Subscapularis Repair
Florian Elser
Peter J. Millett
INTRODUCTION
Historically, the incidences of subscapularis tendon tears have been underreported, despite its importance as a major muscle of the rotator cuff and its important role in shoulder function and stability. Codman found a 3.5% involvement of the subscapularis tendon in 200 rotator cuff tears (1). More recent studies found a higher incidence of 5.8% (8/139 patients) for isolated subscapularis tears and 29.4% to 33.8% (47/139) overall involvement of the subscapularis in rotator cuff tears (2,3). The reason for the higher incidence may be that many of these tears started as partial thickness articular sided tears that were easily missed clinically and with traditional open surgical approaches.
Anatomy
The subscapularis muscle originates from the medial two thirds of the anterior scapula. It courses laterally underneath the coracoid process and inserts onto the lesser tuberosity. The muscle becomes tendinous at the level of the joint line. It is innervated by the upper and lower subscapular nerves.
The subscapularis has the largest muscle tendon unit of all rotator cuff tendons (4) and the largest footprint (5). There are several papers published in the literature on the anatomy of how the subscapularis tendon inserts on the humerus. The footprint has been described as ear shaped (6) or comma shaped (4,7). Its superior insertion is wide in the uppermost margin of the lesser tuberosity, while the superior two thirds have a tendinous insertion (8). The inferior portion inserts into the anteromedial bony anatomy of the lesser tuberosity. In this area, the tendon is shortened and the muscle almost inserts directly onto the humerus (8).
The superior glenohumeral ligament has been described as inserting proximal to the subscapularis insertion on the lesser tuberosity. More recent arthroscopic (9,10) and histologic studies (11) have shown that the humeral insertions of the subscapularis, superior glenohumeral ligament, and coracohumeral ligament appear to be attached through interdigitating fibers.
Function
The subscapularis is an internal rotator and stabilizer to the glenohumeral joint.
Subscapularis injuries can cause considerable changes in shoulder mechanics (12,13). Untreated subscapularis tears may lead to pain, loss of function, weakness (14,15), and anterior instability (12,13,16,17). Many studies have been published on subscapularis function. Burkhart et al. (18) showed that the subscapularis and its moment balance the transverse force couple, which is important to provide a stable fulcrum for glenohumeral motion. Neviaser et al. (19) highlighted the role of subscapularis tears in shoulders with recurrent instability after traumatic dislocations.
Therefore, it is important to surgically address repairable subscapularis tears.
Etiology
The mechanism of subscapularis tendon injury has been reported to be mainly traumatic in nature. Traumatic injury usually occurs with the arm with hyperextension or external rotation of the abducted arm (20).
This is in contrast to the history of microtrauma and early nonspecific onset of symptoms that are frequently seen with degenerative rotator cuff tears involving the supraspinatus or infraspinatus tendons.
It has been suggested that a narrowed coracohumeral interval (21) and conditions that allow the biceps tendon to subluxate anteriorly (9,22) may be a cause for subscapularis tendon tears.
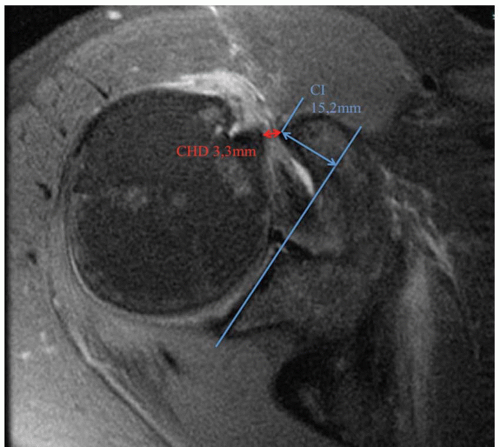
The coracohumeral interval is the distance between the tip of the coracoid and the nearest cortex of the lesser tuberosity (Fig. 15.1). There is no evidence in the literature how humeral head rotation influences these distances.
Richards et al. (21) found a significant relationship between a narrowed coracohumeral distance (CHD) and subscapularis pathology (10 ± 1.3 mm vs. 5 ± 1.7 mm).
A study recently by Millett et al. presented at arthroscopy association of north america (AANA) showed significant correlations between subcoracoid space narrowing and rotator cuff tears, including supraspinatus (p = 0.008) in 94 patients. Complete rotator cuff tears had smaller CHDs (9.6 mm) compared to partial tears (11.2 mm) and no tears (12.3 mm).
DIAGNOSIS
History
Subscapularis pathology diagnosis can often be difficult. However subscapularis tears, especially traumatic tears, can be evident from the history alone. Sudden onset of symptoms (weakness, pain) after a hyperextension or external rotation trauma of the abducted arm indicates subscapularis pathology. Traumatic glenohumeral dislocations in individuals older than 40 years of age also have a strong association with rotator cuff tears, especially subscapularis tendon tears. Further recurrent anterior instability can be caused by rupture of the subscapularis and anterior capsule. Patients with prior open surgical history, where the subscapularis has been taken down, are also at higher risk for subscapularis pathology.
Patients with intrinsic degeneration of the tendon and degenerative tears typically present with limited shoulder function due to pain and weakness. Recurrent anterior shoulder dislocations can also be associated with subscapularis tears (19).
Clinical Examination
Patients with full thickness subscapularis tears may present with an increased external rotation on the affected side and no defined end-point on external rotation.
Clinical tests for detecting tears or dysfunction of the subscapularis are the lift-off test (20) and the belly-press test (23), both described by Gerber and coworkers. The Napoleon test described by Schwamborn and Imhoff (24), the belly-off sign described by Scheibel and Habermeyer (25), and the Bear-Hug test described by Barth et al. (2) are also useful.
Clinical examination should include more than one test to optimize the chance of detecting subscapularis tears. The authors prefer to perform both the belly-press and the lift-off test because they are reliable clinical tests. Performing a lift-off test, the patient’s hand of the affected side is placed on the back. The test is
considered positive, if the patient is unable to lift the arm posteriorly off the back. For the belly-press test, the arm is positioned at the side with the elbow flexed at 90 degrees. The patient is asked to press the palm onto the abdomen by internally rotating the shoulder. The test is considered positive if the patient shows a weakness in comparison to the opposite shoulder or if the force is not achieved by active internal rotation but elbow or shoulder extension.
considered positive, if the patient is unable to lift the arm posteriorly off the back. For the belly-press test, the arm is positioned at the side with the elbow flexed at 90 degrees. The patient is asked to press the palm onto the abdomen by internally rotating the shoulder. The test is considered positive if the patient shows a weakness in comparison to the opposite shoulder or if the force is not achieved by active internal rotation but elbow or shoulder extension.
Positive bear-hug and belly-press tests suggest that the tear size is at least 30%, a positive Napoleon test suggests that the size is at least 50%, and a positive lift-off test suggests that the tear size is at least 75% of the subscapularis (2).
Imaging
As a first step, plain radiographs in three planes are recommended to rule out bony alterations, degenerative changes, or calcification of the rotator cuff tendons. Patients with isolated subscapularis tears usually have a normal bony radiographic anatomy, but an anterior subluxation might be present in the axillary view. In rare instances, coracoid abnormalities such as subchondral sclerosis or a positive coracoid index (CI) might be present. The CI (26) is measured on axial cross section images (CT, magnetic resonance imaging [MRI]). It describes the lateral projection of the tip of the coracoid beyond a tangential line to the articular surface of the glenoid (Fig. 15.1). The average index in 67 nonsymptomatic shoulders was 8.2 mm (26).
The gold standard for imaging of soft tissue pathologies of the shoulder girdle is MRI. Studies have proven a high sensitivity and specificity of MRI in detecting the presence or absence of full-thickness rotator cuff tears, ranging from 84% to 100% and 93% to 99%, respectively (27, 28, 29, 30, 31, 32, 33, 34, 35). Newer studies have shown that high-quality MRI scans are even able to predict tear patterns (36), which enables the surgeon to better plan the procedure.
In every MRI, the muscle quality should be evaluated. Flury et al. (37) found that advanced fatty degeneration stages 3 and 4 (Goutallier Grading System of Fatty Degeneration of Muscle, 38) are associated with a significant increase in rerupture rate after subscapularis repair.
In a postoperative setting, the diagnosis and imaging of subscapularis retears are more difficult. Especially the differential diagnosis to subscapularis dysfunction due to denervation or nerve injuries can be challenging. When in doubt, additional neurologic examinations have to be performed before revision surgery.
TREATMENT
Surgical Indications
Early operative management with primary tendon repair has been shown to yield reproducible results (23), whereas chronic tears lead to muscle atrophy and retraction of the tendons. Ticker and Warner (39) found that tears repaired more than 1 year after the injury have frequent repair failures because of severe muscle degeneration. Other studies also showed that a delay from the time of injury to the time of operative repair may cause decreased quality of results (23,37




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree