Chapter 44 Sports Medicine
Role of the Team Physician
The team physician has multiple, overlapping roles within the framework of the team itself, the individual athletes and their families, the school or overseeing organization, and the community. The primary responsibility is caring for the health and well-being of the individual athlete. The chief duties are to determine initial medical eligibility, provide care for the injured athlete, facilitate and determine return to play, create and maintain emergency preparedness, oversee the healthfulness of the team’s overall training program, supervise the personnel providing health care for the team, and protect against institutional and personal liability.124 The role of intermediary for each of these groups is both a challenging and rewarding one. The team physician is responsible for conveying information to other medical specialists, allied health professionals, athletic trainers, and coaches, as well as for creating and coordinating health care plans for the athletes.3
Beyond the medical obligation to the athlete, there is an assumed medicolegal responsibility of a team physician. Physicians receiving financial or other obvious remuneration for services are bound by normal medicolegal responsibilities. The physician might be held legally liable if injury occurs as a result of negligence or treatment below the professional standard of care. Those physicians who volunteer their services are typically covered by Good Samaritan laws, although these are not present in every state and vary from state to state. These laws often state that the services provided must meet the accepted standard of care to be protected.41 Professional organizations, universities, high schools, and individual physicians also have all been held liable for inadequate emergency preparedness.124 Preparticipation evaluations (PPEs) are not covered under Good Samaritan laws. In some cases, athletes might be legally allowed to participate despite a disqualifying PPE.
The team physician is also responsible for the final decision regarding clearance to play or return to play (RTP) after injury. These issues can be complex, and several fundamentals must be met before the athlete should be cleared. When recovering from an injury, the athlete must have completed appropriate rehabilitation; a health care professional must document the athlete’s recovery; and the risks of return must be discussed and documented. The team physician must obtain the appropriate consultant opinions when dealing with conditions or injuries outside the scope of his or her practice. Although some states have determined that athletic participation implies assumed risk, this is not universal. Team physicians have been held liable for injury occurring after full RTP has been granted. In cases of differing opinion of the team physician and a consultant, the final responsibility typically lies with the team physician.
Event Administration
Both require significant preseason or pre-event planning.72 From an administrative perspective, it is essential that the team physician or chief medical officer develops a chain of command that defines the responsibilities of the medical providers, emergency medical services, event officials, and other parties involved in the athletic event and athlete care. Establishing and regularly rehearsing an emergency action plan (EAP) is critical. Reviewing the medical equipment that will be available at the event as well as the protocols for attending to an injured athlete are standard components of preparation. The team physician must also assess environmental concerns and playing conditions and have a policy to modify or suspend practice or competition if adverse conditions exist.
Although any marathon has a known number of people requiring medical assistance (2% to 20% of participants depending on event size, duration, and weather conditions), if these numbers should increase unexpectedly, there is a potential for the community resources to become overwhelmed if not allocated appropriately.30,133 For this reason, communication among the medical team, race officials, emergency medical services, local hospitals, and participants is critical to help prevent and respond to incidents during the race. It is the role of the chief medical officer of the event to coordinate these effective lines of communication.
Principles of Conditioning and Training
Effective training programs require a fundamental understanding of strength, flexibility, and endurance development, as well as the basic principles of specificity, individuality, periodization, overload, and tapering. Please refer to Chapter 18 on Therapeutic Exercise for an overview of strength, flexibility, and endurance training.
The principle of overload requires that the training stimulus be greater than what the athlete normally performs in competition. Exercise frequency, duration, and intensity are manipulated to produce overload. These specific training variables (frequency, duration, and intensity) must be periodically increased for an athlete to progress (Box 44-1).
BOX 44-1 Training Program Design Variables: FITT
From Frontera WR, et al: Clinical sports medicine: medical management and rehabilitation, Philadelphia, 2007, Saunders.
Periodization
Periodization is one structured training approach that highlights this concept. It was developed by a Russian physiologist in the 1960s but has had a significant resurgence in today’s training programs (Figure 44-1). In periodization, training is divided into defined “periods” to allow buildup of training stresses, time for rest and adaptation to training, and continual progression of fitness. These periods include macrocycles (commonly lasting 1 year), which are divided into shorter mesocycles (commonly lasting 1 month), which are then subdivided into microcycles (commonly lasting 1 week). Microcycles are generally the weekly training programs. Each mesocycle can be made up of four weekly microcycles with a gradual buildup of training frequency and intensity over the first 3 weeks and then a slight decrease in the fourth week to allow for rest and the subsequent metabolic training adaptations to occur. The athlete is then ready to enter the next 4-week mesocycle and progress through another four weekly microcycles. The amount and intensity of training occurring in each mesocycle depend on where the athlete is in relationship to the competitive season, which is how macrocycles are structured.
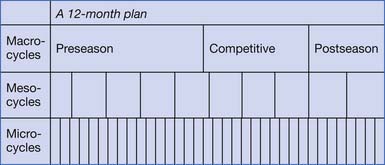
FIGURE 44-1 A template for a periodized training program.
(From Bachl N, Baron R, Smekal G: Principles of exercise physiology and conditioning. In Frontera WR, et al, Clinical sports medicine: medical management and rehabilitation, Philadelphia, 2007, Saunders.)
A typical year-long training program will have three macrocycles: preseason or “build-up phase,” competitive season or “maintenance and fine-tuning phase,” and finally a postseason or “recovery phase.” The preseason macrocycle is typically the longest, occurring before the competitive season. It is designed to develop fitness in anticipation of the more intense training to follow.162 During the preseason macrocycle the athlete generally focuses on higher volume and lower intensity exercise.
The competitive season macrocycle follows the preseason period. The focus of this cycle is to develop and maintain peak fitness with a focus on high-intensity training and sport-specific technique drills.162 Because of the higher intensity training, the volume must be significantly reduced.
Finally, the postseason macrocycle is a time for the athlete to recover from the previous year’s training and physically and mentally prepare for the next year of training and competition.162 The early portion of this period necessitates “active rest.” The athlete generally participates in unstructured, non–sport-specific recreational activities to allow for recovery from the stresses of the competitive season. This is an important period for the athlete to adequately recover from injuries, prevent overtraining, and take a “mental break” from the competitive season.
During the competitive season, a typical microcycle includes a tapering period just before competition. The taper is a short period of reduced training before an important competition with the goal of optimizing performance. Although it is well recognized that a reduction in training before competition improves performance, it not definitively known what is the most ideal taper strategy regarding altering training volume, intensity, and frequency.8,77,113 A recent metaanalysis demonstrated that the most efficient strategy to maximize performance gains appears to be a 2-week taper during which training volume is exponentially reduced by 41% to 60%.19 This study found that the ideal taper for endurance athletes kept training intensity and frequency stable, with only volume being progressively reduced.
Overtraining Syndrome
An important set of symptoms to be aware of for any athlete, coach, or sports medicine physician is that related to overtraining syndrome. When prolonged, excessive training occurs concurrently with insufficient recovery, the athlete might have unexplainable performance decrements resulting in chronic maladaptations leading to overtraining syndrome.109 Common symptoms of overtraining syndrome in addition to an unexplained performance decrement include generalized fatigue, mood disturbance, poor sleep, and increased rates of illness and injury. By definition, these symptoms persist despite more than 2 weeks of rest.158 The treatment is rest, from weeks to months, with gradual resumption of training. Prevention, however, is the best treatment, and following a periodized training program is one method to ensure adequate rest from more intense bouts of training.
Altitude Training
Altitude/hypoxic training is a controversial area of research and sports performance. Many elite endurance athletes incorporate altitude training into their typical training program in hope of enhancing performance in competition. For those athletes who do not live in mountainous areas, there are a variety of “altitude tents” on the market that can be used to simulate living at high altitude. Some controversy arose in 2006 when the World Anti-Doping Agency (WADA) considered placing “artificially-induced hypoxic conditions” on the Prohibited List of Substances/Methods.166 Another area of controversy is the uncertain primary physiologic mechanism(s) responsible for the effect of altitude training on sea-level performance. The proposed mechanisms include accelerated erythropoiesis (increased erythrocyte volume) as the primary hematologic effect, as well as nonhematologic factors such as improved muscle efficiency at the mitochondrial level, glucose transport alterations, and enhanced muscle-buffering capacity via pH regulation.60
Most scientists agree that the most effective form of altitude/hypoxic training is the “live high–train low” method, whereby athletes “live high” to stimulate erythropoietin and subsequently increase erythrocyte volume and “train low” to train at a higher intensity with improved oxygen flux to induce beneficial metabolic and neuromuscular training adaptations.167 The controversy here comes from not knowing what the optimal “dose” of altitude training truly is. So far the research suggests that for athletes to derive the most beneficial hematologic effects while using natural altitude, they need to live at an elevation of 2000 to 2500 meters for 22 hr/day for 4 weeks. For those using simulated altitude environments, 12 to 16 hours of hypoxic exposure might be necessary but at a higher elevation (2500 to 3000 meters167).
Injury Prevention and Rehabilitation
Kinetic Chain Assessment
The kinetic chain model is based on the idea that each complex, athletic movement is the summation of its constituent parts. For example, a quarterback’s throwing motion is created through the action of feet on the playing surface, loading of the lower limbs, rotation of the hips and abdominal muscles, activation of the latissimus dorsi, stabilization of the glenohumeral joint by the periscapular muscles, loading of the throwing arm through the deltoid and biceps, and finally from the upper limb motion of elbow extension and wrist flexion. The upper limb acts as a “funnel” for the energy generated by the core and lower limbs.85 Each of the “links” in the chain must function well to optimize performance and minimize potential tissue trauma.
“Catch-up” occurs when an athlete tries to compensate with one segment for a deficiency in a separate segment. This phenomenon puts higher stress on the tissues of the distal segment and predisposes it to injury.85 For example, a runner mighty present with patellofemoral pain for a variety of these reasons. This could simply be an overtraining phenomenon, or it might be due to weak or inhibited hip musculature, abnormal foot and ankle biomechanics, or poor running technique.105 Relief can be achieved through resting the athlete temporarily, but the pain might consistently return unless the causative issue is corrected. The experienced sports medicine physician will identify the tissue diagnosis and treat it appropriately, but will also identify and correct all predisposing factors. It is important that the physician is able to explain these concepts to the athlete and the treatment team to achieve optimal results.
Rather than view all similar overuse injuries as the same issue, the sports medicine physiatrist is able to break down the complex motions of the athlete into the constituent parts, identify the maladaptive pattern, and create a rehabilitation program that will prevent the injury from recurring. When examining the injured athlete, it is vital to make a biomechanical diagnosis rather than to focus exclusively on the injured tissue. Although it is easy to focus exclusively on the painful tissue, it is essential to assess the entire athlete and his or her mechanics to make appropriate tissue and biomechanical diagnoses (Table 44-1).
Table 44-1 Tissue Diagnosis and Biomechanical Diagnosis
| Tissue Diagnosis | Potential Biomechanical Diagnosis |
|---|---|
| Lateral/medial epicondylitis | Posterior deltoid weakness |
| Hamstring strain | Overly tight hamstring, weak gluteal musculature |
| Metatarsal stress fracture | Supinated foot |
| Athletic pubalgia | Weak core musculature, tight hip girdle |
| Shoulder impingement with rotator cuff strain | Periscapular weakness or inhibition |
| Patellofemoral syndrome—patellar cartilage irritation or chondromalacia | Quadriceps and gluteal weakness or inhibition, overpronation |
| Repetitive ankle sprains—anteriotalofibular ligament FL laxity | Weak peroneals, proprioceptive dysfunction |
The physical examination of the athlete must be focused on finding the biomechanical culprit, rather than focusing solely on the painful tissue. The athlete must be examined in detail to fully assess the possible causes of the injury. Select upper limb tests that help determine the role of the scapula in upper limb injuries include the scapular assistance test and the scapular retraction test.87 Core muscle function must be assessed dynamically and addressed as part of the rehabilitation plan.88 Examples of physical examination maneuvers to evaluate core muscular function in the athlete are demonstrated in Figures 44-2 to 44-5. The kinetic chain assessment is designed to assess flexibility, strength, and functionality of the affected limb. The examination essentially assesses multiplane sports-specific dynamics rather than single-plane, solitary joint movements.
It is vital for the examining physician to have a thorough understanding of the motions involved in the athlete’s sport to make the appropriate changes; for example, a difference of 10 degrees in knee extension during the cocking phase of a tennis serve increases the valgus load at the elbow by 21%.50 When necessary, this can be accomplished through discussion with the athlete, parent, coach, and/or trainer.
Prehabilitation
Prehabilitation is based on the concept that many sports injuries can be prevented if the athlete engages in an appropriate preseason “prehabilitation” program. Most of the scientific literature regarding prehabilitation programs focuses on noncontact anterior cruciate ligament tears.73,74,97 Poor form is also linked to numerous athletic injuries. Balance perturbation, plyometric training, and stretching programs all have a role in the prehabilitation of the athlete. Ideally, some of these issues can be assessed during the preseason physical examination and corrected before the start of the season. A large proportion of sports injuries are related to overuse, and it is wise to have a discussion of these issues with athletes and coaches in the preseason. Off-season cross-training, core muscle work, and cardiovascular preparation are generally considered key to a healthy season.
Injury Phases
Rehabilitation is guided by the status of the injured tissue, so an understanding of the timing of injury and recovery is essential. Injuries can be acute, subacute, chronic, or an exacerbation of a chronic condition. A detailed history is required because athletes will present at varying points of their tissue healing, and the treatment plan will have to be created appropriately. Four general phases are typically seen in tissue injury and repair. The physician caters the treatment to the individual tissue and the timing of the injury. The first phase involves the initial injury and the subsequent inflammation, edema, and pain. This phase is typically short, lasting days, depending on the severity of the injury. The reparative phase of the injured tissue might last from 6 to 8 weeks. It involves cell proliferation, granulation tissue formation, and neovascularization. The last phase is remodeling, which occurs as the tissue matures and realigns.
Stages of Rehabilitation
Rehabilitation can be viewed as a three-stage spectrum from the acute stage to the recovery stage, and then to the final functional stage through return to full play (Table 44-2).86 Each stage has individual goals that lead to the overall goal of RTP. The acute stage of rehabilitation is focused on managing the symptoms and signs of the injury. The classic PRICE (protection, rest, ice, compression, and elevation) approach is often followed. Medications, manual therapy, and physical modalities are also used during this phase. If necessary, bracing, injection, or surgery is performed to facilitate protection and future healing. ROM, strength, and cardiovascular fitness must be maintained as much as is possible and tolerated. This can be accomplished by exercising the upper body of an athlete with a lower body injury. Passive ROM must be viewed with caution in the acute to subacute injury phase because it might injure the tissue, leading to increased pain and inflammation. Isometric strength exercises can be prescribed during this stage, if tolerated, to decrease pain, edema, and potential atrophy. The athlete can advance to the next stage of rehabilitation if adequate pain control and near-normal ROM is achieved.
Table 44-2 Typical Return-to-Play Phases
| Phase | Goal | Timing |
|---|---|---|
| Phase 1 (acute) | Allow injured tissue time to heal; decrease symptoms, maintain range of motion | <72 hr |
| Phase 2 (recovery) | Increasing demands on the athlete; flexibility, strength, endurance training; kinetic chain corrections; maintain cardiovascular fitness through cross-training | Variable |
| Phase 3 (functional) | Advance toward full return to play, advance cardiovascular fitness | 2-4 wk |
In the case of an athlete with a shoulder injury, the rehabilitation program moves from predominantly closed-chain exercises, to axial-loaded exercises, to open kinetic chain exercises, to full sport-specific rehabilitation.108 Kinetic chain rehabilitation is modified to the individual athlete’s symptoms and dysfunction. Rather than view this type of rehabilitation as a series of discrete steps, the physiatrist should consider it as a transition from dysfunction to function and adjust the treatment plan and timing accordingly.108
The parameters of the strength training program (repetitions, resistance, speed, multijoint movements) can be adapted during this time, depending on the clinical scenario. Preexisting kinetic chain issues or tissue overload issues from the current injury are addressed at this time as well. As the rehabilitation program continues, increasingly athletic maneuvers (running, jumping, cutting) are used. Neuromuscular control (NMC) involves proprioception, muscle control, and the interplay between the two. Without sufficient NMC, the athlete might continue to be predisposed to future injury. This recovery phase is the most variable and has the highest potential for reinjury, as the tissue is actively remodeling. The athlete must be reevaluated frequently during this phase because setbacks are common and can require modification of the rehabilitation plan. The athlete can advance to the final stage once pain-free ROM is achieved and strength is 75% to 80% or greater (compared with the noninjured side).
During the final functional stage of rehabilitation, the focus remains on kinetic chain issues and technique errors. Strength balance, power, endurance, functional ROM, and NMC are aggressively addressed. Sport-specific drills are used during this stage and advanced to include practice. Full RTP is achieved when the injury is no longer painful; when there is normal flexibility, strength, and proprioception; and when appropriate sport-specific mechanics and sport-specific skills are achieved and reproducible. In many cases, this rehabilitation phase becomes the maintenance program.56
Biomechanics of Sports
Throwing
Approximately 50% of the velocity of a pitch results from the step and body rotation (from the potential energy stored in the large leg and trunk musculature).154 The other 50% comes from the smaller muscles of the shoulder, elbow, wrist, and hand. When forward stride is not allowed, the peak velocity of a pitched ball decreases to 84%. When the lower body is restricted, it decreases to 64%. Peak velocities in water polo are approximately 50% that of baseball because of the lack of a ground reaction force.
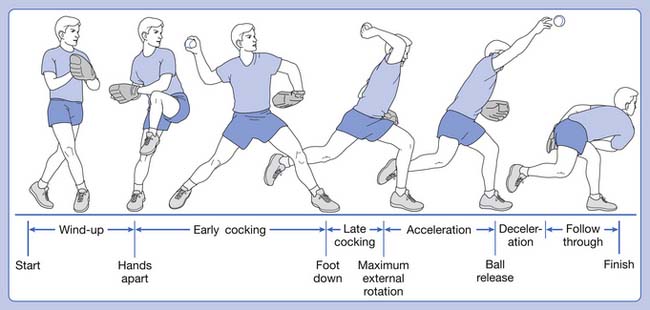
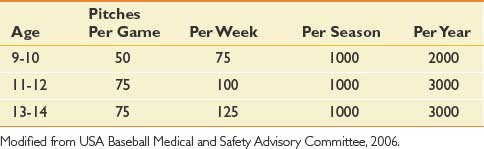
The baseball pitch is composed of six phases (Figure 44-6). Understanding these phases is critical to understanding, diagnosing, preventing, and treating throwing sports’ injuries.
Early cocking is next and is often called the stride phase.110 The stride leg extends toward the batter, as does the knee and hip of the pivot leg, propelling the body forward into the stride. As the hips rotate forward, the trunk follows and subsequently, the throwing shoulder abducts, extends, and externally rotates, leaving the shoulder in a “semicocked” position. Again, in this early phase, there is less risk of injury because most forces are still being generated in the trunk and lower limbs; however, shoulder activity does become more evident. The trapezius and serratus anterior demonstrate moderate to high activity to protract and upwardly rotate the scapula. The middle deltoid generates the abduction force, and the supraspinatus fine-tunes humeral head positioning within the glenoid.
The next phase is late cocking. The hallmark of this phase is when maximal shoulder external rotation is obtained. The shoulder begins this phase in approximately 50 degrees of external rotation and ends in about 175 degrees at maximal external rotation. This extreme amount of rotation allows the greatest accelerating force to the ball over the greatest possible distance. The amount of external rotation obtained correlates with the speed of the pitched ball. A majority of injuries occur in the late cocking and deceleration phases of throwing (Box 44-2).121 For late cocking, this is due to the forces needed to stabilize the shoulder in this extreme ROM. The dynamic stabilizers of the anterior shoulder (long head of the biceps, subscapularis, and pectoralis major) are very active in this phase. The static stabilizers (glenohumeral ligaments, capsule, and labrum) are active as well. The glenohumeral ligaments and capsule increase in laxity because of the extreme ROM in the overhead athlete. This laxity is necessary for performance; however, overstretching these ligaments enhances the work of the dynamic stabilizers with a resultant potential for injury to them.
The deceleration phase is manifested by large eccentric muscular forces of the posterior shoulder girdle to decelerate that rapid internal rotation of the acceleration phase.20 Deceleration begins after ball release and ends when the arm reaches 0 degrees of internal rotation. The posterior shoulder girdle is active in this phase, including the scapular muscles, rotator cuff external rotators (particularly the teres minor), and the posterior deltoid. Because of these large eccentric contractions, injury is common in this phase (Box 44-3).
Because of the high risk of overuse injury in the young pitcher’s throwing arm, U.S. baseball has developed age-based pitch count guidelines to decrease this risk (Table 44-3).83 For similar reasons, curve balls and sliders should not be pitched until the athlete reaches puberty. It is also recommended that young pitchers not compete in baseball more than 9 months per year. During those 3 “off” months, they should not compete in other overhead arm sports, such as competitive swimming or javelin throwing.
Running
Notable differences are observed between a walking gait cycle (see Chapter 5) and a running gait cycle.120 One in particular is a third phase in running called the float phase. Float is a period when neither foot is in contact with the ground. It occurs at the beginning of initial swing and the end of terminal swing (Figure 44-7).
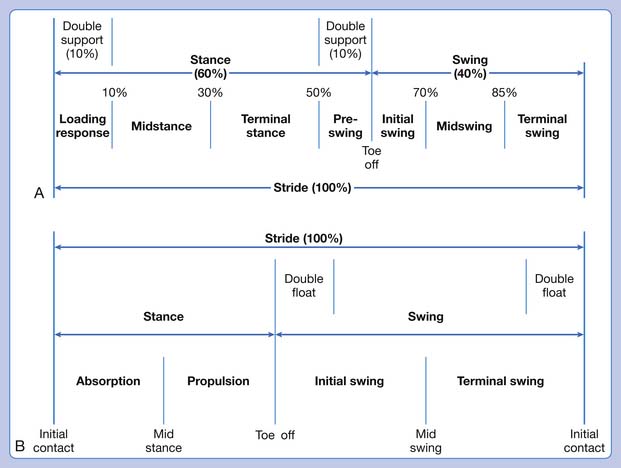
FIGURE 44-7 A comparison of the walking (A) and running (B) gait cycles.
(Modified from Ounpuu s: The biomechanics of walking and running, Clin Sports Med 13(4): 843-863, 1994.)
Faster running also changes foot contact.168 In slower running and walking, contact is typically heel to toe. As running speed increases, foot strike occurs with the forefoot and heel simultaneously, or the forefoot strikes initially followed by the heel lowering to the ground. In sprinting, the athlete maintains weight-bearing on the forefoot from loading response to toe-off.
Swimming
During the propulsive phases of swimming, the arm is moved through adduction and internal rotation starting from a stretched position of abduction and external rotation. The pectoralis major and latissimus dorsi are the major contributors to this motion; however, the serratus anterior and the internal rotator function of the subscapularis and teres major assist.156
General rehabilitation and prehabilitation principles have been established for swimmers with shoulder pain with which all sports medicine clinicians should be familiar. The overarching principle is that most shoulder pain in swimmers (impingement and rotator cuff tendinopathy) is due to dynamic muscle imbalances, weakness, and biomechanical faults, and not hard anatomic factors. A major tenet of shoulder rehabilitation for the swimmer is scapular stabilization, with a prime focus on endurance training of the serratus anterior and lower trapezius. The serratus anterior is a muscle of particular focus because it has been demonstrated to function at 75% of its maximum test ability in swimming and is active throughout the swim stroke cycle.143 Other tenets of shoulder rehabilitation in swimmers include stretching the internal rotators and posterior capsule and cervical and thoracic mobilization.
Jumping and Landing
The biomechanics of jumping and landing in sports is particularly well researched in the setting of noncontact anterior cruciate ligament (ACL) injuries of the knee. Noncontact ACL injuries occur more frequently with the knee in less flexion.172 In this position there are greater knee extensor loads with greater forces creating anterior tibial translation and subsequent ACL injury. A well-defined gender difference is observed in jumping and landing mechanics that is likely one reason for the higher rate of noncontact ACL injuries in female athletes.29 Female athletes land more erect with less knee and hip flexion. They land with less hip external rotation and abduction. They also generally have an imbalance of increased quadriceps to hamstrings activation ratio, creating greater knee extension and lesser knee flexion forces. One goal of ACL injury prevention programs is to improve jumping and landing technique by increasing knee and hip flexion during landing and balancing the quadriceps to hamstring activation ratio.
Pharmacology in Sports
“Doping” refers to any substance or method used to increase performance, possibly at the detriment of the health of the athlete or the ethics of the competition.43 WADA was created to unify the control of the fight against doping. WADA rulings are accepted by all National Olympic committees, the International Olympic Committee (IOC), Paralympics committee, national governments, and international sports federations. The agency, based in Montreal, Canada, consists of government representatives from all continents and members of the Olympic movement. The World Anti-Doping Code was developed in 2003 and enforced in 2004, with a complete listing of banned substances and methods.43 A brief history of doping in sports is presented in Box 44-4.
BOX 44-4 History of Doping and Drug Monitoring
Modified from Calfee R, Fadale P: Popular ergogenic drugs and supplements in young athletes, Pediatrics 117(3):e577-589, 2006; de Rose EH: Doping and sports. In Clinical sports medicine, Philadelphia, 2007, Saunders; Silver MD: Use of ergogenic aids by athletes, J Am Acad Orthop Surg 9(1):61-70, 2001.
A summarized list of substances banned by WADA is available online. Banned substances are divided into those that are banned in and out of competition and those that are banned in competition only.170 The lists of drugs and supplements banned by the National Football League (NFL), National Collegiate Athletic Association (NCAA), and other organizations are also available online.114
When an athlete has an illness or condition that requires treatment with a banned medication, a therapeutic use exemption (TUE) can give that athlete the authorization to take the needed medicine. Per WADA, all international federations and national antidoping organizations must have a process in place whereby athletes with documented medical conditions can request a TUE.69
Therapeutic Drugs
Analgesics
Acetaminophen can be linked to decreased muscle building after exercise (to an extent similar to that of ibuprofen). Prostaglandins are normally released after eccentric resistance exercise. This response might be blunted after consumption of maximal doses of ibuprofen or acetaminophen, profoundly influencing the anabolic response of muscle to this type of exercise.155
Antiinflammatories
One study found that 15% of high school football players used nonsteroidal antiinflammatory drugs (NSAIDs) daily.160 Although the pain relief provided by NSAIDs might enhance performance, NSAIDs are not considered ergogenic. NSAIDs can mask pain and interrupt a natural defense mechanism for preventing injury. Because of their antiinflammatory effects, NSAIDs likely inhibit the production of prostaglandin E2, which is known to play a role in bone healing.125 Consequently, in those with suspected or known fractures, NSAIDs might be contraindicated.
Corticosteroids are potent antiinflammatories. In general, their use is prohibited by WADA when given orally, rectally, intravenously, or by intramuscular injection. Topical preparations for skin, eye, ear, nose, or buccal cavity, or for iontophoresis are allowed. For applicable athletes, epidural or intraarticular steroid injections or inhaled steroids require a TUE.170
Antihypertensives
Experts recommend diuretics as first-line treatment of hypertension, possibly with early addition of a β-blocker or angiotensin-converting enzyme inhibitor (ACE-I).150 Because of the side effect profile diuretics and β-blockers portend to athletes, however, ACE-I or calcium channel blockers can be considered first-line agents. The detection and management of hypertension and the efficacy of various agents are beyond the scope of this chapter. Rather, this discussion will focus on the aspects of these medications that impact athletes.
Diuretics can decrease plasma volume, cardiac output, and peripheral vascular resistance. Dehydration and electrolyte alterations might result in cramps or even heat stroke. For amateur athletes, the benefits of antihypertensive therapy with diuretics likely outweigh the risks. In the case of elite athletes, diuretics are banned in part for their theoretical ability to increase urine output and mask use of other banned agents (although this method rarely works optimally).125
β-Blockers can reduce exercise tolerance by increasing perceived effort. They can also inhibit glycolysis and glycogenolysis with resulting hypoglycemia after exercise. The negative chronotropic effects of β-blockers can decrease heart rate recovery after exercise. β-Blockers are banned in certain sports because of their anxiolytic effects.125
Diabetes Drugs
Insulin doses might need to be adjusted for persons with insulin-dependent diabetes starting a new exercise program. A 20% to 40% reduction is typical because of increased insulin sensitivity with exercise. High-intensity exercise (i.e., greater than 80% VO2max) can cause a temporary increase in blood glucose secondary to increased sympathoadrenal activation. In that situation, supplemental insulin, if used, should be given at a smaller dose than given for hyperglycemia at rest.13,81
Intramuscular injections of insulin should be avoided because muscle contraction can accelerate insulin absorption. Heat can increase absorption rates of insulin, whereas cold can decrease absorption rates. Therefore athletes with insulin-dependent diabetes mellitus should avoid modalities that use extremes of temperature, for example, hot or cold whirlpools. Extreme ambient temperature can also reduce insulin action in athletes.81
Asthma Drugs
Exercise-induced bronchospasm (EIB) can be treated effectively with a short-acting β-agonist, such as albuterol, within 15 minutes before exercise.150 If not sufficient to prevent symptoms, cromolyn (a mast cell stabilizer) can be added. Inhalation of either cromolyn sodium or a β-agonist, or both, 15 minutes before exercise is almost always successful in blocking EIB and airway inflammation.93
For patients who have chronic persistent asthma (forced expiratory volume in 1 second <80% of predicted and symptoms greater than twice a week), inhaled corticosteroids are standard treatment. Inhaled corticosteroids do not appear to have ergogenic or anabolic effects.125
Performance-Enhancing Drugs
Anabolic Steroids
It is estimated that 1 to 3 million athletes in the United States alone have used anabolic steroids (AS),145 with annual market sales well in excess of $100 million.152 The Centers for Disease Control and Prevention found an overall prevalence of lifetime steroid use in females, grades 9 to 12, to be 3.2%.104 Furthermore, as many as 1 in 10 steroid users is a teenager.94 One study found that 6.3% of high school varsity football players were current or former AS users.63
AS have three general effects that enhance athletic performance. By binding androgen receptors, AS stimulate messenger RNA synthesis, increasing structural and contractile protein synthesis94,152 and producing an anabolic state.22 AS are also anticatabolic via competitive inhibition of the glucocorticoid receptor, inhibiting the catabolic effects of cortisol,152 preserving muscle mass.22 Finally, AS have emotional effects, pushing athletes to train more intensely and more often.22
Because AS are illegal, studying their health risks and side effects is a challenge. Inconsistent formulations, dosing, and training habits make it difficult to derive statistically sound conclusions. Some studies show minimal effects on body composition and strength, whereas others show that supraphysiologic doses of testosterone (or its derivatives) can lead to an increase in lean mass and muscle size in humans (Table 44-4).152 Typical users of steroids can take 10 to 40 times the prescribed dosage for disease states.63,80,104,152 Users often share needles, at a rate of up to 25% in adolescent users, with reports of HIV, hepatitis B and C, and abcesses.152 Premature deaths have resulted from AS use, most commonly as a result of suicide and acute myocardial infarction.80
Table 44-4 Negative Effects of Anabolic Steroids
| System | Effects |
|---|---|
| Cardiovascular | |
| Hepatic | < div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|