATOMY
A subtrochanteric femur fracture is a fracture between the lesser trochanter and a point 5 cm distal to the lesser trochanter.
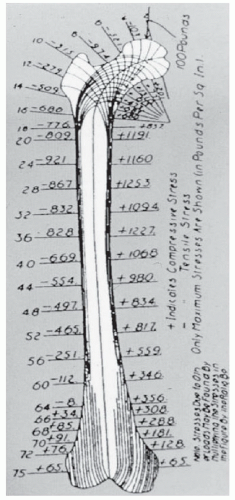
The subtrochanteric segment of the femur is subject to high biomechanical stresses. The medial and posteromedial cortices are the sites of high compressive forces, whereas the lateral cortex experiences high tensile forces (Fig. 31.1).
The subtrochanteric area of the femur is composed mainly of cortical bone. Therefore, there is less vascularity in this region and the potential for healing is diminished as compared with intertrochanteric fractures.
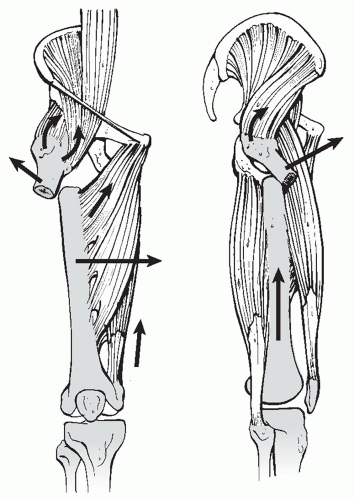
The deforming muscle forces on the proximal fragment include abduction by the gluteus, external rotation by the short rotators, and flexion by the psoas. The distal fragment is pulled proximally and into varus by the adductors (Fig. 31.2).
Mechanism of Injury
Low-energy mechanisms: Elderly individuals sustain a minor fall in which the fracture occurs through osteoporotic bone.
High-energy mechanisms: Younger adults with normal bone sustain injuries related to motor vehicle accidents, gunshot wounds, or falls from a height.
Ten percent of higher energy subtrochanteric fractures result from gunshot injuries.
Pathologic fracture: The subtrochanteric region is also a frequent site for pathologic fractures, accounting for 17% to 35% of all subtrochanteric fractures.
CLINICAL EVALUATION
Patients involved in high-energy trauma should receive full trauma evaluation.
Patients typically are unable to walk and have varying degrees of gross deformity of the lower extremity.
Hip motion is painful, with tenderness to palpation and swelling of the proximal thigh.
Because substantial forces are required to produce this fracture pattern in younger patients, associated injuries should be expected and carefully evaluated.
Field dressings or splints should be completely removed, with the injury site examined for evidence of soft tissue compromise or open injury.
A significant volume of blood from hemorrhage can be lost into the thigh. In turn, the patient should be monitored for hypovolemic shock, with invasive monitoring as necessary.
Provisional field splinting should be converted to a traction pin until definitive fixation to limit further soft tissue damage and hemorrhage.
A careful neurovascular examination is important to rule out associated injuries, although neurovascular compromise related to the subtrochanteric fracture is uncommon.
RADIOGRAPHIC EVALUATION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree