Chapter 8
Strength training
In people with spinal cord injury, the performance of motor tasks can be limited by the strength of completely paralysed, partially paralysed or non–paralysed muscles. For example, a patient with thoracic paraplegia may be unable to transfer from floor to wheelchair because of complete paralysis of the lower limbs and poor strength in the upper limbs (see Figure 8.1). The obvious impairment in this case is paralysis of the lower limbs. However, paradoxically paralysis of lower limb muscles is of little immediate interest to physiotherapists because strengthening programmes cannot induce neurological repair following complete spinal cord injury. Instead, physiotherapists are primarily interested in the strength of the neurally intact upper limb muscles, notably the triceps and latissimus dorsi muscles. These upper limb muscles are not directly affected by spinal cord injury nor are they necessarily any weaker than the upper limb muscles of most able-bodied individuals. However, ‘normal’ upper limb strength is typically not sufficient to lift the entire body weight off the floor. To master this motor task, patients need to develop strength over and above that typically required by able-bodied individuals. Upper limb strength may be an even greater problem in patients who are deconditioned from extended periods of prior bedrest or who are overweight. The appropriate intervention is a strengthening programme which specifically targets the ability of the triceps and latissimus dorsi muscles to generate force.

Often the performance of motor tasks is limited by strength of partially paralysed muscles.1 For example, a patient with C6 tetraplegia may have partial paralysis of the pectoralis muscles due to damage of some, but not all, motor neurons innervating the pectoralis muscles. Weakness of the pectoralis muscles may limit shoulder horizontal adduction and hence prevent rolling in bed (see Chapter 3). Likewise, a patient with incomplete paraplegia may have partial paralysis of the tibialis anterior muscles, and therefore may be unable to hold the ankle dorsiflexed during the swing phase of gait. In these examples, the appropriate intervention is a strengthening programme for the partially paralysed muscles.
The performance of motor tasks can also be limited by muscle power. Power refers to the amount of work done over a specified period of time.2 For example, lifting a set weight rapidly requires more muscle power than lifting the same weight slowly. Muscle power is important for motor tasks which need to be done at high speed. In the able-bodied population, the vertical jump is commonly provided as a good example of a task requiring high levels of lower limb power.3 There are comparable tasks for patients with spinal cord injury where large forces need to be generated at high speeds.2 For instance, pushing a manual wheelchair up a slope or jumping up steps with bilateral knee–ankle–foot orthoses requires upper limb power.
Small changes in strength, power and endurance can have important implications for the ability to perform motor tasks, particularly in patients with tetraplegia. For example, a small increase in the strength of the shoulder flexor muscles of a patient with C5 tetraplegia can make the difference between attaining and not attaining independence with feeding (see Chapter 5, Figure 5.3). A subtle increase in wrist extensor strength of a patient with C6 tetraplegia can make the difference between useful and very limited hand function.4 Similarly, small changes in lower limb strength can have implications even for very weak patients unable to walk. The ability to move the legs even slightly can make it easier to transfer.
The broad aims and approaches to physiotherapy are similar regardless of whether the problem is one of strength, power or endurance and regardless of whether the problem is with partially paralysed or non-paralysed muscles. In all cases, the focus of training is driven by an analysis of task performance (see Chapter 2). This determines which muscles are targeted and how training is best structured.
Assessment of strength
Manual muscle test
Manual muscle tests have traditionally been used by physiotherapists to measure strength of patients with spinal cord injury. There are numerous variations in the way manual muscles tests are performed.5 One type of manual muscle test rates strength of individual muscles (e.g. the brachioradialis and brachialis)6 and another rates strength of muscle groups (e.g. the elbow flexor muscles).7 Strength is usually assessed on either a six-point8 or 11-point scoring system, although there are variations on these systems.6 For example, the original six-point scoring system is sometimes used with transitional grades (‘plus’ and ‘minus’ grades). Some physiotherapists replace the numeric scales with descriptors such as ‘trace’, ‘poor’, ‘fair’, ‘good’ and ‘normal’ (see Table 8.1). To add further confusion, sometimes grade 4/5 and 5/5 strength is tested with resistance applied as patients move through full range of motion,8 and at other times these higher grades are tested with resistance applied during an isometric contraction.6 A range of testing positions are used, and these are documented in several classic texts which describe manual muscle test protocols.8,9 The manual muscle test used as part of the ASIA assessment is yet another variation. The ASIA assessment uses the six-point scale but all testing is conducted with the patient in the supine position.10 In the ASIA assessment only 10 muscles representing the C5 to T1 and L2 to S1 myotomes are tested (see Chapter 1 for details).
Table 8.1
Different ways of scoring results of manual muscle test
| Descriptive scoring system | 6-point scoring system | 11-point scoring system | Definition | |
| Normal | N | 5 | 10 | Full available ROM, against gravity, strong manual resistance |
| Good plus | G + | 4 + | 9 | Full available ROM, against gravity, nearly strong manual resistance |
| Good | G | 4 | 8 | Full available ROM, against gravity, moderate manual resistance |
| Good minus | G– | 4– | 7 | Full available ROM, against gravity, nearly moderate manual resistance |
| Fair plus | F + | 3 + | 6 | Full available ROM, against gravity, slight manual resistance |
| Fair | F | 3 | 5 | Full available ROM, against gravity, no resistance |
| Fair minus | F– | 3– | 4 | At least 50% ROM, against gravity, no resistance |
| Poor plus | P + | 2 + | 3 | Full available ROM, gravity eliminated, slight manual resistance |
| Poor | P | 2 | 2 | Full available ROM, gravity eliminated, no resistance |
| Poor minus | P– | 2– | 1 | At least 50% ROM, gravity eliminated, no resistance |
| Trace plus | T + | 1 + | Minimal observable motion (less than 50% ROM), gravity minimized, no resistance | |
| Trace | T | 1 | T | No observable motion, palpable muscle contraction, no resistance |
| Zero | 0 | 0 | 0 | No observable or palpable muscle contraction |
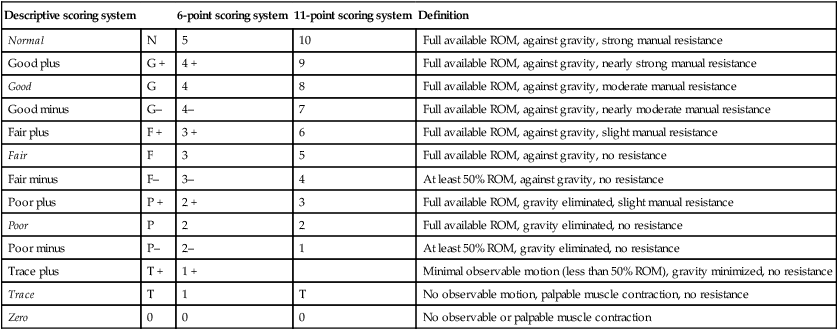
From White DJ: Musculoskeletal assessment. In O’Sullivan SB, Schmitz TJ (eds): Physical Rehabilitation: Assessment and Treatment, 5th edition. Philadelphia, FA Davis, 2007, Table 6.6, p. 181, with permission.
The results of manual muscle tests correlate broadly with more objective measures of strength.11,12 For example, patients with grade 4/5 strength attain higher dynamometric measures of isometric strength than patients with grade 3/5 strength. However, this conceals an important limitation of manual muscle tests identified over 50 years ago,13 namely their poor sensitivity. This is particularly apparent with grade 4/5 and 5/5 strength.4,14–20 Grades 4/5 and 5/5 encompass a much wider range of strengths than that encompassed by grades 0/5 to 3/5. Consequently, two patients with grade 4/5 strength can have clinically important differences in strength. As a result, manual muscle tests are of limited use for testing strength of stronger patients.17 Manual muscle tests also have limited use in patients with marked spasticity.19 It is often difficult to distinguish between voluntary strength and spasticity, especially if spasticity is elicited with attempts at movement during testing.
The frequency with which manual muscle tests are performed is often determined by hospital protocols. Muscle tests may need to be done daily, or sometimes even several times a day if a patient’s neurological status is rapidly changing. However, once neurological status has stabilized manual muscle tests can be done less frequently. For example, after the acute phase, it may be appropriate to perform manual muscle tests every 3–4 weeks and thereafter every 3–4 months. Once patients have been discharged from rehabilitation, manual muscle tests are performed less frequently and primarily used to monitor neurological status and detect neurological complications such as syringomyelia.21 Syringomyelia can occur many years after injury and lead to loss of strength, typically in the myotomes immediately above the level of the injury.
One repetition maximum
Strength can by assessed by determining the ‘one repetition maximum’ (1 RM).22,23 This test is appropriate for muscle groups with grade 4/5 and 5/5 strength. One repetition maximum refers to the maximum weight a patient can lift through an entire range of motion against gravity. The physiotherapist initially estimates a weight which the patient will only just be able to lift. The patient attempts to lift that weight. If the weight can be lifted two or more times it is less than the true 1 RM. If it cannot be lifted at all with a maximum effort it is greater than the 1 RM. Testing involves adjusting the weight until it can be lifted but not more than once. This weight is the 1 RM. It is important that patients receive sufficient rest between each attempt to avoid fatigue.23,24 Testing the 1 RM of multiple muscles can be time-consuming and may need to be done over two or more occasions.
To determine the 1 RM of most upper and lower limb muscles, the weight is secured to the wrist or ankle, commonly with wrap-around velcro weights (see Figure 8.2a). For the upper limbs, a dumbbell can be held in the hand if patients have sufficient grasp (see Figure 8.2b). Alternatively, a weight and pulley system can be used (see Figure 8.2c). When using a weight and pulley system to assess 1 RM it is important to ensure the line of pull is reproducible on subsequent tests; this is best done by ensuring that the line of pull is perpendicular to the limb when halfway through range of motion. The weight a patient can lift using a weight and pulley system does not correspond with the weight a patient can lift using a dumbbell because the same weight generates a different torque when lifted in the two ways.
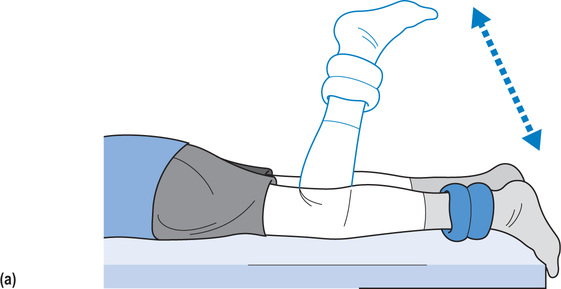

A ‘modified’ 1 RM can be used to measure strength in muscles with grade 3/5 or less strength. Instead of lifting a weight against gravity, the patient moves a weight horizontally. The limb is supported using slideboards or overhead suspension (see Figure 8.6). Alternatively, devices can be used which counteract the weight of limbs, enabling very weak patients to move in anti-gravity positions (see Figure 8.7).
Hand-held myometers
Strength can also be measured with hand-held myometers. Myometers are small portable devices used to test isometric strength (see Figure 8.3).4,14,15,25,26 There are mechanical and electronic versions. All provide measures of force, not torque. Reliability is dependent on replicating the position of the patient, the position of the myometer and the angle at which the force is directed through the myometer.25–31 Myometers are more difficult to use in stronger patients because physiotherapists cannot always provide adequate resistance and stabilization especially when testing the larger lower limb muscles.16,30,32 Hand-held myometers are useful for testing strength in patients confined to bed, although it is not always possible to test all muscles. For example, it is not possible to test the strength of the hip extensor muscles in patients restricted to the supine position.
Isokinetic dynamometers
Isokinetic dynamometers measure torque during dynamic (concentric or eccentric) contractions at a constant angular velocity.16,32,33 They are not commonly used in spinal cord injury units because the equipment is expensive, not easy to adjust when testing many muscle groups, and not appropriate for patients with profound weakness or patients restricted to bed.2,16
Neurally intact muscles
Most of what is known about strength training of neurally intact muscles comes from studies in healthy able-bodied individuals. These studies indicate that training typically increases strength by approximately 2% per week.34,35 Gains in strength are greater during the early stages of training, especially in previously deconditioned individuals. However, strength continues to improve over extended periods of time if training is sustained. Males and females of all ages benefit in a similar way from strength training.34,36,37
Training increases muscle fibre cross-sectional area and leads to muscle hypertrophy. These changes are well correlated with increases in strength. Training also induces other morphological and histochemical changes. For example, it changes the protein content of muscles, increases the density of capillaries and prompts fibre type conversion.22,38–40 Improvements in strength with training may also be due to better motor unit synchronization, firing and recruitment.41–51 Evidence to support these types of neural adaptations come from studies demonstrating increases in strength of untrained limbs in response to imagined training49 or training of contralateral limbs.44–46,52 At least with short-term training it is thought that increases in strength are not due primarily to muscle hypertrophy. Instead increases in strength have been attributed to improvements in synchronization, firing and recruitment of motor units.46 These neural adaptations may be due to changes within the spinal and supraspinal sensorimotor networks.43,45,46,52
Progressive resistance training
Strength is best improved with progressive resistance training. The key aspects of progressive resistance training are resistance, repetition and progression.53 The optimal resistance is equivalent to an 8–12 repetition maximum (RM). This means that if training involves lifting dead weights the weight needs to be adjusted so that after 8–12 lifts the patient cannot possibly lift the weight again.54,55 This weight is normally equivalent to about 60–80% of a 1 RM.41,55,56 In a training session the patient should repeatedly lift this weight 8–12 times. Typically, the patient would then rest for 1–3 minutes before repeating the process a second and third time. The whole process should be repeated two to three times a week.41,57 As the patient gets stronger the weight is increased (that is, training is ‘progressed’). The patient should not be able to lift the weight more than 8–12 times.
These principles of progressive resistance training can be applied to most types of strengthening programmes, regardless of whether the exercise involves lifting weights, using isokinetic strengthening equipment, pulling on theraband22 or practising motor tasks (see Figure 8.2).
There is considerable debate and research around subtle questions relating to optimal protocols for progressive resistance training.22,53–55,58–61 For instance, while most advocate multiple sets within a training session, one review argues that there is now sufficient evidence to indicate that one set is equally effective.61 Some evidence suggests that training with long rests between sets (3 minutes) is superior to training with shorter rests (40 seconds), that eccentric strengthening is superior to concentric strengthening41,62,63 and that varying the load between sessions is better than fixing the load.64,65 Similarly, there is some evidence that the speed at which the weight is lifted may be important.53,60,66,67 These controversies have not yet been resolved, but there remains broad agreement that regular, progressive high-resistance exercise is needed to increase strength. Such programmes continue to be recommended by the American College of Sports Medicine.57
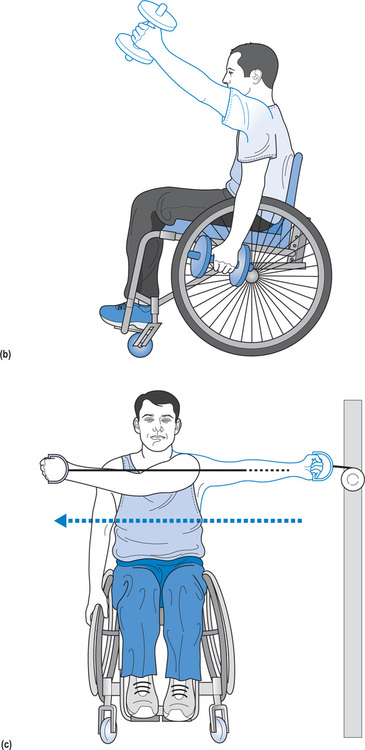
Specificity of training
The effects of progressive resistance training are specific to the way training is performed. That is, strength training will be most effective when it closely mimics the way muscles are required to generate torque. This includes mimicking factors such as the need for co-contraction, the position of the joint, the type (i.e. eccentric, concentric or isometric) and speed of contraction.41,68 For this reason strength training for a particular functional task is best done as far as possible within the context of that specific motor task. For instance, upper limb strength training aimed at increasing the ability of patients with paraplegia to get from the floor into a wheelchair could involve lifting upwards and backwards from a small stool positioned in front of the wheelchair or lifting sideways between two stools (see Figure 8.4a,b). Weaker patients can practise lifting their body weight in long-sitting, with or without externally applied resistance.69 As the patient becomes stronger strength training can be performed during practice of the whole task. That is, by moving between the floor and wheelchair. Strengthening in this way helps ensure that training targets the right muscles and involves muscle contractions at the speeds and muscle lengths required for the motor task.41,68 For example, it strengthens muscles used for stabilization which might otherwise be neglected in a training programme consisting solely of lifting weights.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









