Subtotal Palmar Fasciectomy for Dupuytren’s Contracture
James W. Strickland
INDICATIONS/CONTRAINDICATIONS
Limited (subtotal) palmar fasciectomy is indicated for patients with advanced contracture of one or more digits. The procedure is designed to remove only the pathologic fascia responsible for joint contracture. Hueston applied the term regional fasciectomy to this procedure and defined it as the removal of diseased fascia within the area. Howard perhaps said it best when he wrote that surgery was indicated for the release of “bothersome contractures.”
A painful or annoying palmar nodule is rarely an indication for surgery, because the potential complications of the procedure outweigh the nuisance value of the lesion. Because metacarpophalangeal (MCP) joint deformities almost always can be corrected, surgery at this level is less urgent than that undertaken to correct developing contractures at the proximal interphalangeal (PIP) joint. At about 30 degrees of flexion, an isolated MCP joint contracture begins to become annoying to
many patients, and surgery may be appropriate. It is much more difficult to correct PIP joint contractures secondary to Dupuytren’s disease than MCP joint deformities, and the greater the magnitude of the presenting contracture, the less likely it is that significant, long-term improvement can be achieved by surgery. The author concurs with McFarlane that PIP surgery should be considered before joint contractures exceed 30 degrees.
many patients, and surgery may be appropriate. It is much more difficult to correct PIP joint contractures secondary to Dupuytren’s disease than MCP joint deformities, and the greater the magnitude of the presenting contracture, the less likely it is that significant, long-term improvement can be achieved by surgery. The author concurs with McFarlane that PIP surgery should be considered before joint contractures exceed 30 degrees.
Patients undergoing surgery for Dupuytren’s disease should be counseled carefully about the nature of the disease process and the prognosis for the additional contracture and functional impairment should they elect not to proceed with surgery. The intricacies of the operation also should be reviewed, including the possibility of complications and the need to commence early postoperative digital motion to minimize stiffness or recurrent contracture. Make every effort to identify patients who develop a postoperative sympathetic “flare” and often the author is more reluctant to proceed with surgery in these patients. It has been said that a moist, sweaty hand is a bad prognostic sign, as is the thickened hand of a laborer. Alcoholics, epileptics, and patients with Dupuytren’s diaphysis (strong family history, early onset of the disease, multiple areas of fibromatosis, ectopic fibromatosis, Peyronie’s disease, knuckle pads, or foot involvement) can be expected to do less well than patients who do not have these characteristics. In addition, there is a strong feeling that female patients are more likely to develop a postoperative sympathetic “flare” than male patients. Although the indications for surgery are generally the same in these patients, it may be appropriate to follow them longer to ensure that their disease is progressive and to consider alternative methods designed to lessen the magnitude of the operative procedure, such as subcutaneous fasciotomy or a more limited open fasciectomy.
PREOPERATIVE PLANNING
In preparation for subtotal palmar fasciectomy, drawings are made of the position and the extent of the fascial involvement, and accurate measurements of digital motion, including the extent of the MCP or PIP joint flexion contractures, should be made. In some instances, radiographs may be important to rule out any arthritic involvement of the joints one expects to mobilize during the operative procedure.
SURGERY
The author carries out all subtotal palmar fasciectomies for Dupuytren’s contracture on an outpatient basis, with the patient under axillary block anesthetic. The advantages of regional anesthesia are considerable and include the fact that the procedure produces a sympathetic blockade, which may be of value in diminishing the incidence of postoperative sympathetic “flare.” Most of our axillary blocks are done using bupivacaine so that patients will have prolonged postoperative anesthesia, which will permit them to return comfortably to their homes before experiencing any postoperative discomfort.
The axillary block is administered in a remote anesthetic area, with the provision of additional sedation depending on the patient’s desires. The patient then is brought into the regular operating room, where preparation and draping are carried out in standard fashion.
Incisional decisions are made according to the exact location of the offending fascia. If the digital cord is midline, the incisions will be centered over the midportion of the palmar digit. If the fascia is located more to the radial or ulnar side of the involved digit, incisions should be centered over the fascia rather than over the digit to lessen the amount of dissection necessary to expose the offending fascia and to decrease the often-precarious length of the digital flaps.
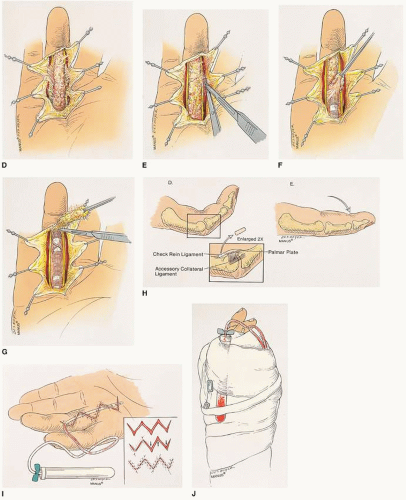
Limited fasciectomy requires wide surgical exposure of the offending fascia. My goal is to release contractures of the MCP and PIP joints fully, even if that requires concomitant capsulectomy. Incisional options include the use of a continuous Z-plasty; multiple, long zigzag incisions as described by Brunner; or shorter, Y-shaped incisions that are converted to V-shaped incisions to bring additional skin to the midline (Fig. 27-1). The zigzag incision with the Y-V closure, advocated by King and associates, has the advantage of allowing mobilization of considerable skin into the longitudinal axis of the palm and digit and is the author’s preference. There is rarely a need for skin grafting following correction of the deformity, and parallel incisions may be made if the disease involves adjacent digits.
Subtotal palmar fasciectomy is a meticulous, technique-intensive surgical procedure (Fig. 27-2A). Incisions are centered directly over the involved fascia, beginning at the proximal palm and extending to a level distal to the terminal fibers of the diseased cord. If several digits are involved, carefully planned, parallel incisions may be made continuously in the palm and digit. All incisions are drawn
on the finger at the onset of the procedure using a skin-marking pen, following which the hand and arm are exsanguinated with an Esmarch bandage, and the tourniquet is elevated to the appropriate pressure (100 to 150 mg greater than systolic blood pressure, not to exceed 300 mm Hg). Although many surgeons prefer to use a magnifying loupe, magnification of greater than ×2 may hinder dissection by limiting the surgeon’s field of vision. Magnification for Dupuytren’s fasciectomy is rarely used. Throughout the dissection, small bleeding vessels should be cauterized immediately to minimize bleeding at the time of tourniquet release. Skin flaps are dissected carefully off the underlying diseased area, and despite the intimate relationship between the fascia and its overlying skin, a satisfactory plane always can be identified. Sharp dissection with a no. 15 blade is used, and flaps are mobilized until the entire diseased cord has been exposed.
on the finger at the onset of the procedure using a skin-marking pen, following which the hand and arm are exsanguinated with an Esmarch bandage, and the tourniquet is elevated to the appropriate pressure (100 to 150 mg greater than systolic blood pressure, not to exceed 300 mm Hg). Although many surgeons prefer to use a magnifying loupe, magnification of greater than ×2 may hinder dissection by limiting the surgeon’s field of vision. Magnification for Dupuytren’s fasciectomy is rarely used. Throughout the dissection, small bleeding vessels should be cauterized immediately to minimize bleeding at the time of tourniquet release. Skin flaps are dissected carefully off the underlying diseased area, and despite the intimate relationship between the fascia and its overlying skin, a satisfactory plane always can be identified. Sharp dissection with a no. 15 blade is used, and flaps are mobilized until the entire diseased cord has been exposed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree