A Mild truncal asymmetry These mild asymmetries are variations of normal, do not require treatment, and cause no disability.
Normal Development
The axial system develops during the embryonic period.
Embryo
During the fourth week, mesenchymal cells from the sclerotome grow around the notochord to become the vertebral body and around the neural tube to form the vertebral arches [B]. Cells from adjacent sclerotomes join to form the precursor of the vertebral body, an intersegmental structure. Between these bodies, the notochord develops into the intervertebral disc. Cells surround the neural tube to become the vertebral arches.

B Sclerotome growth Cells from the sclerotome grow around the notochord and neural tube.
During the sixth fetal week, chondrification centers appear at three sites on each side of the mesenchymal vertebrae. The centrum is formed by the coalition of the two most anterior centers. Chondrification is complete before the ossification centers appear [C]. The centrum, together with an ossification center of each arch, make a total of three primary ossification centers for each vertebra.
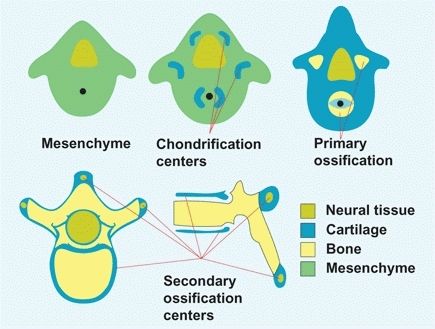
C Vertebral development Vertebrae develop first as mesenchyme, then cartilage, and finally bone. Secondary ossification centers develop during childhood and fuse during adolescence or early adult life. From Moore (1988).
Childhood
During early childhood, the centers of each vertebral arch fuse and are joined to the vertebral body by a cartilaginous neurocentral junction. This junction allows growth to accommodate the enlarging spinal cord. Fusion of the neurocentral junction usually occurs between the third and sixth years. Anterior notching of the vertebrae is sometimes seen in the infant’s or child’s vertebrae and shows the site of somite fusion [C].
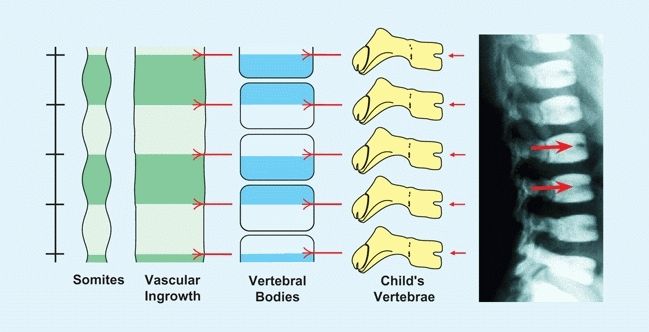
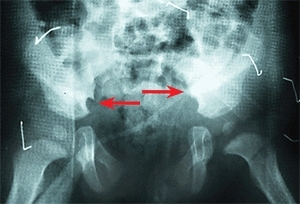
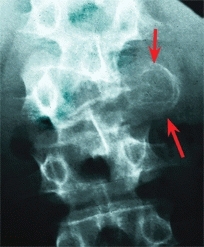
C Vertebral intersegmental development The vertebral bodies form as intersegmental structures. As blood vessels grow between somites, their final position is midvertebral. The site of blood vessel entry and somite fusion is sometimes seen radiographically as an anterior notch in the vertebral body of the child (red arrows).
Secondary ossification centers
develop at the ends of the transverse and spinous processes and around the vertebral end plates at puberty. These fuse by age 25 years. Congenital defects are common in the axial system. Variations in the lumbar spine occur in about one-third of individuals. Spina bifida occulta is common. Hemivertebrae result from a failure of formation or segmentation. Such lesions are frequently associated with genitourinary abnormalities and less frequently with cardiac, anal, and limb defects; tracheoesophageal fistula; and conductive hearing defects if the cervical spine is involved.
Cord level
Initially, the neural and bony elements of corresponding somites lie opposite each other. Thus, the caudal end of the spinal cord fills the spinal canal, and the spinal nerves pass through the corresponding intervertebral foramina. By the 24th fetal week, the cord ends at S1; at birth, at L3; and in the adult, at L1 [A]. This differential growth rate results in the formation of the caudal equina: the accumulation of the nerves traversing the subarachnoid space to the intervertebral foramina. The end of the cord is attached to the periosteum opposite the first coccygeal vertebra by the filum terminale. The filum is the residual of the embryonic spinal cord.
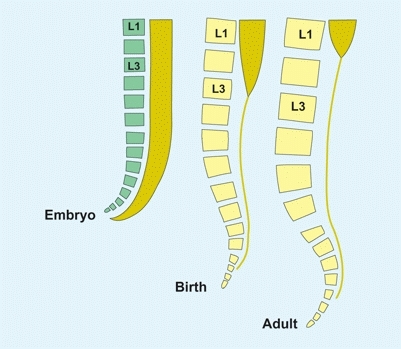
A Spinal cord vertebral column relationship During the fetal period, the spinal cord fills the vertebral canal. With growth, the cord ends at a progressively higher level.
Sagittal configuration
In the frontal projection, the spine is relatively straight throughout growth. In the lateral projection, the spine evolves from a single curve at birth to a triple curve pattern in the child [B]. Although this triple curve pattern is necessary to assume an upright posture, the obliquity imposes an added load on the lumbar spine. This load contributes to development of spondylolysis in the child, intervertebral disc herniation in the adolescent, and degenerative arthritis in the adult.
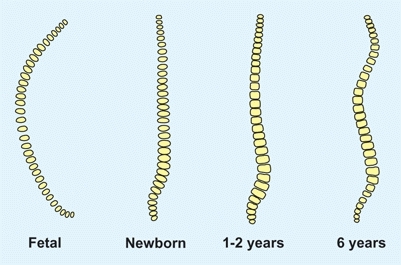
B Normal spine development (sagittal plane) The spine changes from a single curve at birth to a triple curve during childhood.
Evaluation
The spine is evaluated as part of a screening examination or to assess pain or deformity.
History and Physical Examination
Screening examination
Is there some underlying disorder? Marfan syndrome, neurofibromatosis, osteochondrodystrophies, or mucopolysaccharidoses are readily obvious in the older child but may not be so apparent in the infant.
History
Inquire about the onset, progression, disability, and duration. Family history is of great importance because scoliosis and hyperkyphosis are often familial. Back pain is also familial.
Posture
Note asymmetry of shoulder height, scapular prominence, flank crease, or asymmetry of the pelvis. Note any skin lesions, especially those in the midline. The presence of midline skin lesions, such as dimples, hemangioma or hair patches, cavus feet, or leg atrophy, are often associated with underlying spinal lesions. Café au lait spots are associated with neurofibromatosis, a cause of scoliosis.
Be aware that minor truncal asymmetries occur in about 10% of children. These are benign, cause no disability, and require no treatment. Avoid calling attention to such normal asymmetries because it only worries the patient and family.
Forward bending
Perform the forward bending test [A]. This is best done with the examiner seated in front or behind the child. Control the child’s forward bend by holding the hands together. Slowly guide the child’s forward bending while observing the symmetry of each level of the spine. Any significant scoliosis will be readily apparent.
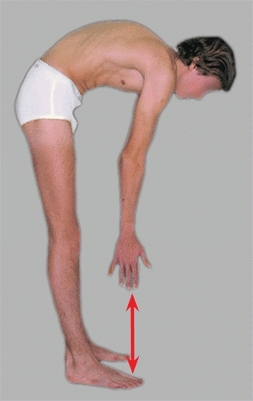
A Limited forward bending Limited forward bending (red arrow) is seen in a variety of diseases. It is an important sign that suggests the need for additional studies.
For children unable to stand, examine the child sitting with forward bending. If unable to sit, examine the child prone and look for truncal asymmetry.
Assess asymmetry with a scoliometer [B], which measures inclination. Minor degrees of asymmetry are usually only a variation of normal, but require follow-up examination. If any abnormalities are found, a detailed physical and screening neurological examination is essential to avoid diagnostic errors. Hesitation, a list to one side, or restricted motion is abnormal. Lesions such as spinal cord tumors, spondylolisthesis, disc herniations, or discitis limit the mobility or symmetry on forward bending.
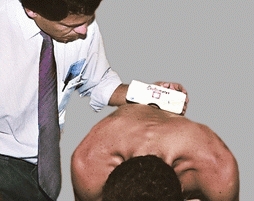
B Truncal inclination Asymmetry may be assessed with an inclinometer or scoliometer. Measures above 5°-7° are an indication for radiographic studies.
Side view
As viewed from the side, the back should curve evenly without any sharp angulation. A sharp angular segment of the spine is seen in Scheuermann kyphosis.
Neurological examination
should be part of the examination. In addition to the routine assessment, assess abdominal reflexes. Abdominal reflexes are assessed by gently stroking each quadrant of the abdominal wall [C]. Absence or marked asymmetry suggests a subtle neurological abnormality that may indicate the need for more intensive neurological investigation, such as MRI.
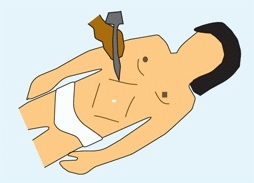
C Abdominal reflexes Stroke each quadrant of the abdomen with the base of a reflex hammer to assess the symmetry of the reflex.
Imaging Studies
Radiographs and other imaging studies are indicated to measure the vertebral curves and to further assess specific problems identified by the physical examination [D].
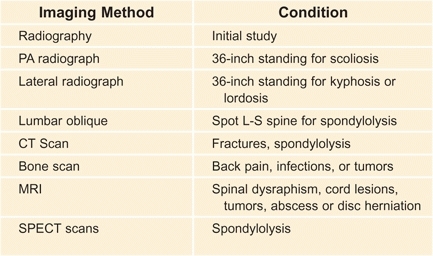
D Uses of imaging methods for spinal disorders Avoid ordering a battery of studies, as this is expensive and often exposes the child to unnecessary radiation.
Radiographs
Make PA and lateral spine films in the upright position on 36-inch film using shielding and techniques that avoid excessive radiation exposure. Order oblique lumbosacral views to assess the pars if spondylolysis is suspected and not seen on lateral view.
SPECT
Single-photon emission computed tomography (SPECT) imaging is useful to assess subtle pars reactions.
CT studies
are useful to detail bony deformities or lesions.
MR imaging
is used to study patients with neurological findings, those with unexplained progression of deformity, and certain types of deformity, as well as preoperatively for children with neurological impairment. These studies are helpful in evaluating tumors, congenital abnormalities such as Chiari malformation [C], various cysts, tethered cords, and filum terminale anomalies.
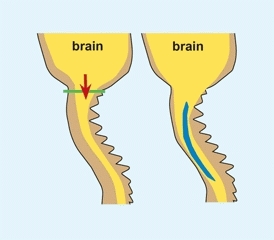
C Chiari malformation and syrinx This malformation is a displacement of the cerebellum into the spinal canal (red arrow). These lesions may be associated with a syrinx (blue).
Multiple studies
Order only those imaging studies that are definitely necessary during the initial evaluation [D].


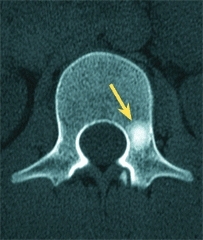
D Osteoid osteoma spine This lesion caused severe night pain. Enlargement of pedicle is seen on radiographs (red arrow). The bone scan showed a focal hot spot (orange arrow) and the CT scan shows the sclerotic lesion (yellow arrow). Excision was curative.
Normal variability
Measurements of deformity are made from standing radiographs [A]. Be aware of the normal range in the sagittal plane [B].
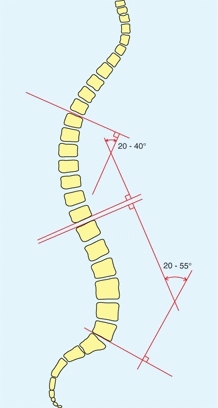
A Method of measuring spinal alignment Select the endplate of the upper and lower vertebrae with greatest deviation from the horizontal plane. Construct an endplate and right angle line (red). The enclosed angle is the degree of kyphosis or lordosis.
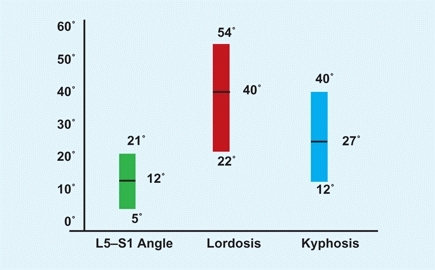
B Normal values of sagittal measures of the spine in children The range includes values from the 10th to the 90th percentiles. The L5-S1 angle includes measures between the inferior surface of L5 and the superior surface of S1 (green). Lordosis is measured using the Cobb method between L1 and L5 (red). Kyphosis is measured using the Cobb method between T5 and T12 (blue). From Propst-Proctor & Bleck. JPO 3:344, 1983.
Sagittal plane
The normal range for dorsal kyphosis falls between about 20° and 45°. Kyphosis between 45° and 55° is marginal. Kyphosis below 20° is referred to as hypokyphosis, and above 55° as hyperkyphosis. Hyperkyphosis is sometimes referred to as a “round back” deformity. Normal levels for lumbar lordosis fall between 20° and 55°. Likewise, reduced lordosis is termed hypolordosis, and increased lordosis is termed hyperlordosis. Hypolordosis is called a “flat back” and hyperlordosis either a “lordotic deformity” or a “swayback.”
Frontal plane
Mild curves that cause truncal asymmetry are usually normal variants. These variations are <10° by Cobb and <5° by scoliometer measure. These asymmetries have not been shown to cause any disability in childhood or adult life. Bone scans are usual in assessing back pain when radiographs are negative or equivocal.
Congenital Deformities
Diastematomyelia
This is a congenital defect with a central cartilaginous–bony projection that divides the spinal cord [A].



A Spinal dysraphism Diastematomyelia and other congenital spine defects should be considered in children with cavus feet or limb hypoplasia (red arrow). The interpedicular distance is widened (orange arrow) and a midline bony bar bisects the spinal cord, as shown on myelography (yellow arrow).
Diagnosis
Cutaneous lesions occur in most patients with a hairy patch, dimple, hemangioma, subcutaneous mass, or teratoma at or near the level of the diastematomyelia. Other deformities are common. Nearly all have some associated anomaly, such as spinal dysraphism, asymmetry of the lower extremities, clubfoot, or a cavus foot. Two-thirds have congenital scoliosis. Two-thirds are located in the lumbar spine. Half have neurological abnormalities.
Management
Resect the spur in a patient with progressive neurological findings. Follow the others and consider resection should neurological findings develop or if correction of spinal deformity is planned.
Sacral Agenesis
Caudal regression or sacral agenesis includes a spectrum of abnormalities [B] with hypoplasia or aplasia [C] of the sacrum, which is most common in offspring of diabetic mothers.
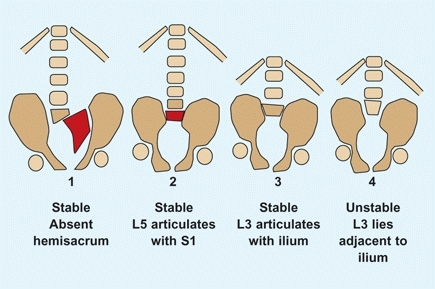
B Sacral agenesis classification by Renshaw. The sacrum may be hypoplastic or completely absent (red). The spine-pelvic relationship may be stable or unstable. Based on Renshaw (1978).
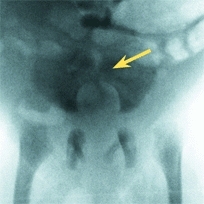
C Sacral agenesis Radiographs show a type 3 deficiency (yellow arrow).
Clinical features
include knee-flexion contractures with popliteal webbing, dislocations and flexion contractures of the hips, scoliosis, equinovarus deformities of the foot, and instability at the spinal–pelvic junction. These deformities vary in severity with the level of the agenesis and the resulting loss of motor power. Neurological features may be most predictive of progression, and MR imaging is helpful in assessment.
Management
is often difficult and depends upon the deformity, motor, and sensory status. Knee flexion deformities are difficult to correct, and recurrence is common. The combination of limited operative procedures and orthotic or mobility aids are tailored to the child. Spine–pelvic instability and hip dislocations are often better tolerated than the stiffness caused by surgical stabilization or reduction.
Exstrophy Bladder
A failure of anterior closure of the pelvis results in pelvic diastasis and an open bladder [D]. In the more severe form, cloacal exstrophy, an omphalocele containing intestinal contents, is also present.

D Bladder exstrophy This is associated with separation of the pubic bones (yellow arrow) and retroversion of the acetabula. Bilateral iliac osteotomies (red arrows) were performed to facilitate bladder reconstruction.
Clinical features
include pelvis diastasis, acetabular retroversion, and lateral rotation of limbs with out-toeing gait. This out-toeing tends to improve with age.
Management
Orthopedic disabilities are insufficient to require correction. A pelvic osteotomy may be required during bladder reconstruction to facilitate closure. Perform bilateral supra-acetabular osteotomies and stabilize with a spica cast following urological repair.
Back Pain
During the past several decades, back pain in children has become increasingly common [A]. This is especially true in adolescents and late teens. This increase is associated with increasing stress, complexities in family relationships [B], diminished physical activity, and increasing time with television and electronics. Because of the prevalence and social/cultural factors, the role of the primary care provider has increased significantly.
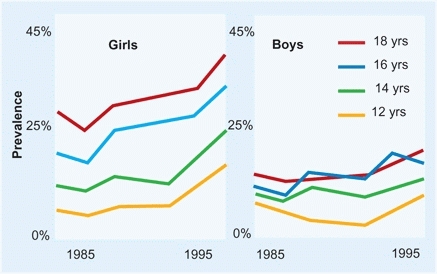
A Back Pain Children Prevalence by date, age, and gender. From Hakala et al, BMJ 325:737, 2002.
B Familial back pain The child may learn about back pain from siblings and parents.
Prevalence
Back pain has becomes increasingly common especially among girls in late teens [A].
Evaluation
Be aware of the causes of back pain [C]. Worrisome features include onset before age 4 years, symptoms persisting beyond 4 weeks, interference with function, systemic features, increasing discomfort, night pain, neurological findings, and recent onset of scoliosis.
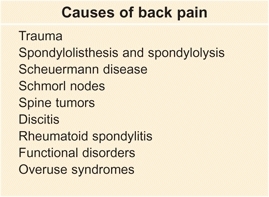
C Causes of back pain in children These are the major causes of back pain in children and adolescents.
The location is significant [D]. Thoracic back pain is more common in girls, more common in late teens, and much less likely to be serious and require treatment.
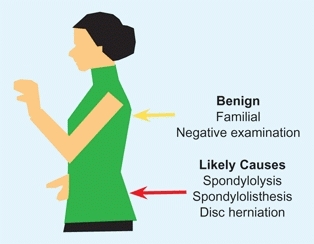
D Location and seriousness Lower back plain (red arrow) is much more likely to require treatment than upper and mid back pain (yellow arrow).
Perform a careful physical examination. On bending, look for symmetry, mobility, and evenness of the curvature. Note the location of any tenderness. Perform a neurological examination and check for tight hamstrings.
Generally, image by radiographs – anteroposterior and lateral studies – are sufficient. Be aware that oblique views and CT scans expose the child to significant amounts of radiation. Avoid ordering MRI and other expensive studies. The spine doctor will prefer to order exactly what is needed.
When to refer
Upper thoracic pain
Can often be managed in primary care.
Low back pain
Especially if associated with localized tenderness, limited spine mobility, limited straight leg raising, uneven curvature of the back when bending, or asymmetry.
Management
Adolescent benign back pain
Some suggest limiting backpacks to less than 20% of body weight (not evidence based). Encourage activity, a healthy lifestyle, and weight control. Provide reassurance. Consider this as a common backache, requiring no treatment, and best ignored.
Prognosis
If back pain is present in adolescence together with a positive family history of back pain, nearly 90% of these adolescents will have back pain in adult life. Psychosocial problems are more significant than structural abnormalities in determining the likelihood that back pain will become chronic [C].
Tumors
Tumors may be metastatic or primary. Primary tumors may arise from the cord or bone [A].
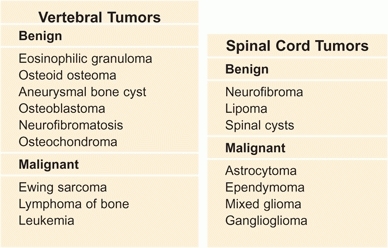
A Vertebral (bone) and spinal cord tumors
Metastatic Tumors
These tumors are most common in the thoracic, then lumbar, and least common in the cervical spine [B]. Manage with chemotherapy and radiation. Mortality is high. Those who survive are likely to have deformity. Early stabilization may prevent progression of the deformity.
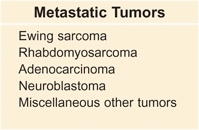
B Metastatic tumors to spine From Freiberg (1993).
Primary Tumors
Primary tumors may occur in the vertebrae or cord. Most vertebral tumors are benign, and most cord tumors are malignant. Either type may cause spinal cord compression [C].
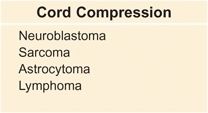
C Tumors causing cord compression in children From Conrad (1992).
Spinal cord tumors
cause diagnostic difficulties. They may present to the orthopedist with torticollis, scoliosis, gait disturbances, foot deformities, or back pain. Often forward bending is limited and asymmetrical. Perform a careful neurological examination. Study with plain radiographs first. Look for changes in intrapedicular distance. MRI studies are usually diagnostic.
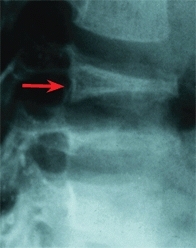
Vertebral tumors
are more common. Most are benign. Most present with pain. Duration of symptoms from benign tumors is usually longer than those from malignant tumors. Most may be diagnosed by conventional radiographs.
Osteoid osteoma and osteoblastoma
cause classic night pain, usually secondary scoliosis, limited spinal mobility [D], often tenderness, and sometimes classic radiographic features. Bone scans are often diagnostic. Excision is often necessary. Exactly localize with preoperative imaging. Percutaneous ablation is an option [E].



D List on forward bending This boy with an osteoid osteoma shows asymmetrical forward bending. Bending is restricted on the left side (arrow).



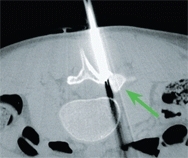
E Percutaneous ablation of osteoid osteoma The lesion is difficult to image on the radiograph (white arrow), but inflammation is readily apparent on MRI (red arrow), well defined on CT (yellow arrow), and ablated percutaneously, as shown by intraoperative imaging (green arrow).
Eosinophilic granuloma
causes pain, tenderness, limited mobility, and usually a focal lesion. The classic vertebrae plana [F] is often absent. For solitary, uncomplicated lesions, observational management is appropriate. If lesions are multiple or if neurological involvement is present, operative resection may be necessary.
F Disc collapse from eosinophilic granuloma Note the vertebral collapse. The appearance is classic.
Aneurysmal bone cysts
cause pain, rarely cord or root compression, sometimes deformity, and limited mobility. Radiographs are often diagnostic with expansion and ballooning of the cortex [G]. Management is often difficult. Manage with preoperative selective arterial embolization, intralesional excision curettage, bone grafting, and fusion of the affected area if instability is present.
G Aneurysmal bone cyst in 15-year-old boy Note the expansile cystic lesion (arrows).
Scheuermann Disease
Scheuermann disease is a familial disorder of the thoracic spine producing vertebral wedging and kyphosis greater than about 45° [A] and often causing back pain.
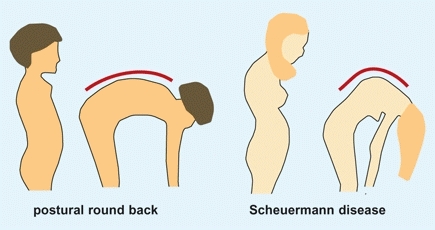
A Differentiating postural round back and Scheuermann disease Note the smooth contour of the back on forward bending in the child with round back as compared with the angular pattern in the child with Scheuermann disease.
Clinical Features
A history of heavy physical loading from athletics or work is common. Often the deformity is familial [B]. Patients often complain of deformity, fatigue, and sometimes pain. The normal even contour of the spine is lost with an abrupt kyphotic segment at or above the thoracolumbar level. Tenderness over the apex may be present. Radiographs show anterior body wedging. Mild scoliosis is common. The strict definition requires a wedging of at least 5° involving three vertebrae [C].

B Familial Scheuermann This father and son have the same fixed deformity.
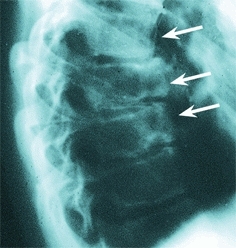
C Painful kyphosis This 16-year-old male has pain and tenderness over the lower thoracic spine. Note the narrow disc spaces, as well as erosion and deformity of the vertebral bodies (arrows).
Management
Treat the pain by NSAIDs, rest, and stress reduction. Sometimes a thoracolumbar sacral orthosis (TLSO) will be helpful in controlling the pain. Management of the deformity is discussed on page 253.
Schmorl Nodes
These nodes are vertical herniations of the intervertebral disc through the vertebral endplate, causing narrowing of the disc space [D]. Sometimes the condition is referred to as lumbar Scheuermann disease. This herniation is most common in adolescents, is often associated with trauma, and may be the cause of back pain. The lesions may be seen on plain radiographs, although MR imaging is most sensitive and may be indicated when the diagnosis is uncertain. Manage by rest, NSAIDs, and sometimes a TLSO.
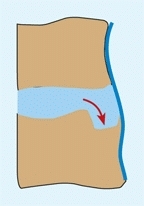


D Schmorl nodes With vertical loading, the nucleus may herniate into the vertebral body (red arrow) producing pain and atypical radiographic defects (yellow arrows).
Disc Herniation
Disc herniations occur rarely in adolescents. Predisposing features include positive family history, recent trauma, facet asymmetry, spinal stenosis, transitional vertebrae, and spondylolisthesis.
Clinical Features
Herniations usually occur at the L4–L5 or L5–S1 levels, often producing radicular pain and secondary spinal deformity. The patient may be seen because of scoliosis or a list. Straight leg raising is limited, and neurological changes are variable. Radiographs are usually normal. Occult spina bifida is more common in these patients. MRI studies or myelography shows the lesion [E]. Disability is increased if the herniation is associated with spinal stenosis. Be aware that fracture of the lumbar vertebral ring apophysis may be confused with disc herniations.
E MRI in disc herniation The posterior bulging disc at L4-L5 is clearly demonstrated on MRI.
Management
Manage first with NSAIDs, rest, limited activities, and a TLSO. Persisting or increasing disability are indications for MRI and operative disc excision. Endoscopic or open discectomies are successful in 90% of cases.
Discitis
Discitis is an inflammation (probably an infection) that involves the lower thoracic or upper lumbar disc spaces in infants and children. Unlike other musculoskeletal infections, discitis usually resolves spontaneously.
Clinical Features
The clinical features of discitis are age related. Discitis in the infant is characterized by fever, irritability, and an unwillingness to walk. The child may show constitutional illness with nausea and vomiting. The adolescent may complain of back pain. Because the symptoms are vague and poorly localized, the diagnosis is often delayed. The findings of fever and malaise, a stiff back, unwillingness to walk, and an elevated ESR and CRP are suggestive of discitis.
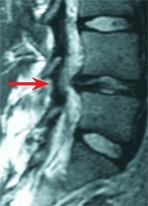
Imaging
Early in the disease, a bone scan may show increased uptake over several vertebral levels [A]. After 2–3 weeks, narrowing of the disc space is seen on a lateral radiograph of the spine. MRI often shows worrisome features and may lead to overtreatment [B].

A Discitis L4-L5 The typical features of discitis are shown on different imaging studies. The bone scan shows increased uptake (red arrow), and later the lateral radiograph shows narrowing (yellow arrow) of the disc space.
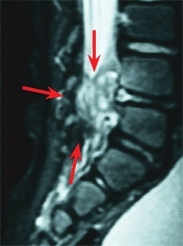
B MRI of discitis The typical intense inflammatory reaction seen on MRI may lead to concern about abscess formation and lead to unnecessary operative draining.
Aspiration or biopsy
Disc space aspiration is not necessary unless the disease is atypical.
Management
Manage based on the stage and severity of the disease. If the child is systemically ill, antistaphylococcal antibiotic treatment is appropriate. If the child is acutely ill, an intravenous route is appropriate. Otherwise, oral medication is adequate. Discitis is more severe in the older child [C]. Continue antibiotics until the ESR returns to normal. For comfort, consider immobilization in a “panty spica” or brace [D] for a period of several weeks.


C Discitis in an older child Discitis is more severe in the older child. Note the extensive inflammation of adjacent vertebrae in the MRI (yellow arrow) and the residual narrowing (red arrow).
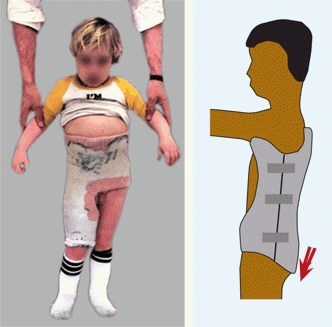
D Immobilization of the back reduces discomfort Most complete immobilization includes the back and one limb to immobilize the lumbosacral spine (left). Adequate immobilization is often achieved with a custom TLSO that extends well down over the pelvis (arrow).
Prognosis
Long-term studies show a variety of abnormalities that include residual narrowing [A, right], block vertebrae, and limited extension, but the likelihood of back pain is not increased.
Spondylolysis and Spondylolisthesis
Bilateral or unilateral defects of the pars interarticularis cause spondylolysis [A]. This defect may allow displacement of the vertebrae, which is called spondylolisthesis. These lesions are the most common cause of structural back pain in children and adolescents.
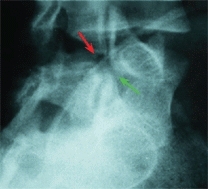

A Spondylolysis The fracture through the pars is shown by red arrows. Note the fracture through the pars as shown on the oblique radiograph (upper left) and diagram (upper right). The scotty dog analogy is often used (lower left) to describe the vertebral elements (yellow lines). The neck is the site of fracture. The superior facet of the sacrum (green arrow) normally prevents forward displacement of L5. This restraint is lost when the pars fractures. The model (lower right) shows the site of the fracture.
Pathogenesis
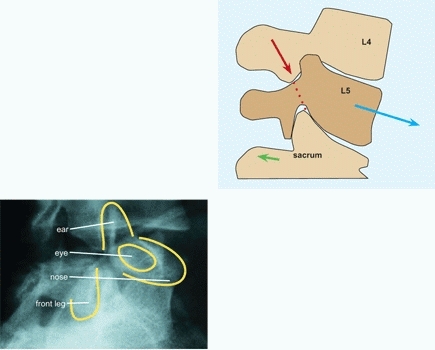
In children, these conditions are usually due to a stress fracture through a congenitally dysplastic pars interarticularis. This inherent weakness occurs more commonly in certain races (such as Inuit peoples), families, or individuals. The defects often are associated with spina bifida occulta. Spondylolisthesis occurs in about 4% of 4-year-old children and increases to about 6% by maturity. Spondylolisthesis occurs in about a third of those with pars defects, especially in those with mechanical instability. These lesions occur more commonly in children with abnormal bone or connective tissue, as occurs in conditions such as Marfan syndrome and osteopetrosis. Lesions are common in children who participate in certain sports that cause hyperextension of the lumbar spine with rotation, such as gymnastics, wrestling, diving, and weightlifting [B]. Progression after adolescence is unusual.
B The natural history of pars defects Most defects develop during early childhood and remain mild. Others develop in late childhood, usually due to repetitive trauma from certain sports or less commonly due to acute trauma.
Clinical Features
History and physical examination
The child usually complains of back pain. Tenderness may be present at the L5-S1 level. If the displacement is severe, a prominence is palpable over the defect. Straight leg raising and forward bending may be limited. The neurological examination is usually normal. If the condition is acute, secondary scoliosis may be present.
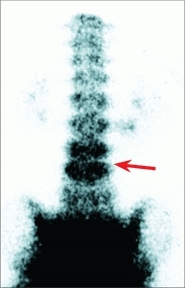
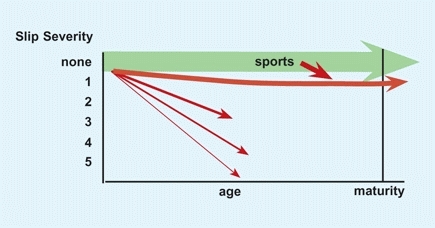
Imaging
First, order a standing lateral radiograph of the lumbosacral spine. A forward displacement of the body of L5 or L4 establishes the diagnosis. If no displacement is present, order oblique radiographs of the lower lumbar spine to assess the status of the pars. Spina bifida occulta is common in children with the defect. A bone scan may show reaction [C] before radiographs show a defect and may be used to determine the activity and healing potential of the lesion. Even more sensitive is SPECT imaging in demonstrating the stress reaction of spondylolysis.
C Unilateral spondylolysis These studies were performed in a 15-year-old girl with a history of back pain for one month. This bone scan shows an active unilateral defect (orange arrow), and the CT scan shows the defect clearly (red arrow).
Classification
Wiltse classifies spondylolisthesis into two types:
Dysplastic
is a congenital facet deficiency allowing slippage.
Isthmic
allows slippage due to a defect in the pars interarticularis. These lesions may be due to a fatigue fracture, a stress fracture, or elongation without fracture.
Grade
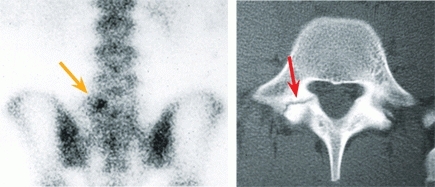
the degree of slip in severity and activity (duration).
Severity
Grade on the basis of slip angle [A, next page] and displacement [C, next page]. Slip angle changes usually occur with slips greater than 50%.
Activity
Grade on the duration or activity. Recent fractures are active and show increased uptake on bone scan. Cold lesions are chronic, inactive, and less likely to heal.
Progression
Pain is most pronounced at the time of onset or fracture. Most isthmic lesions become stable and painless with time. Pain is aggravated by activity, especially competitive sports. Lesions often are symptomatic in adolescence but become painless in adult life when activity levels are reduced. The incidence of back pain is comparable to normal population levels.
Management
Management is based on the patient’s age, degree of deformity, type of lesion, activity, and physical activity level.
Spondylolysis
management depends upon the activity of the lesion.
Acute lesions
from an acute injury or recent overuse experience are managed by reduction of activity and usually an under-arm brace [B]. Often these lesions will heal.
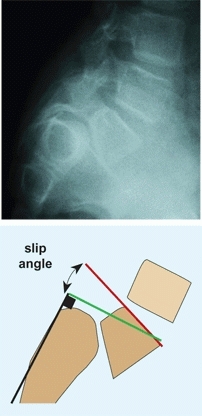
A Slip angle Draw the sacral line (black) along the posterior margin of the sacrum. Construct a right angle line to sacral line (green). Draw the L5 body line along the superior margin of the body of L5 (red line). The slip angle is the angle between the green and red lines.
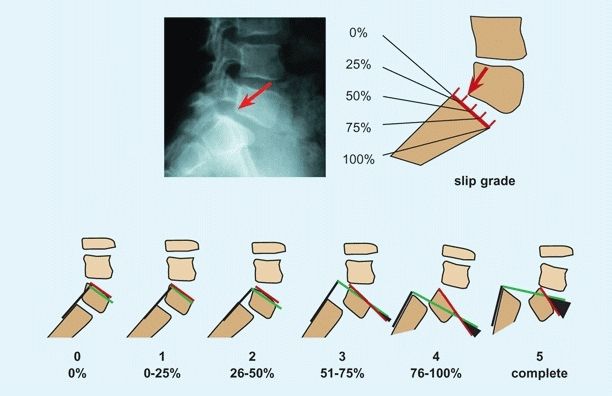
C Slip displacement The severity of the slip is assessed by the degree of displacement of L5 relative to the sacrum (red arrows) and the slip angle (black triangles). Slips are graded into five categories based on degree of displacement. Note that the slip angle increases progressively through grades 3 to 5.


B Brace for spondylolysis The brace from the front and back shows the anterior closure and posterior extension to provide optimal immobilization for an under-arm brace.
Established lesions
Manage symptoms with NSAIDS and activity modification. Operative stabilization is seldom necessary.
Spondylolisthesis
is managed based on the severity of the slip, considering the displacement and slip angle. If fusion is required, it is often performed without reduction.
Grade 1–2 slips
Manage with NSAIDS, activity modification, and TLSO as necessary to control symptoms. Follow with standing lateral radiographs.
Grade 3 slips
Most require operative stabilization in children. Fuse L4–S1 level with posterolateral autogenous grafting.
Grade 4 slips
These slips may require fusion of L4-S1, as the displacement may be significant, making identification of the transverse process of L5 difficult. If slip angle is severe, reduction is sometimes performed.
Grade 5 (spondyloptosis)
management is controversial. In situ fusion provides pain relief and safety, but the deformity remains. Reduction incurs greater risk but improves appearance and posture.
Special situations
require tailoring of management.
L4 spondylolisthesis
is less common, more mechanical in etiology, often causes more symptoms, and is more likely to require operative stabilization.
Spondylolysis
with persisting symptoms may be managed by repair of the pars defect with grafting and fixation.
Scoliosis
Scoliosis is often defined as simply a frontal plane deformity of the spine >10°. The deformity is much more complex, however, and includes significant transverse and sagittal plane components. The causes of scoliosis are numerous [A]. Mild truncal asymmetry occurs in as much as 10% of the population and may be considered as a variation of normal. Curves greater than 10° are abnormal, and in the growing child may progress to cause a significant problem. Scoliosis is the most common back deformity.
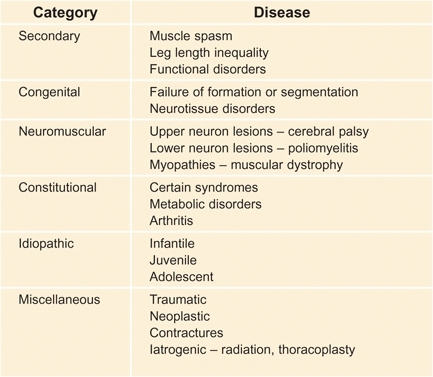
A Classification of scoliosis Scoliosis is classified into general categories.
Secondary or Functional Scoliosis
This type of scoliosis can also be described as “functional” because it is secondary to some other problem [B]. The scoliosis usually resolves when the underlying problem is corrected. The scoliosis is usually flexible and nonstructural. There are no bony changes, and the rotational elements are minimal. The common causes of functional scoliosis are leg length inequality and muscle spasm.
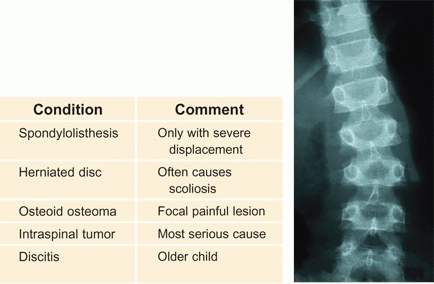
B Underlying causes of scoliosis due to muscle spasm These conditions should be ruled out if the scoliosis is atypical, associated with pain, list, stiffness, tenderness, or obvious muscle spasm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








