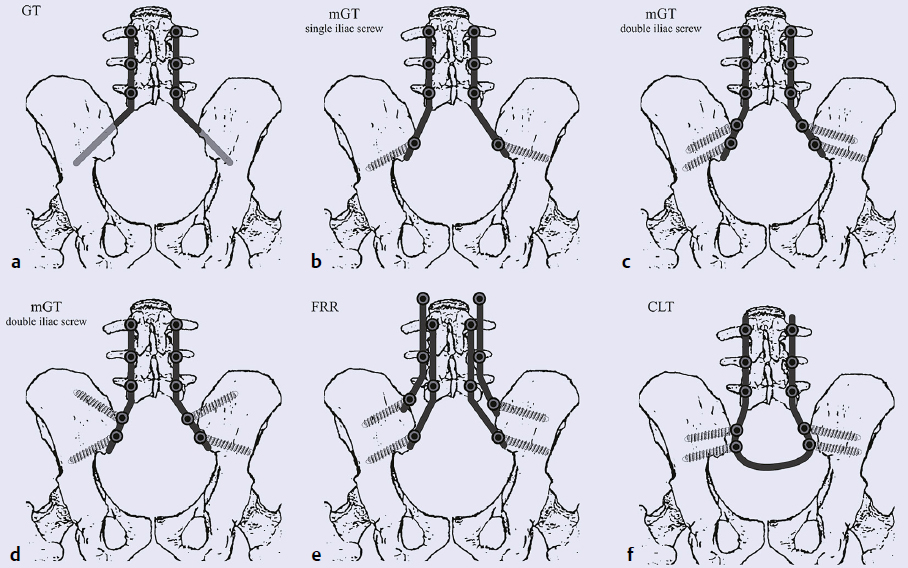
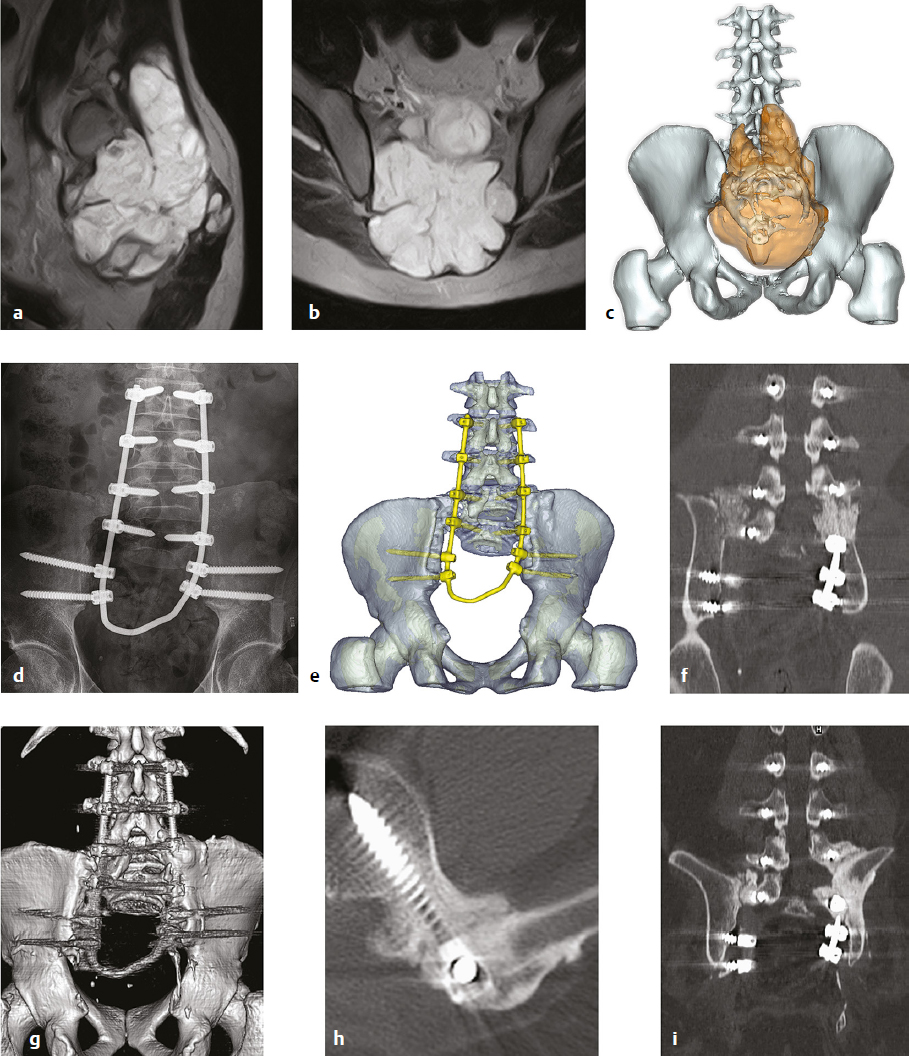
13 The tumorous pathologies of the lumbosacral junction requiring surgical intervention are very challenging even for the most experienced spine surgeons. Tumors of this region often grow insidiously without specific symptoms, reaching a large size that makes their complete removal a complex feat. Due to the localization, special issues should be considered when investigating all aspects of the local anatomic and biomechanical properties irrespective of the particular oncological approach. Achievement of the optimal oncosurgical resection margins often entails potential functional losses, resulting in psychological issues that should be considered during the planning process. The patient should be prepared accordingly by the surgeon and psychologists for this technically demanding surgery. In metastatic lesions (which are more common in the sacrum and in the entire spine than are the primary tumors), surgery is always palliative. The main goal of the palliative procedure is functional improvement, although the literature suggests that debulking of the metastatic mass can be oncologically beneficial and can provide longer survival.1 Primary malignant spinal tumors are rare conditions, and the sacrum is the most common location.2,3 The main aim of surgical treatment in these cases is to be curative. En-bloc resection of a primary malignant sacral tumor with wide oncological margins could significantly influence the biomechanics of the spinopelvic complex, which in turn can result in severe deterioration of the ambulatory status, worsening the postoperative morbidity and mortality. The procedures targeting the spinopelvic soft tissue and bony reconstruction after the resection significantly lengthen the surgery and increase the risk for intra- and postoperative complications. Due to multidisciplinary cooperation, and particularly to the development of the intensive care and to anesthesiology advancements, as well as the spinal implant technology, it is possible to perform these extensive surgeries even routinely in comprehensive oncosurgical centers, where the general medical and technical environment fosters a high level of spinal surgical experience. This chapter discusses the special considerations of spinopelvic stabilization after sacral tumor resection. The body weight from the axial skeleton is transferred to the lower limbs via the sacroiliac (SI) joints. Resection of the sacrum, involving partially or totally the uni- or bilateral SI joints, can affect the biomechanical integrity of the pelvic ring, resulting in disturbances in the physiological movement of the patient particularly in standing and walking. There is no consensus among sacral tumor experts regarding the need for stabilization and bony reconstruction after resection of a sacral tumor. Some authors reported that spinopelvic stabilization was not necessary after total sacrectomy.4,5 In their opinion, based on their clinical observations, the remaining muscles and the developing scar tissue at the site of the spinopelvic defect of the body wall can somewhat stabilize the spine as a sling during the postoperative course. Detailed analysis of functional outcomes after long-term follow-up is still unclear. In contrast, biomechanical studies and case series of patients undergoing total sacrectomy show the benefits of bony reconstruction supported by spinopelvic stabilization.6–16 In cases of total sacrectomy and in certain cases of high sacrectomy, where the cranial resection plain is above the S I/II junction uni- or bilaterally, spinopelvic stability significantly deteriorates.17–19 In cases of high sacrectomy, if the resection is done above the S1 foramina, the remaining sacral bone is potentially not strong enough to transfer the loading from the spine to the pelvic ring, yielding a higher risk of subsequent fatigue fractures of the sacral remains.18 The immediate advantage of stabilization is that it enables starting rehabilitation immediately after the surgery, starting with in-bed exercises and, a few days later, progressing to walking. The early mobilization of these patients helps prevent the postoperative complications related to long-term inactivity, such as thromboembolism, pneumonia, and pressure sores. The psychological effect of the early mobilization is also considerable. Based on these results, and also supported by our own clinical experience, spinopelvic stabilization is strongly advised after destabilizing sacrectomy surgeries. There are no gold-standard techniques for spinopelvic stabilization. In vitro studies showed the efficacy of different stabilizing (i.e., motion reducing) techniques, but there is no evidence supporting the absolute advantage of the most rigid fixation construct. It is expected that the optimal spinopelvic fixation method should be shock absorbing and a fusion promoting. There is no doubt that the developing bony fusion between the lumbar spine and the pelvic bones will provide definitive, long-term biomechanical stability. Rigid constructs with structured bone grafts seem to be effective, but there are no available studies (or radiological images published) in the literature with long-term follow-up. The total rigidity of the implant construct can absolutely ease the graft–host surface from loading, whereas a nonrigid construction can enable cyclic loading during walking, promoting the incorporation of the bone graft. At this time the optimal rigidity of the different stabilizing constructs and their effect on graft incorporation are open questions. Sagittal balance has been reported recently to be a global biomechanical factor influencing the degenerative spinal disorders as well as the progression of deformities. In the natural course of sagittal balance and in the development of imbalance, spinopelvic parameters such as pelvic tilt, sacral slope, and pelvic incidence seem to have some predictive value. Total sacrectomy and spinopelvic reconstruction influence the spinopelvic parameters per se,20 and there can be long-term consequences of the alteration of sagittal alignment, especially if an imbalanced situation is fixed by the spinopelvic instrumentation. Proper sagittal balance is also assumed to play a role in ambulatory ability and in the development of implant failures or nonunion. Spinopelvic fixation (SPF) procedures join the lumbar spine to the pelvis (Fig. 13.1). The Galveston L-rod technique with pedicle screws and iliac rods system was among the first published techniques in 1984.21 The original Galveston technique (GT) performed the SPF with the implantation of the L-rods into the iliac crests, but these directly implanted rods commonly loosened. A modified Galveston technique (mGT) was introduced in 2000 in which the rods were also fixed to iliac screws in the caudal end of the construct. This procedure has been widely used, and further biomechanical studies showed the positive effect of the use of dual iliac screws, independent of their orientation.22,23 Fig. 13.1a–f Spinopelvic fixation (SPF) methods. (a) Galveston technique (GT). (b–d) Modified Galveston technique (mGT). (e) Four-rod reconstruction (FRR). (f) Closed loop technique (CLT). The four-rod (FRR) or double-rod double iliac screw system is a further modification of the mGT.24 In this case, the additional lumbar rods increase the rigidity of the construct but can carry a higher risk of wound healing problems due to the excessive metal implants.25 The closed loop technique (CLT) for SPF was published in 2009.15 With this technique, one single U-shaped rod is used to connect all pedicle and iliac screws (bilaterally in the lower double position), providing a better load distribution along the construct (Fig. 13.2). This method applies the philosophy of nonrigid fixation to avoid the stress-shielding phenomenon and to promote the bony fusion between the lumbar vertebral body and the pelvis. By this method, safe and strong bony connections develop within the first 24 months after the surgery (Fig. 13.2g-i). Posterior pelvic ring fixation (PPRF) is an additional dimension of spinopelvic stabilization (Fig. 13.3). This method uses part of the whole construct to connect the two iliac bones with each other. One published technique is the triangular frame reconstruction (TFR), in which one horizontal rod is used to attach the L5 vertebral body to the two iliac wings and the lower part of the ilia are also connected with another horizontal rod. This technique enables good load distribution across implants, but excessive stress in the iliac bones could entail an increased risk of implant loosening and failure.13 Another technique was published by authors from Johns Hopkins Hospital (JHH) in 2005.26 In this technique, an mGT with a transiliac bar inserted through the iliac crests is completed with a horizontal pelvic fixation screw-rod implant and a horizontal femoral allograft placed between the two iliac crests. The different parts of the construct are attached with various connectors. Anterior spinal column fixation (ASCF) is the third possible dimension of spinopelvic stabilization (Fig. 13.4), which consists of adding an anterior support to the lumbar spine. Kawahara et al9 used a two vertically inserted pedicle screws attached to a sacral rod connecting the two ilia to directly connect the L5 vertebral body to the spinopelvic fixation construct. Their novel technique is a combination of SPF, ASCF, and PPRF techniques using a minimal amount of implants. Dickey et al7 reported the bilateral fibular graft (BFFR) technique, where two fibular grafts placed between the L5 vertebral body and the bilateral iliopectineal area provide a good anterior support strengthening the ASCF aspect of the construct. It can be combined with any SPF and SPF+PPRF techniques.
Spinopelvic Reconstruction/Fixation and Fusion

 Introduction
Introduction
 Biomechanical Considerations
Biomechanical Considerations
 Spinopelvic Stabilization After Total Sacrectomy
Spinopelvic Stabilization After Total Sacrectomy
Spinopelvic Reconstruction/Fixation and Fusion
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree