Fig. 14.1
Rugby player sustaining a groin injury during play
Background
The controversy surrounding the diagnosis and management of groin pain results from the inability to offer an exact pathological diagnosis as many of the conditions which cause groin pain are simply grouped together and are labelled as groin disruption or sportsman’s groin. The groin itself is a very non-specific area lying “somewhere” between the abdomen and thigh so it is no surprise that the terminology itself creates confusion as the word “groin” is too vague and covers many structures. A tear in the rectus sheath attachment is different from an adductor tendon tear or an inguinal ligament strain and yet all are labelled as sportsman’s groin, athletic pubalgia or one of the many eponyms which have evolved to describe this enigmatic condition. Since all the muscular and tendinous attachments to the pubic bone can potentially become disrupted or inflamed, clinicians and sports therapists must consider which particular structure(s) is causing the painful symptom and offer an anatomical and pathological diagnosis.
Differentiating between pain caused by adductor tendon enthesopathy, inguinal ligament enthesopathy, conjoined tendon disruption and rectus sheath pathology is essential as the treatment of these separate conditions is inherently different. The umbrella term of “groin pain” is wrong and misleading for clinicians who should offer a specific treatment for a specific condition. Patients with abdominal pain, for example, seeking advice from a specialist general surgeon expect a more specific diagnosis than that of “abdominal pain”. Similarly, specialists treating patients with groin pain should be able to offer a more anatomical or pathological diagnosis. The term sportsman’s hernia should also be abandoned. If a hernia is present in an athlete the diagnosis of hernia should be used. Sportsmen and women do not develop their own type of hernia. Most sportsmen and women with “groin pain” have a strain or a disruption to one or more of their ligaments, muscles or tendons.
Conventional Concepts
The concept of pain in the upper groin or in the area around the inguinal canal or pubic tubercle was first popularised by Gilmore in 1980—commonly referred to as Gilmore’s groin [3]. Gilmore believes there is a musculo-tendinous injury or muscular disruption of the structures surrounding the inguinal canal and patients improve with surgical repair. He emphasises that the majority of patients have a torn external oblique, a torn conjoined tendon and a dehiscence between the conjoined tendon and inguinal ligament [4]. He also comments that 40 % of sportsmen may have an adductor tear and some have a torn rectus sheath or muscle, but the hypothesis remains that the cause of pain around the pubic tubercle is disruption to structures around the inguinal canal. Despite very acceptable surgical results there has been no documented photographic or reproducible pathological evidence for his findings. Patients undergo an open surgical repair with suture reinforcement of the various layers. This has been an accepted form of treatment for sportsman’s groin for decades and many other surgeons have adopted this philosophy and offer a variety of open surgical repair for the treatment of groin pain [5].
The groin itself is a very non-specific area lying “somewhere” between the abdomen and thigh so it is no surprise that the terminology itself creates confusion as the word “groin” is too vague and covers many structures.
In contrast, Meyers believes there is a mechanical strain around the pubic bone and refers to the complex anatomical confluence of all its ligamentous and tendinous attachments as forming a “pubic joint” over the pubic bone [6]. He believes that there is a hyper-extension injury involving the abdominal wall and muscles of the thigh causing tears in some or many of the structures involved. He proposes that the pubic bone acts as a fulcrum and extreme bio-mechanical forces are instrumental in causing the injury around the so-called pubic joint. If surgery is required then the whole anterior “joint” has to be repaired with detachment and re-attachment of the lateral part of the rectus sheath/muscle insertion together with a tenotomy of the adductor longus insertion. Rehabilitation can take 3 months but very good results can be achieved [7]. He specifies that his patients now undergo preoperative MRI scanning and that any release or repair procedure is tailored to both the clinical and radiological findings [8].
A third hypothesis, perhaps representing a minor variant of Gilmore’s groin, proposed by Muschaweck, is that in elite athletes with groin pain there is a small hernia defect in the posterior inguinal wall within the transversalis fascia [9]. This is associated with a small medial shift of the rectus muscle/sheath attachment onto the pubic bone. Muschaweck also believes that the groin pain caused by this posterior inguinal wall weakness is exacerbated by entrapment of the genital branch of the genito-femoral nerve. She has introduced the “minimal-repair” technique in which athletes undergo open surgery under local anaesthetic where the transversalis fascial weakness is identified, split and repaired in two layers using a small polyprolene running suture. The free lip is sutured to the inguinal ligament. An additional suture is placed in the lower rectus muscle to “lateralise” it [10]. This is placed to counteract the increased tension produced by the rectus muscle on the pubic bone. In 50 % of her patients she divides the genital branch nerve. The results are again very satisfactory with most athletes returning to sport within weeks. The contribution of the nerve to the severity of symptoms has yet to be defined but in all cases fibrosis surrounding the genital nerve branch has been identified. It is unclear why only half of her patients require division of this nerve since her reported results seem not to depend upon this particular neurectomy. It is also unclear whether the additional suture into the rectus sheath does in fact “realign” the muscle and rectus sheath.
A New Concept: Inguinal Ligament Pain
Some athletes present with pain around the pubic tubercle at the medial attachment of the inguinal ligament as seen in this photograph (Fig. 14.2). Although the development of this pain may be insidious, on occasions there can be an isolated injury which precipitates the onset of the pain. The pain is usually caused by kicking, twisting and even by simple movements such as sneezing, coughing or getting out of bed or a car. The repetitive movement can also be specific to a particular sport. The degree of pain varies but the patient often points to an area near the pubic tubercle (Fig. 14.3). The pain can radiate into the abdomen, the adductor region and pubic bone. Radiographic studies are useful to exclude other pathology such as labral tears and ilio-psoas bursitis but rarely are positive findings at the pubic tubercle demonstrated. Occasionally bone oedema of the pubic bone on the affected side is seen on MRI. However, interpretation of the MRI images has to be done with caution as some abnormalities do not correlate with clinical findings. In fact, more abnormalities have been found in the contra-lateral asymptomatic side in some athletes [11].


Fig. 14.2
Photograph of a patient pointing to the site of pain at the inguinal ligament attachment
Fig. 14.3
Schematic diagram of the inguinal ligament and surrounding structures
Clinical examination is paramount as the site of pain needs to be determined accurately. The groin must be palpated with the leg abducted and the knee flexed. Palpation proceeds systematically around the structures relating to the pubic tubercle—the so-called pubic clock [12]. This includes examination of the adductor tendon, pectineus, lacunar ligament, inguinal ligament, conjoined tendon and rectus sheath attachment. More specifically, the adductor tendon is palpated first by assessing whether there is any true tenderness associated with its attachment on to the pubic bone. The tenderness may be enhanced by adduction of the leg against resistance. Many patients with upper groin pain are referred with an incorrect diagnosis of adductor tendinopathy so this initial examination is extremely important. Clearly, if the patient is tender at this point then a diagnosis of adductor enthesopathy could be made. Medial to the adductor longus insertion is pectineus which inserts along the pectin line of the superior pubic ramus. Since the pectineal fascia overlying the pectineus attaches to the pectineal ligament, deep palpation onto the pubic tubercle via the femoral canal has to be done and may elicit the exact symptoms described by the patient. The pectineal ligament joins the lacunar ligament which in turn attaches to the inferior part of the inguinal ligament. Again deep palpation against the pubic tubercle may reproduce the symptoms described by the athlete and indicate inguinal ligament enthesopathy. This, of course, can be very subjective so any interpretation should be taken cautiously and compared with palpation of the contra-lateral side and the examination repeated several times. Careful palpation of all the structures is required to formulate an exact clinical and anatomical diagnosis. Examination continues over the inguinal ligament at its attachment to the pubic bone. Occasionally, athletes present with vague pain around the pubic tubercle and deep palpation of the inferior part of the inguinal ligament attachment may elicit symptoms. This is done by palpating the pubic tubercle through the posterior inguinal canal. The tenderness may extend along the inguinal ligament. It is rare that palpation produces pain more medially over the rectus sheath attachment but this must also be examined. The conjoined tendon inserts between the inguinal ligament and rectus sheath and is difficult to define exactly on clinical examination. If athletes have pain elicited at the junction of the rectus sheath and pubic bone then a rectus sheath tear or osteitis pubis should be suspected and an MRI scan organised. Osteitis pubis produces pain in the midline, anterior and superior to the pubic symphysis with some pain radiating to the perineum. True osteitis pubis produces classic changes on MRI scanning and each patient will of course have to be treated on an individual basis. The inguinal orifices must be examined in the supine and the upright position as clinical assessment for inguinal and femoral hernias is mandatory in any athlete with groin pain. The presence of a bulge or cough impulse may or may not be contributing to the athlete’s symptoms. Since small cough impulses are common in young men they are usually asymptomatic and it should not be assumed to be the cause of the painful symptoms. After a thorough clinical examination, if the patient’s symptoms can be reproduced by palpation around the pubic tubercle, inguinal ligament pathology should be considered.
Inguinal Ligament Pathology
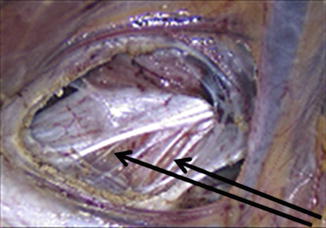
The new concept proposes that there is tension in the inguinal ligament attachment and that in severe cases releasing the tension at the pubic bone attachment results in significant clinical improvement in the patient’s symptoms [13]. The pathology may be analogous to tennis elbow where there is degeneration of the attachment of the extensor tendons on to the lateral epicondyle of the humerus. The analogy may be extended further as the inguinal ligament may actually be a tendon as it is not a typical ligament which crosses a joint. It actually represents the lower fibres of the external oblique muscle and therefore should be defined as a tendon (Driscoll P, Edinburgh, personal communication). At laparoscopy, exposure of the inguinal ligament can be achieved by reflecting the peritoneum and dividing the transversalis fascia medially near the pubic bone. The spermatic cord is retracted upwards allowing full exposure of the ligament. In healthy individuals the ligament is attached uniformly onto the pubic tubercle and the lower fibres are seen to merge with the lacunar ligament with a healthy intact free edge at the medial wall of the femoral canal. In many athletes with groin pain there are abnormalities of the inguinal and lacunar ligaments. The ligaments can appear inflamed and oedematous and even disrupted. The most common finding is that there is attenuation of the ligament at the attachment with tears affecting the inferior half of the ligament. If the tension is uneven and only transmitted through part of the inguinal ligament, this results in an inguinal ligament enthesopathy and pain at the site of the pubic tubercle. Figure 14.4 is a photograph taken at laparoscopy in an elite athlete with groin pain. It demonstrates macroscopic disruption of the inguinal ligament attachment.