Sprengel Deformity
CASE PRESENTATION
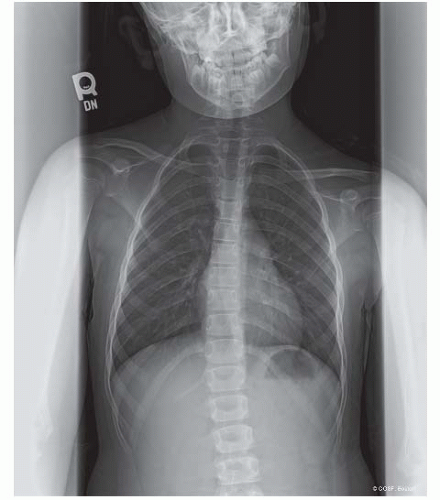
An 8-year-old child presents for evaluation of an asymmetric shoulder deformity. The family reports no antecedent trauma or associated anomalies. In addition to the shoulder deformity, they report that the child has had progressive difficulty with overhead activities, including swimming. Radiographs were obtained by the pediatrician and demonstrated a “birth defect” of the right shoulder blade (Figure 19-1).
CLINICAL QUESTIONS
What is Sprengel deformity?
What are the associated conditions?
How is Sprengel deformity classified?
What are the surgical indications?
What procedures may be performed for Sprengel’s?
What complications may occur from surgical reconstruction?
THE FUNDAMENTALS
Etiology and Epidemiology
When all is said and done, as a rule, more is said than done.
—Lou Holtz
While described by several surgeons prior to 1891, Sprengel is attributed with describing the congenital abnormality of the scapula that now bears his name.1,2 While Sprengel deformity is often referred to as congenital elevation of the scapula, in fact, it represents a failure of the normal descent or caudal migration of the scapula, which occurs during the 9th to 12th week of embryonic development. As the scapula typically migrates from a sagittal to coronal position, patients with Sprengel deformity will have the scapula protracted, with the inferomedial angle medial and the glenoid tilting inferiorly. In addition to the failure of descent, the affected scapula is often smaller, hypoplastic, and dysmorphic.
The etiology of Sprengel deformity remains unknown. Similarly, few definitive statements can be made regarding the epidemiology for Sprengel deformity, owing to its relative rarity and paucity of published information. In general, males and females are equally affected, and bilateral involvement may occur. While most cases are sporadic, an autosomal dominant inheritance pattern has been proposed.3 A number of associated conditions have been described, most notably Klippel-Feil syndrome (congenital cervical spine fusions), congenital scoliosis, and shoulder girdle deficiencies.
Clinical Evaluation
While the scapula is undescended at birth, often the aesthetic differences are subtle. With continued growth, the deformity becomes more apparent, and thus the diagnosis is often delayed in children without more extensive spinal and shoulder girdle congenital differences.
Patients will present with aesthetic differences in scapular position and shoulder height, of varying severity. Shoulder abduction and scapulothoracic motion are limited, often resulting in functional limitations with overhead and away from body activities. Inspection will reveal a small, high-riding scapula, often with malrotation and inferior tilt. Careful palpation will allow for identification of an omovertebral bone, an abnormal bony, cartilaginous, or fibrous connection between the cervical spine and the superomedial scapula thought to be present in approximately one-third of patients. Children with associated Klippel-Feil syndrome or congenital rib anomalies may present with torticollis, scoliosis, thoracic insufficiency, and other manifestations of their spinal/thoracic condition.
A number of classification systems have been proposed to characterize the severity of deformity. Traditionally, the Cavendish classification has been used to characterize the clinical deformity with the patient clothed4 (Table 19.1). Grade 1 deformities present without any visible deformity. Grade 2 deformity results in a mild prominence of the superomedial angle of the scapula. Grade 3 deformity signifies shoulder asymmetry of 2 to 5 cm. Grade 4 deformity results in >5 cm of shoulder height asymmetry.
Rigault et al.5 proposed a radiographic classification based on the position of the superomedial angle of the scapula (Table 19.2).
Rigault et al.5 proposed a radiographic classification based on the position of the superomedial angle of the scapula (Table 19.2).
Surgical Indications
I don’t believe the old statement, “If it ain’t broke, don’t fix it.” If that were the case, then Cadillacs and Jaguars and Mercedes would never make a change. I’ve always looked for ways to make things better.
—Vic Bubas
While the surgical indications for Sprengel deformity continue to evolve, in general, surgical reconstruction may be considered for patients at 3 to 4 years of age with severe deformity and functional limitations. While some authors have proposed surgical treatment based upon Cavendish or Rigault classification, every patient is different, and it is difficult to correlate aesthetic differences and shoulder impairment with clinical or radiographic appearance.6, 7, 8 and 9 Surgical treatment is not recommended for mild aesthetic differences in the absence of pain or functional limitations.
Table 19.1 Cavendish classification of Sprengel deformity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
A fundamental tenet of pediatric orthopaedic surgery is that surgical treatment should only be recommended when the natural history can be favorably altered. Unfortunately, the natural history of Sprengel deformity is not well characterized. The best insight into the natural history of this condition comes from Farsetti et al.,6 who reported on 14 patients with Cavendish grade 1 to 3 Sprengel deformity observed until the ages of 18 to 67 years. One-half had mild-to-moderate pain with activity, and shoulder abduction was restricted in all. While there were no improvements in deformity over time, there were no cases of progressive deformity. When compared with a similar cohort of patients who underwent operative reconstruction, surgical patients had improved shoulder abduction of about 40 degrees, improved aesthetics, and no cases of recurrent deformity.
While a host of procedures have been proposed, most reconstructive strategies are variations of either the Woodward or Green procedures.10,11 The Woodward procedure is preferred by most due to its relative technical ease and potential biomechanical advantage of displacing the muscle origins inferiorly, thereby rotating and lowering the scapula.12,15
SURGICAL PROCEDURES
▪ Resection of Superomedial Angle of Scapula
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree