Fig. 21.1
Factors affecting range of motion after total knee replacement
21.2 Patient Factors
The patient-related factors that have been reported to negatively affect the result after TKR – particularly pain and/or stiffness – are shown in Table 21.1 [3, 15, 19, 26, 27]. Limited preoperative ROM is considered to be the most important risk factor for postoperative stiffness.
Table 21.1
Patient factors affecting range of motion after total knee replacement
General | Diabetes mellitus |
Juvenile rheumatoid arthritis | |
Ankylosing spondylitis | |
Poliomyelitis | |
Lung disease | |
Specific | Limited preoperative ROM |
Multiple previous surgeries | |
Limited degree of preoperative osteoarthritis on X-ray | |
Patella baja | |
Young age | |
Obesity | |
Extensor mechanism and capsule contracturePosttraumatic osteoarthritis Previous septic arthritis | |
Female gender | |
Complex regional pain syndrome type 1 (CRPS-1) | |
Patient personality factors (low pain threshold, higher than normal depression state, and low compliance/motivation) |
Limited preoperative ROM is the most important patient-related risk factor for postoperative stiffness. Other relevant risk factors are previous surgeries, comorbidities, and the patient’s work status.
Stiffness after TKR can also be the result of extensor mechanism and capsule contracture, posttraumatic osteoarthritis, or previous septic arthritis [3, 8]. For successful surgical treatment of a stiff TKR, the quadriceps muscle must be able to elongate to allow motion. In case of a permanently contracted and atrophic quadriceps mechanism, treatment will therefore not be successful. Previous surgery, i.e. the multi-operated knee, is also an important risk factor [7]. Furthermore, various more general pathologies can play a role (diabetes mellitus, juvenile rheumatoid arthritis, ankylosing spondylitis, poliomyelitis, and lung disease) [7, 24, 27–29]. Heart disease and hypertension do not seem to affect the final outcome after TKR nor do alcohol, preoperative narcotic, and NSAID [29]. Body mass index is not strictly related to postoperative ROM, but a large soft tissue mass of the leg, as seen in morbid obesity, will logically limit flexion due to impingement of the soft tissues in the popliteal fossa. For age, a higher incidence of postoperative stiffness has been reported in younger patients undergoing TKR [29, 30]. Work status also seems to have an effect; patients with disability or not working due to pain were 5.8 times more likely to have stiff knees and poor results [17].
21.3 Surgical Errors and Mechanical Factors
Surgical technique errors and mechanical factors are the most frequent causes of the postoperative stiff TKR (Table 21.2) [6, 8, 24, 26, 31, 32]. The former includes patellar problems, inadequate soft tissue balancing with flexion–extension gap mismatch, component malpositioning, component oversizing, and joint line elevation resulting in patella baja. The latter includes aseptic loosening (Fig. 21.2).
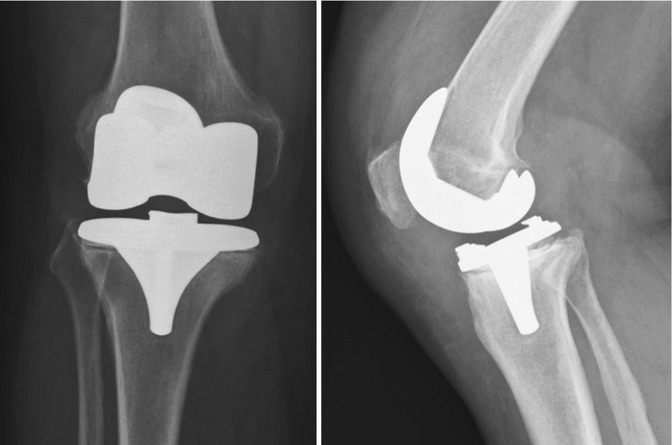
Table 21.2
Surgical technique errors and mechanical factors affecting range of motion after total knee replacement
Early-onset | Flexion loss | Due to tight flexion gap |
Incorrect ligament/gap balancing | ||
Too tight PCL (CR TKR) | ||
Lack of tibial slope | ||
Patella baja (due to iatrogenic elevation of joint line) | ||
Malpositioning (e.g. femoral component: too posterior or hyperextension) | ||
Oversizing (esp. femoral component) | ||
Overstuffing of patellofemoral joint | ||
Other factors: arthrofibrosis, inadequate rehabilitation, joint infection, or heterotopic ossification | ||
Extension loss | In early phase due to | |
Joint swelling | ||
In the chronic phase due to | ||
Tight extension gap following incorrect bone cuts (overstuffing of the extensor space (e.g. undersized femoral component and thicker tibial insert)) | ||
Inadequate distal femur resection | ||
Inadequate posterior osteophytes resection | ||
Incorrect posterior capsule release (especially in severe fixed flexion contractures) leading to improper correction of preoperative flexion deformity with a tight PCL or posterior capsule | ||
Component malposition (e.g. flexed femur, anterior sloped tibia) | ||
A too thick insert | ||
Flexion and extension loss | Usually: poor rehabilitation or arthrofibrosis | |
Sometimes: malrotation, malalignment, joint line elevation, tight PCL (CR TKR), or joint infection | ||
Late-onset | Joint infection | |
Loosening | ||
Component failure/breaking | ||
Patellar tendinitis | ||
Synovitis (particle wear debris, failure implant, or rheumatoid arthritis) |
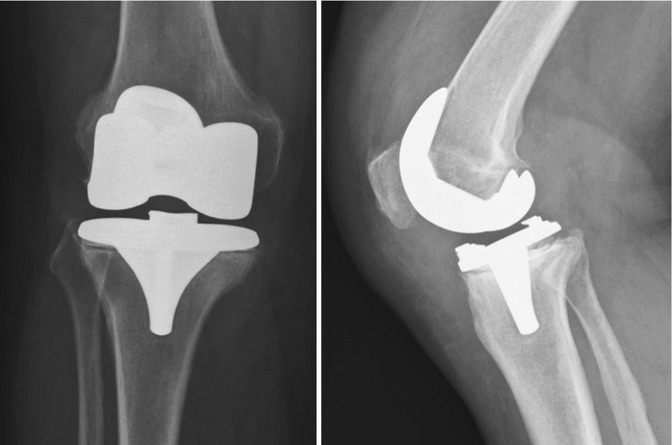
Fig. 21.2
Right total knee replacement with early tibial component loosening. Periprosthetic joint infection work-up was negative (blood serology and synovial fluid analysis). Clinically, there was pain on weight bearing and a flexion up to 80° due to pain around the proximal tibia. Tibial revision was performed and the patient was very satisfied. Flexion improved to 110° and there was effective pain relief
Surgical technique errors and mechanical factors are the most frequent causes of the postoperative stiff TKR.
Patellofemoral joint problems have been reported as an important reason for pain after TKR and the reason for revision in up to 55 % of patients [4, 33]. Reported causes of stiffness, particularly flexion problems, include localized fibrosis (clunk syndrome), patellofemoral overstuffing, true patella baja (actual shortening of the patellar tendon, mainly due to scar tissue [54]), pseudo-patella baja (iatrogenic joint line raising/proximalization [54]), lateralized patellar component, unresurfaced patella (can lead to symptomatic patellar chondrolysis), and patellar tilt or (sub)luxation due to patellar instability and/or component malpositioning. Patellofemoral overstuffing, i.e. an excessive “patellofemoral” thickness, can be the result of a too anteriorly placed femoral component (in case of posterior referencing), a too thick patella component, or femoral component oversizing.
A tight flexion space, e.g. due to tight posterior cruciate ligament (PCL) in cruciate-retaining (CR) TKR, can cause pain (generally posterior knee pain at the endpoint of flexion) and stiffness (compromised flexion). If the PCL is tight, a premature rollback occurs during flexion, hinging the joint open and limiting the degree of maximal flexion. This can also be the result in cases of excessive proximalization of the joint line [34], as illustrated in Fig. 21.3. Conversely, a too loose (or insufficient) PCL can cause excessive anterior translation of the femur resulting in an impingement of the extensor mechanism and posterior impingement of the femur on the tibia [35]. The clinical complaint generally includes anterior knee pain; this should therefore not be mistaken for symptomatic patellar chondrolysis. Excessive femoral component size and/or flexion may cause a potential block to full extension and excessive tension and discomfort at the medial and lateral retinaculum. Hyperextension of the femoral component may lead to anterior notching and limited flexion [9]. Placing a femoral component too posteriorly may cause notching that can act as a stress riser of the femoral cortex, which can predispose for a supracondylar fracture. It also narrows the flexion space, which may lead to decreased flexion capability.
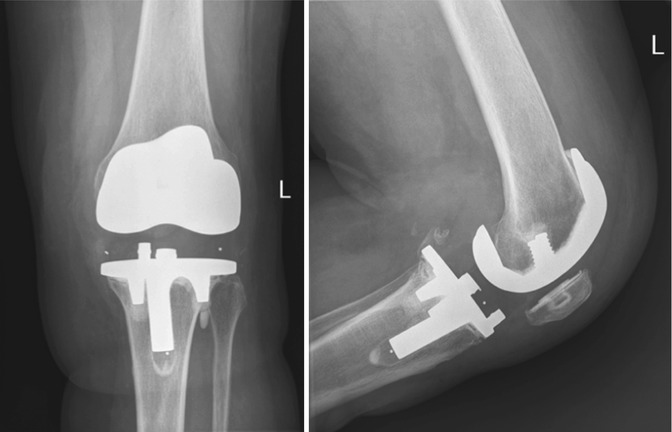
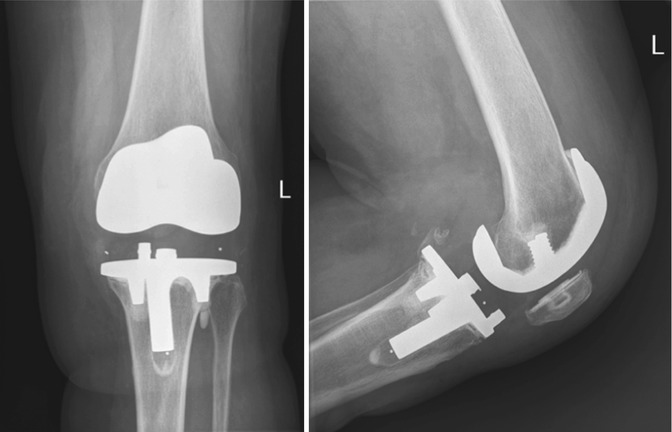
Fig. 21.3
Left total knee replacement (cruciate retaining) with patella baja due to proximalization of the joint line as a result of a thick polyethylene insert (probably following too much tibial resection). Other remarks include somewhat oversizing of the tibial plateau and the suggestion of femoral component oversizing. Clinically, there was pain and compromised flexion (85°). It was concluded that the flexion space was tight with a good patellar tracking but low patella. Subsequently, the PCL was released, immediately improving flexion to 110°, and a release (lateral and medial gutters) performed. Following this surgery, the patient was satisfied, flexion remained 110°, and there was no pain anymore
A tight PCL in cruciate-retaining TKR can cause a tight flexion space and subsequent stiffness. A loose PCL can cause excessive anterior translation of the femur resulting in impingement of the extensor mechanism (clinically: anterior knee pain) and posterior impingement of the femur on the tibia (clinically: possible popliteal fossa-oriented knee pain).
For the tibial component, an excessive sagittal posterior tibial slope increases the posterior space leading to a loose PCL in CR implants in flexion. Conversely, a limited or anterior slope tightens the flexion gap and creates PCL tightness in case of CR TKR, limiting flexion [36]. A high posterior lip on the polyethylene insert in posterior stabilized (PS) TKR may also limit deep flexion. In PS TKR, too much anterior slope – and especially reversed slope – can result also in limited flexion, while too much posterior slope can result in less extension. An example of abnormal tibial slope is given in Fig. 21.4.


Fig. 21.4
Lateral view of a left total knee replacement with too much posterior slope. As a result, the patient had a 25° extension deficit. Flexion was also impaired due to the patella baja
The position of the tibial component in the anteroposterior (AP) plane does not seem to be as important, although posterior overhang can limit flexion. Malrotation, however, is important, as will be discussed subsequently.
In CR TKR, an excessive sagittal tibial slope influences the PCL and, consequently, ROM. In PS TKR, excessive anterior slope can result also to limited flexion, while too much posterior slope can result in less extension.
Component oversizing and/or malpositioning (malalignment and malrotation), particularly internal rotation of the femoral and/or tibial component, has been related to stiffness, (anterior) knee pain, instability, and/or patellofemoral problems [18, 32, 37, 38]. Malalignment can also result in asymmetry of the extension gap that can lead to instability. Malrotation can result in asymmetry of the flexion gap or patellar tracking problems, which both can result in a paradoxically stiff TKR with impaired flexion [8].
Component oversizing and malposition of TKR are related to stiffness and anterior knee pain.
Clinically, the finding that should raise suspicion for malrotation is an external rotation of the patient’s unsupported foot at 90° flexion; this implies excessive tibial component internal rotation (Fig. 21.5). An increasing amount of recent literature advocates CT scanning [39, 40] in cases of a stiff and/or painful TKR to further analyse malrotation and/or malsizing (particularly oversizing) [32, 37]. Notably, internal rotation errors of the tibial component appear an underestimated cause of poor ROM, patellar complications, and anterior knee pain [37]. In our opinion, the presence of component malrotation (particularly tibial component malrotation) should not be solely based on CT analysis [39, 40] but on the combination of both the clinical picture (e.g. Fig. 21.5) and CT analysis.


Fig. 21.5
Clinical example of an internal rotation error of the tibial component resulting in a typical excessive external rotation of the foot and ankle; in this case of the left total knee replacement
Sizing of the components is important. Daluga et al. [18] found significantly higher percentage of manipulation under anaesthesia for stiffness if the femoral AP diameter increased ≥12 %. Carillon and Bonnin [32] also found a relationship between oversizing (femoral and tibial) and pain or stiffness. Kim et al. [25] found oversizing of the component(s) in 18 %. These findings are in line with the comment that downsizing the femoral component is “integral to improving ROM” [38]. Other femoral component factors limiting flexion are an extended or flexed position of the femoral component and possibly a decrease in posterior condylar offset [35, 41, 42] even though others argued this in both CR- and PS-type TKR [41, 43–45]. An example of oversizing is provided in Fig. 21.6.
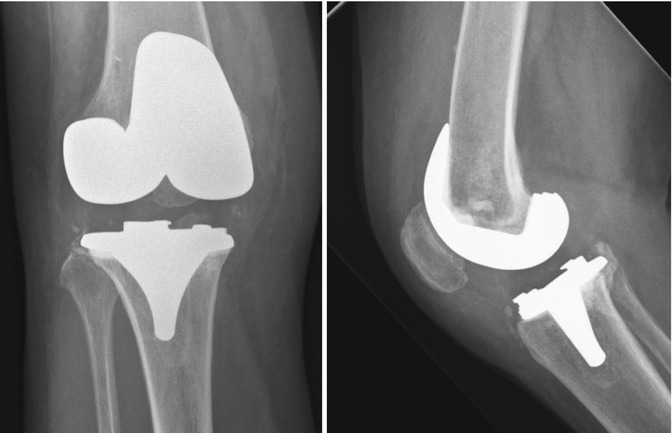
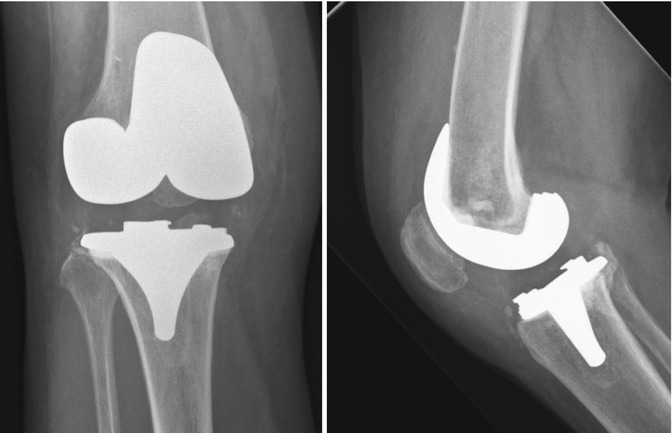
Fig. 21.6
Right total knee replacement with status after two-stage revision for possible infection; the cultures however did not reveal infection. Clinically, there was unchanged diffuse pain and impaired function (flexion 70°, extension 20° impaired). Work-up revealed aseptic tibial loosening, a consequence of not using a stemmed tibial component in revision surgery, given the posterior subsidence of the tibial plateau on serial X-rays and osteolysis around tibial peg and posterior tibial plateau on CT analysis (not shown here). The femoral component was oversized in both mediolateral and anteroposterior planes (on X-ray and CT analysis). Revision was performed, during which the preoperative analysis was confirmed, but there was also unexpected significant ligamentous instability. Therefore, a rotating hinged-type knee replacement was performed. At follow-up, the patient was satisfied, pain had largely gone away, flexion improved to 105°, and extension was only 5° impaired
Joint line height and patella height are intimately linked. Despite the fact that maintaining joint line height is rather straightforward in primary TKR, it is one of the important steps as it is essential for optimal ROM but also ligamentous balance and proper knee kinematics [46–48]. A significant joint line change influences patellar height. The joint line change can involve distalization (resulting in patella alta) or, more commonly, proximalization (resulting in patella baja; Figs. 21.3, 21.4, and 21.7). These changes in patella height – specifically patella baja – are linked to limited ROM up to stiffness and/or (early flexion) instability [46, 48–51]. Specifically, patella baja predisposes for a higher chance of anterior knee pain, limited flexion due to impingement of the patella on the polyethylene liner and/or component(s), and structural tendon damage [46, 51–53]. Many patients with a true patella baja, i.e. who have a shortened patellar ligament due to fibrosis [54, 55], frequently have a painful and stiff patellofemoral joint and a limited ROM.


Fig. 21.7
Lateral view of a right total knee replacement showing a severe patella baja. Patient complained about anterior knee pain and problematic flexion. Lower pole resection, patellar resurfacing (button), tibial tuberosity proximalization, PCL release, and gutter release were performed. Following surgery there was still pain but much better than before surgery and the flexion improved from 70° to 90°
Errors in bony resection may cause flexion–extension gap mismatch with reduction of the ROM. Insufficient posterior condyle resection (in anterior referencing) may cause excessive tension on the collateral ligaments and PCL (if preserved) in flexion, consequently limiting flexion. Excessive posterior condyle resection may lead to a loose knee in flexion, i.e. flexion instability, which can paradoxically give rise to a stiff TKR (difficult to diagnose/analyse). Posterior osteophytes often cause an extension contracture, and removal is always essential.
All these factors limit intraoperative range of motion and will even worsen in the postoperative period, as the patient cannot move properly. Remember, the ROM that is achieved during surgery will not improve after surgery by rehabilitation.
Strive for optimal ROM during surgery, as the ROM will not improve postoperatively with any rehabilitation.
21.4 Postoperative Factors
The possible factors that can cause or attribute to postoperative stiffness are shown in Table 21.3. Joint infection should always be ruled out first as a possible cause for a stiff, swollen and painful TKR. It can present with few symptoms (e.g. difficult and slow rehabilitation without systemic signs) and not necessarily pain and/or the typical clinical infectious hallmarks.
Table 21.3
Postoperative factors affecting ROM after TKR
Joint infection |
Hematoma |
Heterotopic ossifications |
Hip (flexion contracture, e.g. due to osteoarthritis), spine (lumbar kyphosis) |
CRPS-1 |
Various neurological and muscular disorders |
Inadequate postoperative rehabilitation (too little and/or too aggressive physical therapy, noncompliant patient, inadequate pain treatment) |
Some stiff knees can present with massive connective tissue proliferation causing firm – but not fluctuating – swelling of the knee, with decreased patellofemoral mobility and lowering of the patella (patella baja). Histology of this arthrofibrotic tissue shows disordered matrix proteins and increased expression of collagen type VI, comparable to that found in lung fibrosis and superficial fibromatosis [56]. This scarring occurs between the extensor mechanism and anterior femoral cortex with suprapatellar pouch obliteration, but often the medial and lateral gutters are also affected. As a result, the quadriceps muscle becomes adherent to the femur and subsequently shortens, severely limiting both flexion and extension. Clinically, decreased patellofemoral mobility is a typical finding [1]. Hematomas, wound healing problems, and/or prolonged postoperative immobilization can also initiate such a fibrous tissue response resulting in a stiff TKR, including a (true) patella baja.
CRPS-1 can clinically also present as an arthrofibrosis-type reaction in which the entire joint is chronically swollen and the capsule is greatly increased in thickness. It should be specifically considered in the work-up, just as joint infection, as it complicates any treatment of the stiff TKR. CRPS-1 seems to be rare after TKR (0.7–0.8 %) [57, 58]. Notably, a short-term prospective study estimated a much higher prevalence of CRPS-1 (21.0 % at 1 month and 12.7 % at 6 months) [59]. Diagnosing CRPS-1 remains difficult, as there is no specific clinical or imaging modality, but the hallmarks are pain (excessive and disproportional) and stiffness. It should be considered when patients describe diffuse disproportional pain (i.e. pain out of proportion to examination findings and the performed TKR, often of neuropathic character), with a delayed functional recovery (flexion is more often affected than extension), pain at rest, sensory disorders (skin hypersensitivity), and/or atypical skin discolorations with trophic changes (low local temperature, hyperhidrosis, increase in skin hair growth). Early diagnosis is imperative as this may increase the chance for successful treatment. Treatment is difficult, should be approached in a multidisciplinary fashion, and is preferably done by a specialist with experience in this field. Recovery is time consuming and prolonged. Gentle mobilizations and NSAID may be sufficient if diagnosed early (<6 weeks), while more intense therapy is necessary if diagnosed later (>6 weeks).
Heterotopic ossifications (HO), especially when large, can also lead to stiffness after TKR. Dalury et al. [60] found an incidence of 15 % after TKR; other authors report between 1 and 42 % [61–67]. Risk factors for developing HO include male gender and higher than normal weight [60], history of HO, hypertrophic osteoarthritis, ankylosing spondylitis, or diffuse idiopathic skeletal hyperostosis [66]. Wide surgical exposition or closed manipulation may also be risk factors. HO is more frequently found in the suprapatellar pouch and supracondylar region.
Extra-articular factors can sometimes cause stiffness after TKR as well. Hip (flexion contracture, osteoarthritis) or spine (lumbar kyphosis) disorders may lead to flexion contracture and should be treated before TKR. Spinal kyphosis deformity, contractures of the ipsilateral hip (e.g. due to osteoarthritis), or knee extension lag (fixed flexion contracture deformity) causes the patient to compensate by shifting their centre of gravity anteriorly, which is balanced by a flexion of the hip and knee. These factors complicate retaining any correction after revision TKR surgery as contracture often recurs in these situations.
Proper rehabilitation is an essential factor in achieving satisfactory ROM after TKR. In daily practice this means adequate pain control and a controlled early intensive physical therapy protocol directly following surgery. This is important as pain can lead to both quadriceps muscle and hamstring tendon guarding, which negatively influences postoperative ROM. This guarding usually subsides within 6–8 weeks with steadily improving ROM in the first 3 months [68]. Conversely, a too aggressive rehabilitation may lead to an excessive inflammatory reaction with persistent pain and joint contracture. This can lead to scarring and atrophy (with fatty degeneration) of the extensor apparatus, which in itself can cause limited ROM as well.
Continuous passive motion (CPM; Fig. 21.8) has been reported in the postoperative treatment following TKR, particularly in the early phase. A recent Cochrane review found that CPM does increase knee flexion even though this effect was too small to be clinically meaningful (mean difference 2–3°), but reduces the need for manipulation under anaesthesia (weak evidence) [69]. The authors concluded that the effect of CPM on knee ROM was too small to justify its use [69]. In our institution CPM is considered only in patients with a positive history for CRPS-1 or stiffness of previous TKR, compliance issues in early rehabilitation after TKR, or after manipulation under anaesthesia for a stiff TKR. The technique by which we perform MUA is detailed in the treatment section.
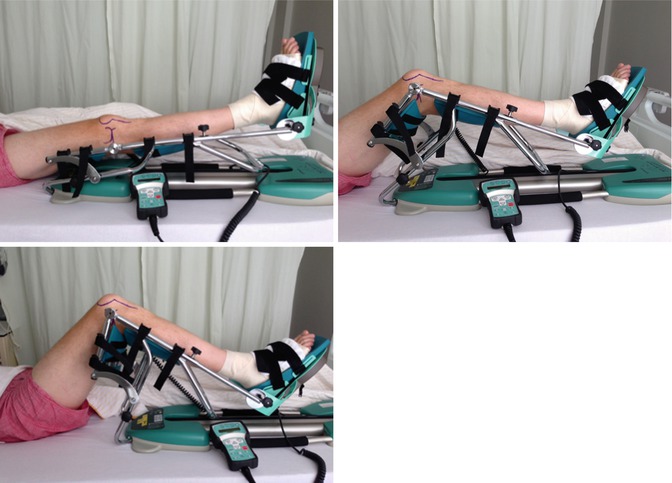
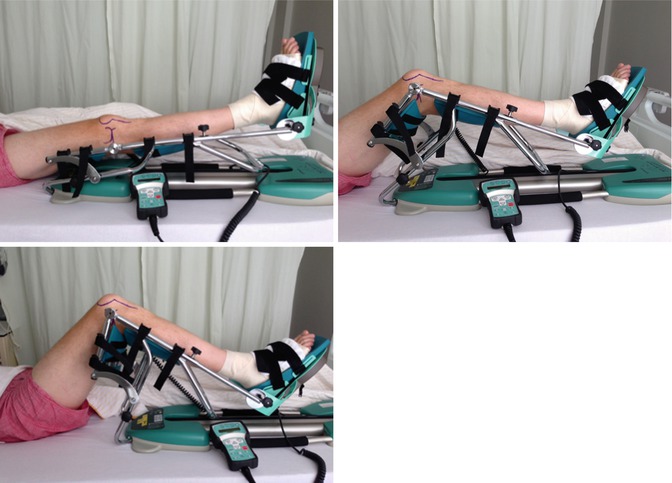
Fig. 21.8
Example of a continuous passive motion (CPM) apparatus. Note that, as shown, the pivoting point of the apparatus should be at the centre of the knee and the foot should be well fixed in the straps but comfortable
21.5 Diagnostics
In our opinion, the standard analysis of a patient with a stiff TKR should include a detailed history, physical examination, standing X-ray studies (including a full leg view), SPECT/(CT) scanning, and blood serology (C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)). We aspirate every TKR for analysis of the synovial joint (aerobic/anaerobic/general culture and leucocyte count with polymorphonuclear granulocyte percentage) if serology is abnormal (CRP and/or ESR) or when there is a higher probability for periprosthetic joint infection (based on history, physical examination, and X-ray analysis). This workflow is analogous to the diagnostic work-up (algorithm and criteria) as stated by the Proceedings of International Consensus on Periprosthetic Joint Infection [85]. We now follow this algorithm in the work-up of possible periprosthetic joint infection. Nuclear imaging (three-phase bone scan or SPECT/CT) can help to diagnose problems like loosening, malrotation, and/or malpositioning. Stress X-rays are performed in cases of suspected instability. Referral for analysis on possible CRPS-1 by a specialist in this field can be performed if suspected.
Standard analysis of a patient with a stiff TKR should include a detailed history, physical examination, standing X-ray studies (including a full leg view), CT scanning, and blood serology (CRP and ESR). On indication, joint aspiration, nuclear imaging, stress X-rays, and analysis by pain specialist for presence of CRPS-1 are performed.
21.6 Treatment
The treatment options for stiffness after TKR include physical therapy (PT), manipulation under anaesthesia (MUA), arthroscopic debridement/arthrolysis, open debridement/arthrolysis, or revision surgery of the TKR [6, 10–15]. Revision TKR will not likely help if there is no clear mechanical explanation for the stiffness. Moreover, the longer the knee has been stiff and the more previous surgeries have been performed, the less probable it is that the quadriceps muscle will regain elasticity and therefore allow ROM, regardless of what else has been improved in the revision procedure. In our institution, if pain is a major problem (particularly when diffuse and superficial), we frequently refer the patients to the pain specialist (anaesthesiologist in our institution) for pain treatment (e.g. capsaicin). This can have a good effect on the complaints and sometimes even better ROM due to better pain control.
The treatment of stiffness after TKR includes physical therapy, manipulation under anaesthesia, arthroscopic debridement/arthrolysis, open debridement/arthrolysis, or revision TKR.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








