CHAPTER 59 Cervical Radicular Pain: Injection Procedures
INTRODUCTION
This chapter will review the literature pertaining to the use of epidural space steroid injection (ESI) in the treatment of cervical radicular pain. Epidural injections are utilized to introduce corticosteroid and anesthetic to the epidural compartment and the suspected site of neural injury. There is a plethora of literature describing ESI in the treatment of lumbar radicular and axial pain, and this topic will be comprehensively addressed in a dedicated chapter of this text. Injection therapy has found a particular role in the treatment of lumbar radiculopathy, as a growing body of literature has supported a biochemical and inflammatory injury component in the case of lumbar radicular disorders.1–5 Recent prospective uncontrolled6–9 and controlled lumbar studies10–12 have suggested a significant beneficial response when transforaminal epidural steroid injections (TFESI) are utilized in the treatment of radiculopathy.
While the role of inflammation in the injury process of cervical radiculopathy has largely been extrapolated from this lumbar literature base, several studies have similarly highlighted the biochemical processes likely at play in cervical radicular disorders. In a study of cervical disc specimens removed during discectomy for radiculopathy,13 when compared to control disc samples, significant increases in matrix metalloproteinase, nitric oxide, prostaglandin E2, and interleukin-6 were observed. A later study by this same author14 revealed herniated cervical disc specimens to be biologically responsive with resultant increased levels of nitric oxide, interleukin-6, and prostaglandin E2 when exposed to interleukin-1β. A more recent immunohistochemical investigation of herniated cervical intervertebral discs15 has revealed the presence of inflammatory processes and neovascularization, increased levels of matrix metalloproteinase, and a marked increase in nitric oxide production when compared to control samples.
Similar to the lumbar literature, which has revealed abnormal radiographs and compressive lesions in asymptomatic individuals,16–18 studies of the cervical spine also reveal abnormal radiographic findings in patients without cervical pain or symptoms of radiculopathy.17,19,20 In a cervical MRI study of asymptomatic patients,19 20% of subjects over 40 years of age were observed to have foraminal stenosis, and 10% of cases under 40 years of age revealed a herniated disc. In an earlier study of asymptomatic subjects employing cervical myelography,17 21% of cases were observed to have nerve root filling defects. These significant radiographic and potentially compressive findings in asymptomatic individuals suggest that a purely mechanical injury construct is too simplistic.
Also, parallel to the lumbar radiographic literature,21–24 which has revealed regression of symptomatic disc lesions with a tendency for symptoms to improve prior to radiographic regression, cervical studies have demonstrated a regression of symptomatic cervical disc pathology.25–27 Both CT26 and MRI25,27 studies have revealed the largest disc herniations to reduce most in size. In greater than 75% of cases a 35–100% size reduction in disc lesions has been observed, and a greater likelihood of resolution is realized in cases of disc extrusion. In combination, these cervical-specific biochemical and radiographic studies set the stage for a mechanochemical injury construct in cases of cervical radiculopathy. It is the biochemical or inflammatory component of neural injury that is the intended target of ESI therapy. The remainder of this chapter will review the available literature addressing this treatment approach in cervical radicular disorders.
BACKGROUND LITERATURE
Similar to lumbar ESI, injections to the cervical spine can be performed through either an interlaminar or transforaminal approach. During the performance of interlaminar injections, medication is most reliably placed in the epidural space with the use of fluoroscopic guidance. This fact has been established in the lumbar spine injection literature. White28 revealed a 25% miss rate when interlaminar injections were performed by an experienced anesthesiologist without the use of fluoroscopy. The inaccuracy of cervical interlaminar injections performed without guidance has more recently been reported.29 In this multicenter retrospective analysis, a first-attempt miss rate of 53% was observed when the typical loss of resistance technique was utilized. When medication was successfully introduced to the epidural space, ventral spread of medication was observed in only 28%. While interlaminar ESI can be performed with technical success, particularly with the use of fluoroscopic guidance, there are anatomic advantages to performing ESI through a transforaminal approach.30 With interlaminar injections, medication is typically deposited dorsally, posterior to the thecal sac. The spinal pathology that serves as the intended target of ESI is typically located in the ventral spinal canal. TFESI provides the interventionist an opportunity to better control the flow of injectant and target the specific level of segmental pathology. In addition, and of particular importance in the cervical spine, the transforaminal injection approach allows for foraminal and extraforaminal spread of medication. The complexity of the cervical anatomy requires fluoroscopic guidance if TFESI is to be performed.
In addition, and similar to ESI in the lumbar spine, the use of fluoroscopic guidance and contrast enhancement allows the interventionist to avoid vascular uptake, which would prevent the successful placement of medication at the injury site. Indeed, this is a significant issue for two reasons. The general notion is that a local instillation of glucocorticoid provides greater benefit than using an oral or parenteral route. If the medication is infused intravascularly, this proposed benefit will be obviated. A second and potentially more important reason to avoid intravascular uptake is the possibility of inadvertent arterial injection with resultant neural injury. Such complications will be further reviewed in the concluding section of this chapter. Several studies underscore the importance of using fluoroscopy during spinal injection procedures. An 11.2% incidence of venous uptake has been observed by fluoroscopy during lumbar TFESI, necessitating needle repositioning to achieve a satisfactory epidurogram.31 An earlier study of fluoroscopically guided lumbar injections32 revealed a 10.9% and 10.8% incidence of vascular uptake during transforaminal and caudal injections, respectively, compared with a 1.9% incidence when utilizing an interlaminar approach. In a prospective study of 337 cervical TFESI,33 the overall rate of fluoroscopically visualized venous uptake was 19.4%. Observation of blood in the hub of the injection needle was determined to be unreliable in the detection of vascular uptake, with a 97% specificity but only a 45.9% sensitivity observed. These studies highlight the role of fluoroscopic visualization as the only reliable means of observing venous uptake, as the sensitivity of blood observed in the spinal injection needle or tubing is unacceptably poor.
While the majority of background literature addressing cervical ESI describes an interlaminar injection approach, performed with and without fluoroscopic guidance, more recent clinical studies employ fluoroscopically guided TFESI. While there is an apparent trend for more recent cervical literature to describe a transforaminal (TF) approach, there remains a wide discrepancy in cervical injection techniques employed by the interventional spine community. A recent national survey of anesthesia practices found that fluoroscopic guidance is employed during cervical ESI in 73% of private practices but in only 39% of academic institutions.34 Similarly, TFESI was more likely to be employed by 61% of private practices but only 15% of academic centers.
INTERLAMINAR INJECTION LITERATURE
Cervical ESI clinical outcome studies have been published, but the body of literature is not as vast as that addressing lumbar ESI. To date, the overwhelming majority of these studies are uncontrolled and retrospective. The introduction of cervical epidural injections initially arose as a result of the described successes in treating lumbar axial and radicular pain with epidural injections of corticosteroid. The earliest reference to cervical epidural injection therapy was in a 1972 study describing the role of intra- and extradural corticosteroids.35 In the 1980s, several studies reported clinical outcomes following cervical epidural injection therapy.36–40 These studies included patients with a variety of clinical presentations including radiculopathy, cervical pain, reflex sympathetic dystrophy, postherpetic neuralgia, and viral brachial plexitis. Three uncontrolled studies published in 1986 which included a total of 180 patients describe a combined result of greater than 90% pain relief in 20–24% of patients and little to no response in 12–24% of cases.37–40 In these studies, an interlaminar injection approach was performed without fluoroscopic guidance. In one of these studies38 that retrospectively analyzed 25 patients receiving an average of 1.5 injections, patients with superior outcomes were more likely to present with radicular pain and sensorimotor deficits on examination. In a 1988 study41 of 16 patients presenting with suspected cervical radicular symptoms without a radiographic correlate, up to three blind interlaminar ESI were performed. After 1 year and questionnaire follow-up, 12 patients described their pain as improved and 50% of those patients with initial neurological deficits reported improvement in these symptoms. Additional outcome studies published in the 1990s36,40,42 describe approximately 40% of 100 combined patients realizing relief of 70% or greater. In one of these studies,36 which included 58 patients followed for 6 months, 41.4% demonstrated an excellent response, defined as greater than 90% pain relief. An excellent outcome was described to be more likely in those patients with radiographic evidence of spondylosis or subacute cervical strains.
A 1993 retrospective analysis of 100 patients43 receiving cervical interlaminar ESI attempted to identify patient characteristics that would serve as reliable predictors of clinical outcome. In each case, a mean of 2.35 injections were performed in a nonfluoroscopically guided (blind) fashion at the level of suspected segmental pathology. Forty-one percent of the total patient population described greater than 50% pain relief and at least a partial return to normal activities at a mean of 14.7 months follow-up. Symptom duration prior to injection and a history of trauma did not prove reliable in predicting clinical outcomes. Older patients and those with radicular pain were observed to realize more lasting pain relief. In this study, patients with a herniated disc or a motor deficit were observed to do worse. Patients with cervical spondylosis or stenosis demonstrated a superior outcome. The authors concluded that patients with clinical radiculopathy or radicular pain were more likely than patients with axial pain alone to realize relief from cervical ESI. Complications in this study included a 2% incidence of dural puncture and 4% incidence of vasovagal events.
In a 1996 study of 26 patients44 treated nonsurgically for cervical radiculopathy associated with a herniated disc, 20 patients demonstrated a good or excellent outcome. Each of these patients was fully satisfied with the outcome and reported little to no residual pain or activity limitation. Nineteen of these 20 successes initially presented with cervical disc extrusion. The outcomes following injection therapy in this study cannot be presented with any certainty, as only nine of these patients received a single fluoroscopically guided cervical ESI performed in either an interlaminar or transforaminal fashion. Other nonsurgical treatment approaches employed in this study included relative rest, icing, the use of a cervical collar, nonsteroidal anti-inflammatory agents, and in most cases, an oral corticosteroid taper. Similarly, in a frequently referenced 1999 study45 which prospectively studied 246 patients nonrandomly assigned to either conservative or surgical treatment for cervical radiculopathy, cervical injection therapy was employed in the conservative care group. Spinal injections employed were described as nerve blocks, ESI, or facet blocks. The body of the paper suggests that injections were utilized in 13% of patients, and therefore outcomes following injection therapy in this paper are unclear. In this paper, both groups of patients realized significant improvements in pain and functional status.
DIAGNOSTIC SELECTIVE NERVE ROOT INJECTION
While there are many references alluding to the utility of lumbar diagnostic selective nerve root block (SNRB), performed through a fluoroscopically guided transforaminal approach, the role of diagnostic cervical injections remains poorly defined. The specificity and sensitivity of lumbar diagnostic nerve root injections has been estimated at 87–100%46,47 and 99–100%,48,49 respectively, with corroborative surgical lesions observed. In a study of patients treated with anterior cervical decompression and fusion,50 75 patients demonstrated a positive response to a preoperative diagnostic cervical SNRB. Diagnostic injections were performed with fluoroscopic guidance, contrast enhancement, and 1 cc of 1% lidocaine. The study describes 65 of 75 patients realizing immediate postoperative relief during a recovery room assessment. In a more recent report,51 the preoperative diagnostic utility of lumbar and cervical selective nerve root injections has similarly been assessed. In this study, 101 patients were included, but only 18 were cervical patients. Nerve root localization was confirmed with both contrast enhancement and symptom provocation utilizing a nerve root stimulator. Anesthetization was performed utilizing 0.5–0.75 cc of 2% lidocaine. A 90% reduction in symptoms during the postinjection assessment was considered a positive response. Of those patients who underwent surgery with a positive preoperative diagnostic injection, 91% reported a successful surgical outcome. Of the 10 patients who demonstrated a negative response to preoperative injection, 60% reported a successful surgical outcome. This difference in outcomes was statistically significant (p=0.05).
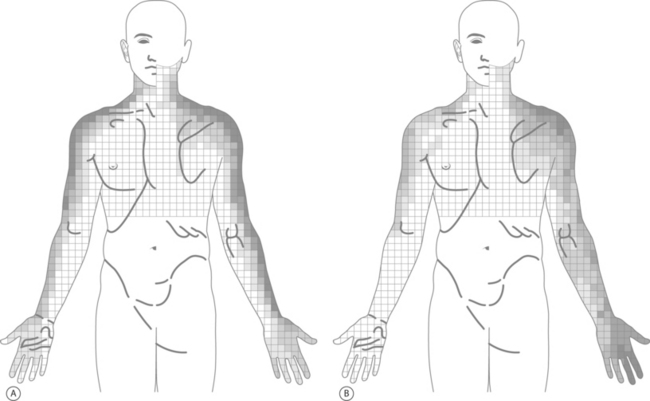
In a novel study,52 the symptoms resulting from cervical nerve root provocation during diagnostic SNRB were recorded and dynatomal maps described. In this study, 87 patients underwent 134 cervical nerve root stimulations. The C4 through C8 nerve roots were studied and symptom distributions recorded utilizing more than 1000 bits of data compiled upon a 793-body-sector bit map containing 43 clinically relevant body regions. The resultant dynatomal maps differed considerably from the classic cervical dermatomes described by Foerster53 and Keegan and Garrett.54 Highlights from the dynatomal maps include C5 root stimulation resulting in symptoms radiating as distal as the forearm in only 14%, C6 symptoms incorporating the ulnar hand and fifth digit in 37% and 30%, respectively, C7 symptoms uniquely referred to the anterior head and to the chest as frequently (17%) as to the middle finger, and C8 symptoms extending to the thumb as often as digit five (Fig. 59.1). As the authors explain, these differences between the dynatomal maps and more classically described dermatomal distributions likely arise in part from limitations in the more classic studies’ methodology, the more frequent existence of cervical intrathecal anastomoses,55,56 and varying nerve root contributions to the brachial plexus.
In the author’s practice, diagnostic cervical SNRB are employed when diagnostic uncertainty remains. As described later in this chapter, the level of segmental pathology is often clarified through a review of radiographs and a detailed physical examination. In those cases in which diagnostic uncertainty remains, electrodiagnostic studies can be utilized. When electrodiagnostic studies fail to confirm a level of segmental pathology, SNRB can be utilized in an effort to more definitively identify the pain generator. In the cervical spine in particular, where dynatomal overlap is more frequently observed, the clinician needs to be cautious in assigning a level of radicular involvement when the physical examination and radiographs are not clearly corroborative. In other cases, radicular pain may be clinically suspect, but a radiographic correlate is not appreciated, i.e. following whiplash or in the setting of a chemical radiculitis. In such instances, diagnostic SNRB are employed. It is the author’s goal during diagnostic injections to achieve a contrast pattern which reveals the exiting nerve root and dorsal root ganglion without epidural spread to adjacent levels. This can often best be achieved by positioning the spinal needle adjacent the posteriorly situated superior articular process but with a more inferior and lateral position in the foramen (Fig. 59.2). Anesthetization is performed with 0.8–1.0cc of 2% lidocaine. The patient’s response to diagnostic injection is considered positive if an 80% symptomatic reduction is realized during the postinjection assessment performed approximately 20 minutes after injection. Pain ratings and diagrams are completed before and after injection, and typically provocative maneuvers are performed during the assessment phase.
TRANSFORAMINAL INJECTION LITERATURE AND DIAGNOSTIC SUBSETS
A 1996 prospective uncontrolled study of 68 consecutive cervical radiculopathy patients reported outcomes following injection therapy.57 Each patient described radicular pain that radiated at least as distally as the forearm. All patients except for one presented with an associated neurologic deficit in the form of either reduced strength, sensation, or a diminished reflex. The average duration of symptoms was approximately 2 months. All but one patient demonstrated a radiographic finding which was believed to correlate with symptoms. In 70% of cases a corroborative intervertebral disc protrusion or herniation was described, and in 30% spondylotic foraminal encroachment was observed. The patients in this study were treated with three possible injection techniques. Initially, a cervical or brachial plexus block was performed using anatomic landmarks without image guidance. If this injection technique proved helpful, it was repeated. Otherwise, a fluoroscopically guided contrast enhanced TFESI was performed. Once again, if this approach proved helpful it was repeated. If this failed to offer relief, a fluoroscopically guided interlaminar ESI was performed. Each patient received an average of 2.5 injections, and in 62% of cases a TFESI was employed. Twenty-nine percent improved with the plexus block approach and 16% received interlaminar injections. No complications were reported in this study. The average time to clinical discharge in this study was 7 months. At that time an average VAS of 0.6 was recorded, all patients had returned to work, and partial or full neurologic recovery was described in 47% and 46%, respectively. An additional phone interview was conducted with 93% of patients at an average of 39 months following treatment. By this survey, 76% of patients were pain free and the other 24% reported an average pain score of 2/10. Eighty-six percent reported an absence of parasthesias, and 73% reported no residual weakness. No patient required surgical intervention. In addition to these described clinical outcomes, the authors share an interesting observation in the discussion section of their paper. This same group of investigators performed a study with similar methodology and interventions in the treatment of patients with lumbar radiculopathy.58 In that study, 14% of patients ultimately required surgical intervention, leading the authors to speculate that the prognosis for recovery following injection therapy might be more favorable for the cervical radiculopathy population.
In a 2001 prospective study of 32 patients with cervical radiculopathy,59 fluoroscopically guided TFESI were similarly employed. Inclusion criteria included a persistence of symptoms for at least 2 months, high radicular pain scores on a 10 point scale, and a radiographic correlate such as a focal disc lesion or degenerative foraminal stenosis. In 26 of 32 cases, spondylosis was described rather than a disc herniation. Injections were performed in the seated position and with fluoroscopic guidance but without contrast enhancement. Patients were clinically followed for 6 months. In 27 of the 34 levels treated only one injection was performed, and in the remaining seven, a second injection was administered. At 6-month follow-up, a good or excellent result, defined as at least 50% pain relief and requiring little to no medical treatment, was observed in 56% of patients. No long-term complications were reported. These outcomes are inferior to those described by the previous 68 patient study in which no patients described ongoing debilitating pain. There are several differences between these studies in methodology and patient populations. First, the majority of the patients in this study presented with radiculopathy suspected as arising from corroborative degenerative foraminal stenosis as opposed to a herniated disc. Additionally, contrast enhancement was not utilized during injections, and repeat injections were not employed in the majority of cases.
Transforaminal injections performed with CT guidance have been utilized in a retrospective study of 30 patients presenting with cervical radiculopathy.60 In this study, 16 patients presented with suspected corroborative degenerative foraminal stenosis and 14 with a focal disc protrusion. Patients were excluded if a strength deficit was evident. The average symptom duration prior to injection therapy was 2.7 months. Patients were evaluated at 2 weeks and 6 months after injection therapy and the pain response was assessed. Injection procedures were performed with CT guidance and contrast enhancement. The mean visual analog score prior to injection therapy was 6.5, and this was significantly reduced (p<0.001) to 3.3 at 2 weeks after the injection procedure. An outcome of excellent was assigned to those with greater than 75% pain relief and good for those with at least a 50% pain reduction. Eighteen patients realized a good or excellent outcome 2 weeks after the first injection and this was sustained at 6 months without further injection therapy. Only 3 of 12 patients who realized an initial fair or poor outcome received a second injection. Two of these patients realized excellent outcomes that were sustained at the 6-month follow-up. Initial pain intensity, symptom duration, and radiographic correlates were not found to reliably predict clinical outcomes. No procedural complications were reported.
In an additional study of CT-guided transforaminal injection therapy for radicular pain,61 outcomes of 160 patients were retrospectively analyzed. In 18 of these cases, patients presented with cervical radicular pain. The remainder of the patients were treated for symptoms of thoracic or lumbar origin. Patients presented with variable radiographic correlates in this study, including degenerative foraminal stenosis, disc herniation, postoperative fibrosus, or no visible radiographic abnormalities. The majority of patients, approximately 80%, received only a single injection. Eleven of these 18 patients (61%) realized symptomatic improvement, and it is extrapolated from the data that in 80% of these cases a greater than 50% reduction in radicular pain was realized. It would also appear after a review of this report that approximately 66% of those cases with improvement demonstrated sustained relief by phone interview at a mean of 110 days following treatment. For the study group as a whole, there was no apparent correlation between radiographic findings at the symptomatic level and outcomes. There was a suggestion of greater efficacy of injections for cervical patients, in which 57.9% of injections were categorized as effective, when compared to thoracic and lumbar patients, in which a 50% and 48% efficacy were assigned, respectively.
In an effort to assess outcomes following cervical TFESI in a more diagnosis-specific fashion, the author’s research group retrospectively analyzed the data in three separate studies.62–64 The first of these three studies62 included 20 subjects with cervical radicular pain arising from atraumatic spondylotic foraminal stenosis. Each patient presented with radiographic evidence of foraminal stenosis at the symptomatic level. A diagnosis of level-specific radiculopathy was confirmed either by a corroborative myotomal strength deficit or reflex abnormality, electrodiagnostic evidence of myotomal denervation, or a positive response to a confirmatory diagnostic SNRB. Patients’ average symptom duration prior to treatment was 5.8 months. At initial presentation, the average VAS was 6.9. Follow-up data collection was performed by an independent reviewer by phone interview at an average of 21.2 months. An average of 2.2 injections was performed in each case. At the time of follow-up, six patients (30%) had proceeded with surgical decompression. An overall good or excellent result was described by 12 patients (60%). To be categorized as a good or excellent outcome, patients needed to demonstrate a pain score of four or less on a ten point scale, be working full time, utilizing no more than prescription NSAIDs to control pain, and demonstrate high patient satisfaction scores. The average recorded verbal pain score at the time of follow-up was 2.0. A significant improvement (p=0.001) in the average pain score was observed. A significant reduction (p=0.0005) in medication usage was also observed at the time of follow-up. At follow-up, only one patient was requiring opioid analgesics and nearly 86% were utilizing no medications or over-the-counter agents. An analysis of patient characteristics at initial presentation, including associated weakness and distal extent of radicular pain, did not predict clinical outcomes with statistical significance. A significant relationship was noted between patient age and satisfaction with treatment, with younger patients providing the highest patient satisfaction scores (p=0.0047).
In the second and third published studies, patients with a traumatic symptomatic onset were described. In the second paper,63 the efficacy of cervical TFESI was retrospectively analyzed in 22 patients who presented with radicular pain following a whiplash event and whose imaging did not reveal a radiographic correlate at the symptomatic level. In this study, patients were excluded if their examination revealed a strength or reflex abnormality or if electrodiagnostic studies revealed denervation. Each patient demonstrated an initial positive response to a diagnostic SNRB to confirm the symptomatic level. Patients’ average symptom duration prior to diagnostic injection was 6 months. Follow-up data were collected by phone interview at an average of 33 weeks after the final therapeutic injection. Outcome categorization was based upon a consideration of work status, medication use, and Oswestry scores. An overall 14% good or excellent outcome was observed. To be labeled good or excellent, the patient was required to be working at least full time with modifications, utilizing no more than prescription NSAIDs for pain control, and demonstrate an Oswestry score of 21–40, suggestive of more ‘moderate’ disability. When considering patient stratification before and following treatment, a significant change was not observed. In patients with initial higher levels of function, a more pronounced pain reduction was reported at the time of follow-up.
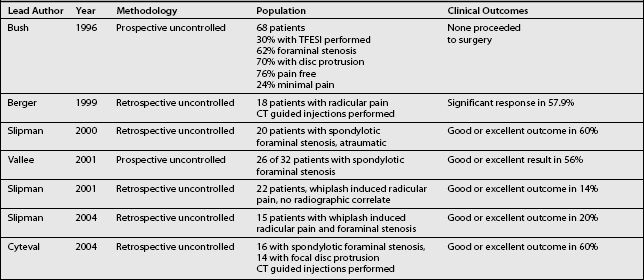
The third64 of these three studies similarly investigated patients with a traumatic symptomatic onset but with radiographs revealing degenerative foraminal stenosis at the symptomatic level. This study included 15 patients presenting with a median symptom duration of 13 months. The symptomatic level was determined by the presence of a corroborative strength deficit or reflex abnormality, electrodiagnostic evidence of myotomal denervation, or a positive response to a diagnostic SNRB. An average of 3.7 injections was performed at each symptomatic level, and follow-up data were collected by phone interview at an average of 20.7 months following treatment. Similar to the first of these three studies, outcomes were determined through a consideration of work status, pain scores, medication use, and patient satisfaction. While a significant reduction (p=0.0313) in pain scores was observed, an overall good or excellent outcome was observed in only 20%. Six patients underwent surgery, and only one of these realized a good or excellent postoperative outcome. The outcomes from these three studies as well as the previous cervical TFESI studies described in this chapter are summarized in Table 59.1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree