Cervical bracing can be categorized in several different manners. In general, these devices can be subdivided into two broad categories: cervical and cervicothoracic. Cervical devices encircle the cervical spine, whereas cervicothoracic braces extend into the thoracic spine. When adding a thoracic extension piece, the cervical orthosis (CO) provides greater motion control of the lower cervical spine. To limit extension and hyperextension of the cervical spine, an intimate fit under the occiput must be achieved.
Soft Cervical Collars
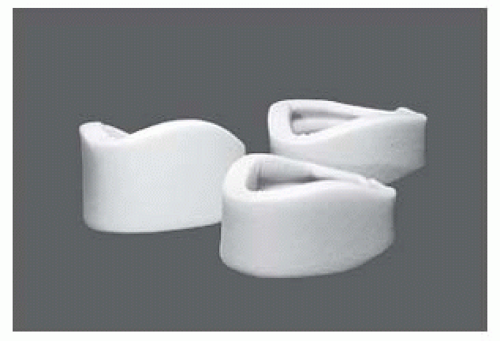
A soft cervical collar is prefabricated foam rubber with a cotton stockinette covering and Velcro closures (
Fig. 77-1). These closures are worn posteriorly. Depending on the patients dexterity and upper extremity range of motion, some can only fasten the closures anteriorly and rotate the collar around their neck while others leave the Velcro closures in the front. The manufacturer’s intention was to have these collars worn with the closures facing posteriorly. Collars range in size from small to extra large. To identify the correct size, circumferential neck measurements are taken. This measure corresponds with pre-determined sizes. Patients tolerate this device very well. Carter and associates reported that the degree of motion restriction achieved with the soft collar was dependent on the velcro closure position (
5). If the intent is to limit flexion, then the collar should be worn in the reverse position with the tabs facing anteriorly. The explanation for this is a function of the starting position of the head. Given its soft material construction, the soft collar can only provide warmth, psychological reassurance, and kinesthetic reminders to limit cervical range of motion; it cannot provide structural support. Essentially, this orthoses reminds the patient not to move. Its use may be appropriate to treat mild muscular spasms associated with arthritic changes and mild soft-tissue injuries.
Soft collars are often prescribed for the early management of whiplash injuries. The effectiveness of its therapeutic use is under scrutiny. A study evaluating whether or not a soft collar reduced the duration and intensity of the patient’s pain following a whiplash (
9) showed that test patients wearing a soft collar and control patients not wearing a soft collar reported persistent pain for at least 6 weeks postinjury. Hence, wearing a collar did influence the patients’ pain. In a randomized prospective study (
10), comparing the effect of early mobilization wearing a soft collar versus not wearing a soft collar, a significant finding was the number of days it took the group with the collar to return to work. Those who wore the collar took twice as long to return to work (mean 34 days) whereas the mobilization group without the collar returned to work sooner (mean was 17 days). In another randomized controlled study (
11), examining the effect of early mobilization versus the use of a collar in patients sustaining a whiplash injury, found that those patients who participated in early mobilization rated their pain and disability less than those wearing a soft collar at 6 weeks after injury. At 6 weeks, the exercise group rated their pain less in the neck and shoulder and had fewer headaches. The early mobilization group was seen by a physical therapist for exercise instruction. In 2006, the same group of researchers published their findings using the same cohort except the patients were 6 months out and the results were the same. Patients who engaged in physical therapy with active exercises had less pain at 6 months than those treated with a soft collar (
12). Considerations regarding the negative effects of brace wearing (i.e., psychological dependency, muscle atrophy, etc.) should be weighed under this condition.
Hard Cervical Collars
These rigid prefabricated COs are used for either prehospital trauma immobilization or long-term management in patients who sustained a cervical injury. Examples of collars used for prehospital emergency stabilization are the Philadelphia, Stifneck, Ambu, and the NecLoc. These collars are either a one- or two-piece design. Each of these devices is radiolucent and also CT
and magnetic resonance imaging (MRI) compatible. With the exception of the Philadelphia collar, these extrication collars are used for short-term use. The purpose of these prehospital collars is to aid the rescuer in maintaining spinal alignment and stabilization in patients with potential or actual cervical injuries during transport. Using six fresh cadaver geriatric spines, Bednar concluded that the Stifneck and Philadelphia collars did not provide significant mechanical immobilization in the unstable cervical spine and may be ineffective in preventing displacement (
13). This study questioned the effectiveness of these collars during field use. The results have to be considered carefully in light of the sample size and population studied. Nevertheless, the prehospital standard of care is to immobilize the cervical spine with a rigid collar with sandbags or foam blocks anchored to both sides of the head on a back board.
For long-term patient management, the Philadelphia, Miami J, Aspen, Newport, or Malibu orthoses have been used. The Newport orthoses was replaced by the Aspen collar. Each of these orthoses is available in pediatric and adult sizes. Typically, these devices are prescribed for mid-cervical bony or ligamentous injuries, postoperative stabilization, or post-halo removal. Some specific clinical conditions are anterior cervical fusion, anterior discectomy, and cervical strain. If spinal instability exists, these rigid devices are contraindicated. These appliances are being used as the first line of treatment instead of traditional halo devices for the conservative management of stable upper cervical fractures in adults (14—20). Examples of these fractures include: unilateral avulsion fracture of the transverse atlantal ligament (
20), Jefferson fracture, (burst fracture of C1) (
14,
16), Hangman’s fracture (traumatic spondylolisthesis of the axis-C2 on C3) (
15,
16,
18), isolated lateral mass fracture of the atlas (
19), and certain types of odontoid fractures (15—17). Studies analyzing patient outcomes in the aforementioned situations showed stable fracture healing, and no increased disability or neurologic compromise on follow-up examination (
14,
16,
18,
19,
20). In addition, these devices are cost-effective, easily applied, and do not have the increased risks associated with the use of the halo. Frequent diagnostic imaging to detect possible instability is strongly recommended. Each of these devices is radiolucent and CT and MRI compatible.
The Philadelphia collar is a two-piece design constructed from closed cell Plastazote foam with molded chin and occipital support. Anteriorly it extends from the mandible to the sternum and posteriorly it extends from the occiput to the upper thoracic spine. The Miami J, Newport, and Aspen collars are two-piece polyethylene shells with internal padding. The Miami J collar offers greater customization; the anterior and posterior shells permit angle adjustability around the chin and occiput allowing for individual differences in bony anatomy. The Newport collar has superior and inferior adjustable supporting tabs that distribute the load along the occiput, upper thoracic spine, sternum, and upper trapezius. Each of these collars has an anterior opening to accommodate a cricothyrotomy/tracheotomy. Given the increasing prevalence of latex sensitivity, physicians may want to consider this when prescribing COs; the Philadelphia, Miami J, Aspen, and Malibu collars are latex free.
According to Goutcher and Lochhead, some patients while wearing a hard cervical collar, Stiffneck, Philadelphia, or Miami J, exhibit a significant decrease in maximal mouth opening (
21). In their study evaluating the above listed collars, 51 male and female volunteers’ inter-incisor distance was measured with and without a collar. In an unpredictable manner, several subjects displayed a reduced inter-incisor distance that was less than or equal to 20 mm. This reduced excursion could obstruct a physician’s visualization of the glottis with a laryngoscope. For some patients, their results suggest that attempting tracheal intubation with a collar in place could be difficult. Should a patient require an emergency tracheal intubation, the authors recommend maintaining manual cervical stabilization with the removal of the anterior shell of the collar before attempting intubation.
When prescribing cervical collars with removable padding such as with the Miami J and Aspen, a second set of replacement pads should be included. The patient needs a second set to replace soiled and odorous pads, to allow moist pads to air dry after patient showering or perspiring, and when the pads show wear. Since these pads can be cleaned, it is not necessary to discard them. For specific cleaning directions, have the patient consult the manufacturer’s guide. Proper cleaning prevents skin irritation. Patients with long hair should be advised to wear their hair outside the collar to prevent irritation.
When assessing fit or proper donning of the COs, look at the patient’s face to determine if the chin is centered in the anterior piece. If the chin extends beyond the collar edge, it is too small. If the chin falls inside the collar it is too large. These visual markers indicate whether or not the device is sized or donned correctly. Patients should be familiar with proper donning and doffing procedures.
Furthermore, patients and caregivers should be educated regarding its effects on ambulation. Since the collar forces the patient to look straight ahead, patients should be warned that they will not be able to look down to see their feet or what is below them. As a result the patient must be alert to tripping hazards, that is toys on the floor, cracks in the sidewalk, pets, loose rugs, etc. Since geriatric patients are prone to tripping and falling, the physician should consider ordering the home care therapist to evaluate the home environment for potential environmental hazards and to formulate safety recommendations.
Barry and associates found that wearing a cervical collar affects the driving performance in healthy men and women (
22). In a prospective randomized study, 23 volunteers wore a Philadelphia collar while driving and the following parameters were measured: velocity, acceleration, cervical rotation, and driver’s blind spot. Their results showed that drivers were able to stop, turn, and control the vehicle but drove slower. The driver’s blind spot was larger with the collar on than without it. A larger blind spot does affect merging and lane change. Overall, the researchers found that the drivers’
exhibited greater caution. Based on their design and sample size, the authors could not conclude that wearing a collar leads to an increased incidence in motor vehicle accidents. Patients should be advised about the increased blind spot associated with wearing a collar.
Pressure ulcer formation is a potential complication of rigid collar use. Fragile or insensate skin is particularly vulnerable to ulceration. Common areas susceptible to damage are the occipital protuberance, mental protuberance of the mandible (chin), clavicles, and ears. These wounds may be the result of pressure, shear, or moisture accumulation. A poorly fitting orthotic could exert an external pressure greater than the acceptable skin pressure of 25 to 32 mm Hg; when this occurs tissue ischemia ensues, resulting in an ulcer. In addition, shearing forces can arise due to facial hair and skin sliding over the collar surface, or from positional changes. For example, when a patient moves from supine to a semi-Fowler position in preparation for getting out of bed, or if the patient slides down toward the foot of the bed, shear forces can develop. Since beards increase the shear forces, it is suggested that patients shave regularly. Since constant collar wearing increases the local skin temperature, excessive perspiration in and around the area can occur. Constant moisture macerates the skin, inducing breakdown. Jirika et al. found that patients with moist skin were four times more likely to develop skin breakdown compared to those with dry skin (
23). Provisions should be made to keep the skin clean, dry, and cool.
To assess for skin breakdown, remove the anterior shell to inspect the chin and clavicles, then refasten the straps before log rolling the patient onto his or her side. Remove the posterior portion and inspect the occipital protuberance and ear lobes. When removing or applying the collar or a portion of it, the physician must maintain proper neck alignment to prevent injuring the cervical spine. Prior to discharge, patients should be advised to contact their physician if they notice any redness or pressure sores.
Plasier et al. conducted a study to evaluate the craniofacial pressures when using different hard cervical collars: Stifneck, Philadelphia, Newport, and Miami J (
24). The study found that the Newport and Miami J collars had lower skin capillary closing pressures, and their open-cell foam material prevented moisture accumulation. In supine and upright positions, the Philadelphia collar exerted high capillary closing pressures leaving the tissues susceptible to injury. In another study, occipital pressure, skin temperature, and humidity were compared when wearing the Philadelphia and Aspen collars (
25). Measurements were taken at two separate time intervals, zero and 30 minutes. Using paired
t-tests the authors found no difference in pressure or skin temperature with the two collars. Skin humidity, however, was higher when wearing the Philadelphia collar. Skin humidity relates to perspiration and perhaps the closed cell materials used in the Philadelphia collar caused the subjects to perspire more. For patients predisposed to excessive perspiration, the materials used in the collar’s construction should be considered in order to optimize patient comfort, compliance, and minimize ulcer formation. Additional but uncommon complications associated with the use of hard collars have included marginal mandibular nerve palsy (
26), dysphagia (
27), changes in intracranial pressure (
28), reduction in tidal volume (
29), and incomplete tetraplegia (
30).