Subtalar Arthroscopy
John E. Femino
CLINICAL EVALUATION
History
Patients with subtalar joint pain commonly complain of the lateral hindfoot or posterior ankle pain, since most pathologies involve the posterior facet. Infrequently, medial hindfoot pain may be related to the subtalar joint. Two examples would be medial subtalar coalition and ganglion cysts from the subtalar joint causing impingement on the posteromedial soft tissue structures such as the tarsal tunnel or flexor hallucis longus (FHL).
Pain is typically worse with walking and running on uneven surfaces such as grass. Cutting sports are likely to aggravate lateral pain in the foot that is planted, since this when the subtalar joint is maximally everted, a position of subtalar joint impingement of the anterior and lateral posterior facet. Some sports, such as soccer, gymnastics, and dance, may have non weight-bearing motions that can aggravate subtalar joint problems. Pain may also be made worse with climbing stairs as this involves the extremes of ankle and subtalar motion.
A history of trauma or inversion injury is common in athletes presenting with subtalar joint problems. Inversion injury mechanisms place the subtalar joint in a position where joint congruence contributes the least to joint stability and therefore most of the joint stabilization is provided by ligamentous constraints. Under these conditions, ligamentous stabilizers can yield to excessive tensile load and result in tearing of intra-articular ligaments, which can lead to soft tissue impingement lesions.
Physical Examination
Diagnosis of pathologies around the ankle and subtalar joint can be difficult since very many structures are close together. Successful arthroscopic treatments depend on precise diagnosis of a patient’s cause of pain. Physical examination of the leg, ankle, and foot should always be performed together since many of the major soft tissue structures around the ankle and hindfoot pass longitudinally from the leg and are redirected by the retinacula and bony gliding surfaces as these structures terminate in the foot. Superficial examination of the skin, sensation, and palpation for pulses can be done by inspection and light palpation without exacerbating painful intra-articular conditions. Neurogenic causes of pain such as neuropraxia of the superficial peroneal nerve or complex regional pain syndrome, which can occur after ankle injuries, should be ruled out.
Examination of muscle strength testing the extrinsic muscles that move the ankle, hindfoot, and toes should be performed. Aggravation of symptoms with resisted active motions can help to further localize pain and reveal adjacent problems such as tendonitis or peroneal tendon instability at the superior peroneal retinaculum.
Evaluation of passive motions of the ankle, subtalar joint, and transverse tarsal joints can reveal any limitation of motion such as with a subtalar coalition.
Palpation of the ankle and foot is the key to pinpointing painful structures. Thorough knowledge of the musculoskeletal anatomy will help the examiner to identify specific painful structures beneath the skin. The ability to decipher the anterolateral ankle recess, lateral ankle gutter, and the anterior and lateral joint lines of the posterior subtalar facet is essential, yet all of these periarticular locations are within a few centimeters of each other. Impingement is a common pathology of the subtalar joint and ankle, and a positive impingement test is very helpful in localizing pain. Each joint has a unique motion that ranges from an open to a closed position. Pressure over a joint in the open position is held while the joint is moved to a closed position recreating the impingement event. Locations of soft tissue impingement include the posteromedial ankle, posterior ankle, lateral aspect of the posterior facet of the subtalar joint, anterior joint line of the posterior facet (sinus tarsi), the anterolateral ankle recess and lateral gutter, and the anteromedial ankle recess and gutter.
The impingement tests for the anterior and lateral subtalar joint posterior facet are distinct in location. The anterior subtalar impingement test is performed by placing the subtalar joint in the open position of plantarflexion and inversion. Mild to moderate digital pressure over the sinus tarsi displaces redundant soft tissue into the joint line. With digital pressure held at a constant pressure,
the hindfoot is everted while the ankle is dorsiflexed, thus closing the subtalar joint. If the patient’s stated pain is reproduced, it is typically a clear diagnosis. Occasionally, the impingement may be more subtle, and repeated gentle impingement maneuvers may recreate the pain more gradually. Crepitus can be felt at the moment of impingement and coincides with reproduction of the patient’s pain.
the hindfoot is everted while the ankle is dorsiflexed, thus closing the subtalar joint. If the patient’s stated pain is reproduced, it is typically a clear diagnosis. Occasionally, the impingement may be more subtle, and repeated gentle impingement maneuvers may recreate the pain more gradually. Crepitus can be felt at the moment of impingement and coincides with reproduction of the patient’s pain.
Flexor hallucis longus (FHL) stenosis is a condition that occurs at the level of the posteromedial subtalar joint where the posterior tibiotalar ligament attaches onto the trigonal process of the talus. This fibro-osseous tunnel can be an area of stenosis of a low-lying FHL muscle belly that occurs near the distal limit of FHL excursion in dorsiflexion of the ankle and first metatarsophalangeal (MTP) joints. Other possible causes of pain at this level include posttraumatic bony irregularity from a posteromedial tubercle fracture of the talus, an unstable or irregular os trigonum or a medial subtalar coalition. The test FHL stenosis is performed with the ankle in neutral and the first metatarsal head supported to simulate standing in foot flat stance. The first MTP joint is isolated and dorsiflexed. In cases of stenosis, this motion is severely limited to 10° or less. The limitation of dorsiflexion is resolved with ankle plantarflexion unlike hallux rigidus where there is a bony block to dorsiflexion. Palpation of FHL under tension and without tension will elicit greater pain with the tendon under tension. Posteromedial ankle soft tissue impingement can be differentiated from FHL symptoms because tension on the tendon will shield the posteromedial ankle gutter and ankle neutral open the posterior ankle joint.
Evaluation for instability of ankle and subtalar joint is performed with the patient seated and relaxed. Stability testing should be done moderately, not suddenly. The patient should be informed of the purpose of the maneuvers to avoid surprise. Sudden forceful maneuvers will often alarm patients and may elicit unnecessary pain and apprehension. The resulting splinting by the patients muscles will confound any further diagnostic examination efforts. Lateral ankle instability and subtalar joint instability can be difficult to differentiate by physical examination. Subtalar instability can be diagnosed when the ankle is stable, but is not reliably diagnosed with an unstable ankle since gross motion of an unstable ankle is much greater than the gross motion of an unstable subtalar joint. Also, the stresses for testing the two joints are similar and therefore the ankle joint instability masks instability of the subtalar joint. Testing for lateral ankle instability traditionally has been described by using two tests, anterior drawer and talar tilt. Instability, however, is actually elicited best by a combination of these forces that recreates the mechanism of injury with inversion ankle injuries. This is done by placing the stabilizing hand on the distal tibia in such a way that the long finger can be used to palpate lateral gutter of the ankle between the fibula and the talus. Anterolateral rotatory stress with inversion stress is performed with the ankle in plantarflexion. As the stress is applied, and if instability exists, the gap of the lateral gutter will be felt to widen. Comparison with the unaffected side will also make it apparent that the depth of palpation into the lateral gutter is greater than normal, indicating deficiency of the anterior talofibular ligament (ATFL). Often this stress will elicit pain and/or apprehension. Tilting of the talus with inversion stress will be pronounced with combined deficiency of the calcaneofibular ligament (CFL). Subtalar instability is identified when talar tilt alone elicits gross increase of inversion in the setting of a stable ankle. In such cases where the lateral subtalar joint opens, there is likely combined deficiency of the CFL and the interosseous talocalcaneal ligament (ITCL).
Imaging
Radiographs of foot and ankle are important for assessing the normal shape and alignment of the talus and calcaneus. Alignment of the hindfoot can demonstrate deformity such as lateral subluxation of the subtalar joint in a flat foot. Radiographs or CT scan can also demonstrate degenerative joint changes, peritalar fractures, bony irregularities such as a symptomatic trigonal process or os trigonum, subtalar coalitions, and bony variations such as an accessory facet of the lateral talar process, which can contribute to subtalar impingement in the sinus tarsi (Fig. 87.1).
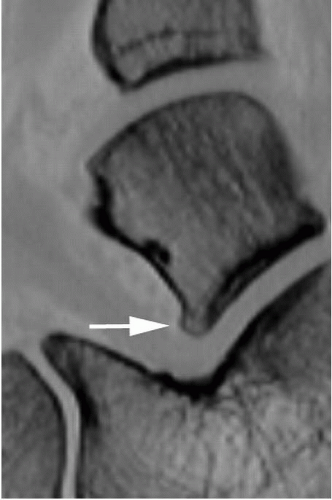 FIGURE 87.1. Arrow pointing to a small accessory facet of the lateral talar process that contributes to anterior impingement in the sinus tarsi. |
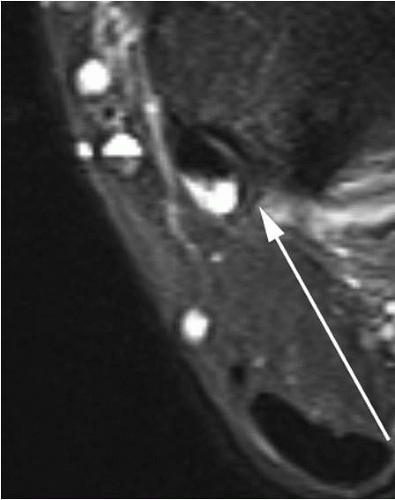
MRI is helpful for demonstrating an effusion of the subtalar joint, which is not easily seen on plain radiographs. Bone marrow edema can be seen as an indicator of bony impingement as with an accessory facet, an unstable os trigonum, or medial subtalar coalition. FHL tenosynovitis can be evidenced by increased peritendinous fluid signal behind the talus (Fig. 87.2). Peroneal tendon pathology can be assessed as well and may be included in any operative planning. MRI can also help to identify occult masses such as ganglion cysts or other tumors. Subchondral cysts or osteochondral lesions may be identified.
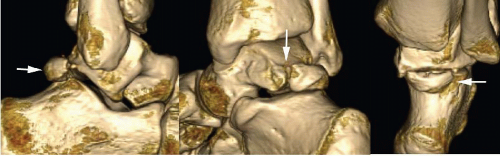 FIGURE 87.3. A sequence of three-dimensional CT reconstructions showing in detail the anatomy of an os trigonum. This is helpful in preoperative planning for prone arthroscopic excision. |
Dynamic ultrasound can be useful for evaluating causes of periarticular pain such as peroneal tendon pathology or instability.
CT scanning can be helpful in both diagnosis and preoperative planning can detect osseous abnormalities such as occult peritalar fractures and other periarticular bony irregularities, which can be amenable to arthroscopic debridement. Improving software can provide three-dimensional surface rendered CT scans to add to the precision of preoperative planning (Fig. 87.3).
Finally, intra-articular contrast can add to the level of diagnostic accuracy for some pathologies such as loose bodies. However, extravasation of dye can also hinder evaluation of some periarticular soft tissue pathologies such as FHL tenosynovitis.
TREATMENT
Nonoperative treatment of subtalar joint pain includes short-term immobilization, ice and anti-inflammatory modalities such as nonsteroidal anti-inflammatory drugs (NSAIDs) and steroid injections, all of which may calm synovitis of the subtalar joint. However, most pathologies that are amenable to subtalar arthroscopy are mechanical in nature and, therefore, are not likely to be resolved in the long term by these nonoperative means. Malalignment due to flat foot should always be considered as a possible underlying cause. Correction with custom medial forefoot posted orthoses or surgical realignment may be necessary to correct overpronation.
OPERATIVE INDICATIONS
Most patients with symptoms suggestive of subtalar joint pathology have a history of injury such as inversion injuries or fractures of the ankle, talus, or calcaneus. Therefore, many of these patients have had either operative or nonoperative treatment for their injuries, and present in a delayed fashion after reasonable efforts of nonoperative treatment. Persistent pain referable to the subtalar joint should lead to an appropriate examination and diagnostic workup. Operative indications can include synovitis,
arthrofibrosis, cartilagenous lesions, and bony impingement in the sinus tarsi, subfibular region, or posterior talar region (1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14 and 15). In addition, cases of early degenerative joint disease may not be apparent by radiographic techniques (4, 16, 15). The role of diagnostic subtalar arthroscopy should be a consideration, especially in the presence of combined ankle symptoms, such as instability and impingement (3, 4, 5, 11, 15). In most reports, the focus of treatment has centered on the sinus tarsi or anterior joint space of the posterior facet of the subtalar joint, which is the most common site of pain referable to the subtalar joint. Soft tissue impingement due to torn ligaments and/or synovitis in this area is a common diagnosis. Underlying anatomic variation of the anterior aspect of the lateral talar process may contribute to impingement due to an accessory facet in this location (17). The supine semilateral approach to the subtalar joint is the most expeditious, and consists mainly of the anterolateral and lateral portals (Fig. 87.4). In the posterior talar region there is, by nature of the anatomy of the talus, confluence of the ankle and subtalar joints. Posterior periarticular causes of pain such as an os trigonum, FHL stenosis/tenosynovitis, and different types of posterior soft tissue impingement can be approached by using a posterolateral and lateral portal (14) but are more directly seen and treated by the prone posterior arthroscopic approach, which allows more direct evaluation and treatment of posterior pathologies of the ankle and subtalar joints (Fig. 87.5) (13, 15). The immediate use of subtalar arthroscopy for fractures, such as those of the calcaneus, is an evolving and promising technique (18, 19 and 20).
arthrofibrosis, cartilagenous lesions, and bony impingement in the sinus tarsi, subfibular region, or posterior talar region (1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14 and 15). In addition, cases of early degenerative joint disease may not be apparent by radiographic techniques (4, 16, 15). The role of diagnostic subtalar arthroscopy should be a consideration, especially in the presence of combined ankle symptoms, such as instability and impingement (3, 4, 5, 11, 15). In most reports, the focus of treatment has centered on the sinus tarsi or anterior joint space of the posterior facet of the subtalar joint, which is the most common site of pain referable to the subtalar joint. Soft tissue impingement due to torn ligaments and/or synovitis in this area is a common diagnosis. Underlying anatomic variation of the anterior aspect of the lateral talar process may contribute to impingement due to an accessory facet in this location (17). The supine semilateral approach to the subtalar joint is the most expeditious, and consists mainly of the anterolateral and lateral portals (Fig. 87.4). In the posterior talar region there is, by nature of the anatomy of the talus, confluence of the ankle and subtalar joints. Posterior periarticular causes of pain such as an os trigonum, FHL stenosis/tenosynovitis, and different types of posterior soft tissue impingement can be approached by using a posterolateral and lateral portal (14) but are more directly seen and treated by the prone posterior arthroscopic approach, which allows more direct evaluation and treatment of posterior pathologies of the ankle and subtalar joints (Fig. 87.5) (13, 15). The immediate use of subtalar arthroscopy for fractures, such as those of the calcaneus, is an evolving and promising technique (18, 19 and 20).
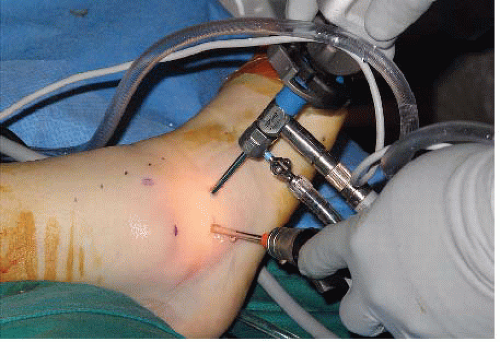 FIGURE 87.4. Supine subtalar arthroscopy is performed through the anterolateral and lateral portals providing good access to pathology in the anterior and lateral regions of the posterior subtalar facet. The lateral portal can also be used to visualize the peroneal tendons.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|