CHAPTER 98 Spondylolisthesis: Epidemiology and Assessment
INTRODUCTION
Etymologically, the term spondylolisthesis derives from Greek roots spondylos (vertebra) and olisthesis (to slip or slide down). It is now well established that spondylolisthesis is a broad group of disorders with the common basis of slippage of a vertebra over another vertebra. Spondylolisthesis was described as early as 1782 by a Belgian obstetrician who noted narrowing of the birth canal due to gross displacement of the fifth lumbar vertebra over the sacrum.1 Killian first used the term spondylolisthesis in 1854 to describe the displacement of fifth lumbar vertebra over the sacrum.2 Far-reaching anatomic studies by Naugebauer in 1888 showed that the forward displacement could occur by a defect in the pars interarticularis and less commonly with an intact but elongated pars.3 The direction of the spondylolisthesis or slippage is defined according to the displacement of the upper (olisthetic) vertebra as in anterolisthesis or retrolisthesis. The intervertebral discs, superior and inferior articular process (also referred to as zygapophyseal joints or facet joints), ligaments and paravertebral muscles work together to provide segmental stability.4–9 Dysfunction of the disc and horizontalization of the lamina and the articular process have been implicated as factors responsible for the development of spondylolisthesis.10–13 This may also occur if there is weakening of the supporting ligaments, muscular weakness or degenerative changes of the articular processes. The upper lumbar vertebrae are subjected to posteriorly oriented sheer forces and the lower lumbar vertebrae to anteriorly directed forces. During the aging process, the intervertebral discs undergo degenerative changes resulting in the loss of water and elasticity.5 Disc height is reduced, leading to loss of the intervertebral disc space height that leads to spinal instability. The vertebrae may begin to slip relative to another vertebra.14–18 The L4 and L5 vertebrae are particularly prone to this stress.
CLASSIFICATION
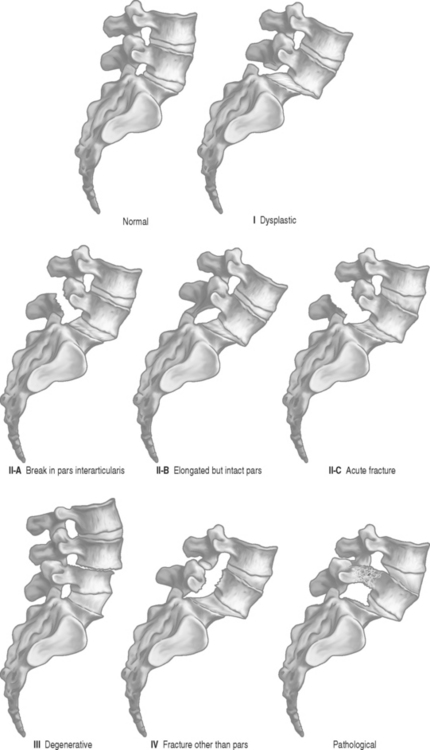
Spondylolisthesis is classified based on the etiology of the slippage of the vertebra. Individual attempts were made to create classification but Wiltse, Macnab, and Newman merged their concepts, leading to the most commonly accepted classification (Fig. 98.1).19
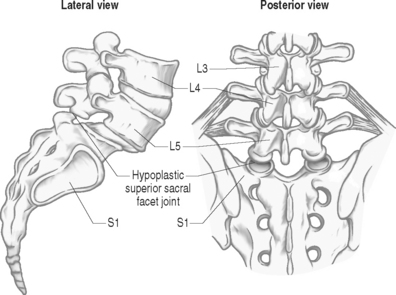
Congenital or dysplastic spondylolisthesis is due to agenesis or insufficiency of the superior articular process (Fig. 98.2). This abnormality can lead to forward slippage due to inability to resist the stress and force placed on these joints under normal conditions. It is more commonly noted in childhood when a patient presents with an episode of severe back pain, hamstring tightness, and rarely a neurological compromise that leads to the work-up. Dysplastic spondylolisthesis typically occurs at the L5–S1 level, and particularly in young patients. It is always accompanied by a congenital anomaly of S1 (usually spina bifida) and often a vertebral arch anomaly of L5. Females are more often affected than males. The fundamental defect is in the L5–S1 facet joint that is dysplastic. A large degree of slip can occur including spondyloptosis in which the L5 has completely slipped off S1.
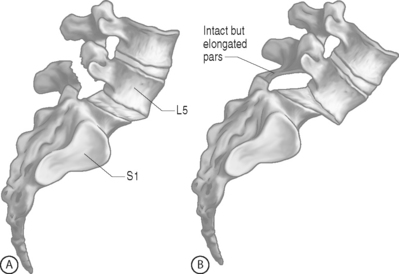
Isthmic spondylolisthesis is the most common subtype and is caused by pars interarticularis defects (Fig. 98.3A, B). Subtype A is hypothesized to occur in individuals who have a congenitally weakened pars, but many do not and the lesion arises de novo. Subtype B includes individuals who have an elongated but intact pars. This is believed to be secondary to repeated fracture and subsequent healing of the stress fracture in the pars. Subtype C is due to acute fracture of the pars interarticularis.
INCIDENCE
The pars interarticularis is the pivotal point where the maximum stress concentration is located. It is the connecting link between the pedicle, lamina, transverse process, and the two articular processes. The defect in the pars interarticularis is due to stress or fatigue fracture, which can allow forward slippage of one vertebra over the adjacent vertebra. The normal lumbar lordosis can lead to forward slippage. In the lumbar spine, isthmic spondylolisthesis occurs with the following frequencies: at the L5–S1 level (82.1%), L4–5 level (11.3%), L3–4 level (0.5%), L2–3 level (0.3%), and other levels (5.8%).20 White men appear to have the highest prevalence (6.4%) and black women the lowest (1.1%). This may indicate a gender and racial difference.21
Degenerative spondylolisthesis is second in frequency only to isthmic spondylolisthesis and is believed to be due to intersegmental instability. It is primarily a condition that affects older adults. Two leading theories on etiology are dysfunction of the intervertebral disc, and the horizontalization of the lamina.11, 13, 22 Degenerative spondylolisthesis occurs more often in women than men, ranging from a ratio of 2:1 to as high as 6:1.23–25 Women who have borne children have a significantly higher incidence of degenerative spondylolisthesis compared to nulliparous women (28% versus 16.7%). In contrast, men have a 7.5% incidence. Sanderson and Fraser suggest that females are more prone to developing degenerative spondylolisthesis, and the incidence of slippage increases with pregnancy.26 A familial component has also been implicated. Ryan reported on 73-year-old twin brothers with symptomatic spinal canal stenosis and lumbar degenerative listhesis involving the L4–5 level.27 In degenerative spondylolisthesis, Vogt et al. noted in radiographs of 788 white women with a mean age of 71.5 years that 73% of the spondylolisthesis was located at L4–5, 28% at the L5–S1 level, followed by 12% at L3–4 level (10% of patients had multilevel listhesis).28 In stark contrast, a study by Merbs on New Mexico Pueblo skeletons revealed 79% of listhesis occurring at the L5–S1 level.23 Prevalence of spondylolisthesis increased with increasing age. Progression of slippage occurs in 30% of patients.29 Due to the inherent increased mobility created by a degenerative spondylolisthesis, it is not surprising that synovial cysts are frequently identified. These mass occupying structures arise from the facet joints and can reside in the lateral foramen or in the central spinal canal.30,31 Degenerative spondylolisthesis was more likely to develop in patients who underwent fusion than in the general population.32
Patients with spondylolisthesis may present with a very broad spectrum of complaints. Symptoms and complaints may also vary over time. Presentation may range from asymptomatic in some patients to having mild through severe back pain which may be intermittent or persistent. In addition, patients may present with or without radicular complaints. There may not be any complaints of back pain despite signs and symptoms of nerve root compression or cauda equina syndrome. The most common pain pattern associated with spondylolisthesis is a dull, aching pain in the back, buttocks, and posterior thigh. The source of pain is likely multifactorial. The pars nonunion may be a source33 and ligamentous stretch may lead to local muscle spasm at the unstable vertebral segment. Disc degeneration is noted in 67% at the level of the slip.34 Saraste’s study of spondylolysis and spondylolisthesis suggests that disc degeneration may contribute to symptoms, as a strong correlation was noted between disc degeneration and low back pain in patients with spondylolysis.35 Often, the central canal is not as compromised, as the neural foramina at the level of the slip and, in some instances degenerative changes may further compromise the neural foramina leading to nerve root compression.36
With an emphasis on healthier lifestyles, many are getting involved in athletic activities. This has led to an increase in participation in various sports at recreational and at more competitive levels. Numerous skeletally immature athletes are also participating in these activities. Many of these growing children are at a higher risk for various musculoskeletal injuries including spinal trauma. Factors that contribute to these injuries includes poor techniques, rapid increase in training frequency, use of improper equipment, inappropriate footwear, and variable playing fields, along with musculoskeletal weakness and inflexibility.37–40
In athletes with persistent back pain, isthmic spondylolisthesis is noted in up 50%. It has a prevalence rate of 4–5% in children at 6 years of age. The prevalence slightly increases by age 18 to 6%.41 The etiology of an isthmic spondylolisthesis is a defective or weakened pars interarticularis that is further injured with repetitive motion or stress. Certain clinical features help distinguish stress fractures from isthmic spondylolisthesis. These include genetic predisposition, rare callous formation, young age of onset, relatively minor inciting trauma, and a low incidence of spontaneous bony union.42 The greatest forces occur at the L5–S1 articulation.38,43 Anatomically, the position of the sacrum creates compressive forces and anterior shear on the neural arch.43–45 Bipedal stance further exacerbates these forces.37 Erector spinae musculature plays an important role in supporting the posterior elements in an erect posture. Extension of lumbar spine leads to closure of facet joints. When additional extension forces are applied, these forces are transmitted to the neural arch.43
It is believed that repetitive motion leads to the higher prevalence of spondylolisthesis seen in athletes. The most commonly implicated movement in injury to the pars interarticularis is hyperextension. Up to 20% of pars defects may be unilateral.46–49 Repetitive rotation motion is implicated in unilateral defects. Football and gymnastics are believed to be the sports with the highest risk, but other sports including hockey, diving, wresting, volleyball, pole vaulting, racquet sports, and weight lifting have also been implicated. A fourfold increase in spondylolisthesis was noted in helicopter pilots in comparison to transport pilots and cadets, suggesting that repetitive minor stress and vibrational force, without acute fracture, can cause lumbar spondylolisthesis.50
DIAGNOSIS
Physical examination may reveal some tenderness to palpation over the involved region. In the late or advanced stages, the patient may present with distortion of the pelvis and trunk. There may be some restriction noted with side-to-side motion along with some guarding, especially in a presentation with acute onset. Forward flexion may be limited due to hamstring tightness. Hamstring tightness is common but it may not be observed in a flexible athlete. Hamstring tightness was believed to be due to traction on the cauda equina; however, all grades of spondylolisthesis can present with hamstring tightness and it is seldom accompanied by neurologic signs.51–53 Several nerve roots (L4 to S3) innervate the hamstring muscles and a very severe single lesion would be necessary to produce such a massive involvement. The development and perpetuation of hamstring tightness may be an attempt by the body to reestablish the patient’s center of gravity by attempting either to control the unstable segment or to rotate the pelvis into a more vertical position. Significant slip can lead to lumbosacral kyphosis and trunk shortening.54–58 Forward slip of the lumbar spine leads to a compensatory thoracolumbar hyperlordosis, which can present with an anteriorly protruding inferior rib cage. In high-grade slips, a clinician may be able to observe a palpable step-off sign or depression at the involved level. Other findings may include tight hip flexors, relative thoracic kyphosis, and positive one-leg hyperextension test. Athletes with lumbar spondylolisthesis may also present with a dull backache that is amplified with hyperextension and rotation motion.54
Gait abnormalities may observed in some patients with spondylolisthesis. Compensation for the hamstring tightness, lumbosacral kyphosis (vertical tilting), compensatory lumbar hyperlordosis, and the flexion deformity at the hips and knees leads to a spondylolisthetic gait. It is characterized by a waddle with limited hip flexion, a wide base of support, and a shortened stride length.52, 54, 57, 59
Neurologic deficits are uncommon and the straight leg raising test is usually negative. Indeed, this is a difficult maneuver to perform because of the previously described hamstring tightness. In nearly half of the patients who require surgical intervention, radicular pain and varying degrees of nerve root dysfunction are present.60–62 The fifth lumbar root is more often involved as it approaches the L5 neural foramina. Osteophytes or hypertrophic facet joints can further affect the compression. Any involvement of bladder dysfunction may be due to involvement of the sacral roots, which can be further evaluated with urologic studies including a cystometrogram.
ASSOCIATED CONDITIONS
Other conditions have been noted to occur with spondylolisthesis. Spina bifida occulta has been reported to be present along with isthmic defects, with a reported incidence of 24–70%. In dysplastic spondylolisthesis, spina bifida occulta occurs in about 40% of the cases. In contrast, the incidence of spina bifida occulta in adults without spondylolisthesis is about 6%. This defect, in which there is incomplete fusion of the posterior arch, likely permits added stresses on the pars interarticularis allowing it to fracture.57, 59, 63, 64 Congenital defects such as sacral spina bifida and hypoplasia of posterior sacral development was found in 94% of dysplastic and 32% of isthmic spondylolisthesis patients.65 Scoliosis is another entity noted in patients with spondylolisthesis. The incidence ranges between 15% and 43%.66–69 Those requiring surgery are noted to have an approximately 30% incidence (range 23–48%). The scoliosis may be due to, or worsened by, muscle spasms. Distortion of the pelvis and trunk may become apparent in the late stages of grade II spondylolisthesis, but are frequently present by the time the slip reaches grade III. Surgery may correct this secondary deformity.53,64,66,70–72 Posterior disc protrusion at the level of the slip is rare, with an incidence approaching 5%.55,56
There have been no reported cases of spondylolysis or spondylolisthesis at birth. The earliest documented case was in a 4-month-old infant whose parents had noted some deformity in the lower back. In that case the spondylolisthesis was confirmed radiographically. The child developed a wide-based shuffling gait with lower extremity in lateral rotation at the age of 15 months.73,74 Rosenberg et al. evaluated 143 lifelong nonambulatory adult patients and found no cases of a pars defect.75 An overall incidence of spondylolisthesis was 4.4% in a group of 500 6-year-olds and it progressed to 6% by adulthood in the same population.63 An overall incidence of spondylolisthesis 8.02% was noted in a group of 3152 athletes evaluated by Soler and Calderon. A higher incidence of 26.7% was noted in throwing sports such as discus and shot put. Gymnastics, a sport that often involves hyperextension, was noted to have an incidence of 16.9%, rowing 16.9%, and swimming 10.2%.76 Elite athletes are not exempt from these findings. Jones et al. compared division 1 college football players’ pre-participation radiographs to controls. It was noted that the rate of spondylolysis was 4.8% in these athletes and 6% in the control group. The rate of spondylolisthesis was slightly less with 3.8% in the group of athletes and 3.6% in the control group.77 Shaffer et al. reviewed questionnaires completed by NFL and 25 NCAA team physicians. The known prevalence of spondylolisthesis was 1%.78 Other studies have reported 10.1–50% spondylolysis rates for down-lineman. Degenerative spondylolisthesis in the cervical spine was noted to have a prevalence of 5.2%.79 Studies by Vogt et al.80,81 did not support a relationship between anterolisthesis and diabetes. Prevalence of isthmic lumbar spondylolisthesis was 5.7% and there was no significant sex difference in a group of diabetics.82 African-American women are 2–3 times more likely to develop anterolisthesis than Caucasian women.81 Oophorectomized Japanese women83 were noted to have an increased prevalence of anterolisthesis, but among older Caucasian women, neither oophorectomy nor use of estrogen was related to the prevalence of listhesis.80 There is support in the literature for a familial component associated with spondylolisthesis. Among first-degree relatives, spondylolisthesis was noted to be 27–69% with the dysplastic type being more prevalent (33%). The familial incidence in first-degree relatives over the age of 10 years was noted to be 40%.84
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree