CHAPTER 43 Spinal Orthoses
INTRODUCTION
Spinal orthoses are external devices which are typically applied circumferentially about the body with the intent of altering spinal motion. Lumbar supports fashioned from tree bark have been found in pre-Columbian cliff dwellings, and the use of orthoses was described both by Hippocrates and Galen.1 Centuries later, in the United States alone, some 1.8 million people use a spinal orthosis in any given year.2
CLASSIFICATION OF ORTHOSES
In 1973, the Task Force on the Standardization of Prosthetic-Orthotic Terminology Committee proposed a systematic nomenclature in which spinal orthoses are named by the segments that are immobized by the device.3 An orthosis spanning the cervical spine is a cervical orthosis (CO). An orthosis spanning the thoracic, lumbar, and sacral spine is a thoracolumbosacral orthosis (TLSO), while an orthosis spanning the lumbar and sacral spine is a lumbosacral orthosis (LSO). This terminology is accepted by all the major professional organizations which commonly deal with the devices, including the American Academy of Orthotics and Prosthetics, the American Academy of Physical Medicine and Rehabilitation, and the American Academy of Orthopedic Surgeons. The Center for Medicare and Medicaid Services (CMS), which is the most common payer for such devices, utilizes a procedural coding system which is based upon this terminology.
BIOMECHANICS
In the upper cervical spine, the occipitoatlantal joint accounts for 20% of the total available cervical flexion and extension. The atlantoaxial joint or C1–2 accounts for 14% of the total available cervical flexion and extension and 54% of the total available cervical rotation. Motion at these joints, however, accounts for only 10% of lateral bending. The greatest cervical flexion and extension takes place at C5–6 and C6–7, whereas the greatest side bending occurs at C2–3 and C3–4 with relatively less motion occurring at the lowest cervical levels.4
The thoracic facets are angled on average only 20° from the coronal plane and are positioned obliquely to the transverse and sagittal planes. Thus, lateral bending is most freely allowed at these segments. This mechanical feature is counterbalanced in the upper thoracic spine by the presence of the rib cage. The thoracic spine has been shown to be 27% stiffer in flexion, 45% stiffer in lateral bending, and 132% stiffer in extension due to the stabilizing effect of the rib cage.5 Upper thoracic segments are most mobile in axial rotation, while lower thoracic regions, less restricted by the ribs, allow the most lateral bending, flexion, and extension.4
The lumbar facet joints, which lay nearly parallel to the sagittal plane and at a nearly transverse angle to the transverse and coronal planes, will allow full flexion and extension, but limit rotation and side bending. Due to the true axis of rotation, obliquity, and contour of joint surfaces, there is some gliding of facet surfaces and some motion in the transverse and coronal planes; however, normal lumbar motion for flexion and extension is by far greater than normal lumbar axial rotation and lateral bending.4,6
Motion control by spinal orthoses is based on the principle of a three-point pressure system. This is illustrated most readily with the flexion control TLSO Jewitt orthosis seen in Figure 43.1. The orthosis provides posteriorly directed forces originating from the sternal and suprapubic pads and an anteriorly directed force originating from the thoracolumbar pad. This configuration encourages hyperextension of the spine. Thus, a simple anterior wedge compression fracture located at the midpoint of the thoracolumbar pad would be ideally treated with this type of brace. Care must be taken when prescribing an orthoses to ensure that the site of intended action is located near the central fulcrum of the three-point system. Poorly prescribed devices can create destabilizing forces and worsen injuries.
With more complex fractures or disease, rotatory control may be required. Depending on the site of injury, the orthosis will be extended and incorporate more body surface contact area, typically in the form of a body jacket. For a T7–L3 level injury a full skin contact TLSO with a high-profile trim line extending to just below the clavicles can control rotation by acting against the opposite anterior superior iliac crest. Rotational control at L5–S1 is best achieved with a low-profile TLSO with a hip spica.7 If motion control is desired above the T7 level some authors recommend a cervical extension be added.8–10 When doubt exists about the effectiveness of a brace, flexion and extension radiographs can be taken while the patient is wearing the orthosis, keeping in mind special beam angulations may be required to avoid artifact due to the superimposition of the image of the orthosis on the image of the desired spinal segments.
CERVICAL ORTHOSES
The term ‘soft collar’ refers to a broad strip of open-cell foam, plastic, or foam rubber encased in cotton stockinet with a Velcro closure (Fig. 43.2). It is the least restrictive and most common cervical orthosis. Soft cervical collars generally provide minimal restriction in range of motion.11–13 A collar which is too large tends to force the neck into extension, potentially decreasing the size of the neural foramina. A soft collar which positions the neck into approximately 10° of flexion maximizes the size of the foramina and minimizes the potential for nerve root irritation. A soft collar with the Velcro closure placed in the front may provide increased resistance to flexion, whereas a collar with the Velcro closure placed in the back may provide increased resistance to extension.13 A soft collar can provide warmth and comfort which may reduce pain and muscle spasm. Moreover, it often acts as a reminder for a person to avoid an active range of motion which may be painful. Another CO, the Thomas collar, initially developed by Hugh Owen Thomas, a physician in the nineteenth century, is a rigid collar, originally made of sheet metal and now typically made from rigid polyethylene, which mainly acts to restrict flexion and extension up to about 75% from neutral.14 It offers little control of lateral bending or rotation due to its lack of head and thorax contact.
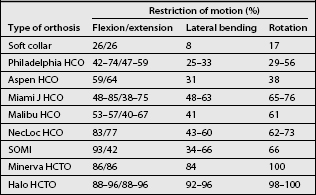
The Philadelphia, Miami J, Aspen, Malibu, NecLoc, and Stiffneck collars are also hard collars made of different materials with different types of linings. However, unlike the COs described above, these orthoses incorporate the mandible and the occiput in their design and can be classified as head cervical orthoses or HCOs. They provide head support and partially restrict motion of cervical spine in all planes, especially in the sagittal plane (Table 43.1). The Philadelphia HCO, which consists of two pieces of closed-cell polyethylene foam attached with Velcro closures (Fig. 43.3), is prototypical of the wide variety of HCOs which are produced in a multitude of sizes and shapes by different manufacturers. The Philadelphia HCO, like other prefabricated HCOs, is available in multiple configurations to accommodate a variety of clinical needs and neck shapes, including a snugly fitting version which can be used to control hypertrophic scarring.22 The Miami J and the Aspen HCOs consist of a two-piece semirigid plastic supporting structure with removable open cell foam liners. This design is often better tolerated than the solid orthoses made of closed-cell foam. In many instances, persons who require a HCO for an extended period of time will have a solid closed-cell foam orthosis, such as the Philadelphia collar, for showering and a HCO constructed like the Miami J or Aspen for everyday use. With regards to effectiveness in restriction of motion, numerous studies have been performed comparing the different types of HCOs. The results vary by study methodology, often with conflicting results.23,24
Cervical orthoses that include rigid vertical posts are cooler than hard collars, due to the lack of total skin contact, and are more stabilizing as they incorporate an additional inferior portion which is supported on the upper thorax. They are classified as head cervical thoracic orthoses or HCTOs. These orthoses may include two, three or four posts (Fig. 43.4). A prototypical HCTO is the three-posted sternal occipital mandibular immobilizer (SOMI) (Fig. 43.5). Because of its points of attachment, as described in its name, the SOMI greatly restricts cervical flexion, particularly lower cervical segments; however, because of a swivel-type occipital pad, it allows some extension.11 Lateral bending is also less restricted than flexion.
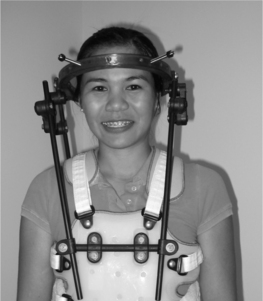
Maximal cervical immobilization is achieved with either a halo vest orthosis (Fig. 43.6) or a Minerva orthosis (Fig. 43.7). Both devices are HCTOs. A halo vest consists of a metal ring which is fixed to the outer table of the skull by four screws, a plastic chest jacket, and superstructure of bars and connectors which connect the ring to the jacket. The jacket is usually lined with sheepskin to improve pressure distribution and comfort. Due to the fixation of the halo ring to the skull, a halo vest has optimal rotational motion control. As a result, it is commonly used to immobilize the upper cervical segments, which, as described earlier, are the segments responsible for the majority of rotation of the cervical spine. However, because of its lack of total contact over the neck, intersegmental snaking of vertebral segments has been reported to occur.25,26 A Minerva HCTO, which has greater skin contact, may provide better control of this intersegmental motion and this may be a better option if this is a major concern.27 The Minerva orthoses may be prefabricated or custom made. The posterior section has a padded band that extends forward to encircle both the mandible and the forehead, thus creating a longer lever arm for cervical control.28 Its name derives from the mythological daughter of Zeus, a warrior who radiated thunderbolts from her forehead. One disadvantage of the halo device as compared to the Minerva orthosis is that it significantly changes the center of gravity of the wearer, potentially leading to balance difficulties and falls.29 Another disadvantage is the requirement of the halo to have pins seated into the skull which presents a risk for both infection and slippage.
THORACOLUMBOSACRAL ORTHOSES
The effects of a TLSO on the restriction of spinal motion, intra-abdominal pressure, intradiscal pressure, and muscle activity have all been studied, with conflicting results.30–32 No study has yet shown even near complete elimination of either segmental or gross spinal mobility by any orthosis. In one study of subjects without spinal abnormalities, who were custom fitted with a lumbosacral corset, chairback orthosis, or molded plastic TLSO, it was found that all three restricted gross body motion.31 Approximately two-thirds to one-half of orthotic free gross body motion was observed.31 When a mean percentage of restriction of all directional movement was calculated, the TLSO was found to be twice as effective as the corset, while the chairback brace was of intermediate effectiveness. The spinal motion controlled by wearing a TLSO is greatest at the upper and midlumbar segments. In contrast, motion controlled at the L4–S1 levels by wearing a TLSO is only minimal: an 8–12% reduction, or even an increase, as compared to spinal motion without a TLSO in place.30,33
Although increased intra-abdominal pressure is associated with increased lumbar spinal stability and decreased spinal load, the effect of a TLSO on abdominal muscle activity and abdominal pressure is controversial.32–36 Nevertheless, the available evidence seems to support that intra-abdominal pressure plays a role in the stabilization of the lumbar spine by a TLSO.
The effect of a TLSO or LSO on intradiscal pressure is also uncertain. Nachemson showed intradiscal pressure decreased by about 25% when subjects wore an inflatable lumbar corset.37 However, when he studied several other lumbar orthoses, an inconsistent effect on intradiscal pressure was found.38 Rohlmann studied several different lumbar orthoses regarding the effect on the load on an internal spinal fixation device, and did not find any reduction of the load by any of the orthoses.39 Since intradiscal pressure is increased with spinal flexion and decreased with the extension, a TLSO may indirectly reduce intradiscal pressures by restricting flexion.
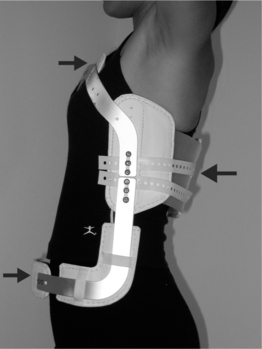
If the principal objective of a prescribed orthosis is to limit flexion and extension of the thoracic spine, and there is not a strong need for rotational control, a simple flexion control orthosis is a good option. There are two principal types of flexion control TLSOs: the cruciform anterior spinal hyperextension (CASH) brace and the Jewitt orthosis (see Fig. 43.1 and 43.8). The basic biomechanical principles underlying these orthoses is a three-point fixation.. Such orthoses are commonly made of flat aluminum bars with a vinyl-covered foam pad attached posteriorly over the midspine and two other vinyl-covered foam pads attached anteriorly over the sternum and pubis. The Jewitt orthosis is most effective for simple compression fractures or thoracic sprains between T7 and L1. It should be avoided for fractures or thoracic sprains above T6 as the sternal pad can act as fulcrum and actually worsen the condition.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree