Soft Tissue Interposition Flaps in the Management of Heterotopic Ossification and Proximal Radioulnar Synostosis
Douglas P. Hanel
Seth D. Dodds
Indications/Contraindications
Heterotopic ossification of the elbow with loss of motion can be severely debilitating. The functional arc of elbow motion spans from 30 to 130 degrees of flexion and from 50 degrees of pronation to 50 degrees of supination. Limitations to this functional arc significantly impair the ability to perform activities of daily living. Cases of elbow ankylosis or radioulnar synostosis further minimize use of the affected extremity. Once heterotopic ossification has developed and constricts motion, it is nearly impossible to regain the lost motion with conservative measures, such as physical therapy, dynamic splinting, radiation therapy, or medication.
Surgical resection of heterotopic bone about the elbow should be considered in patients who present with an unacceptable loss of flexion/extension or pronation/supination. Excision is also warranted in cases of neurovascular impingement caused by ectopic bone. In cases of proximal radioulnar synostosis or even radial head excision, interposition materials can be used to cover exposed bone surfaces.
While options for soft tissue interposition include silicone sheeting, fat graft, and free adipofascial flaps, pedicled myofascial flaps and allograft fascia lata have become increasingly popular. The pedicled anconeus myofascial flap is an ideal choice in those cases approached posterolaterally, whereas the pedicled brachioradialis muscle flap passed through the interosseous membrane is best suited for those cases approached from an anterior exposure. The soft tissue interposition acts as a barrier to the formation of recurrent heterotopic calcification and allegedly decreases pain with pronation and supination. It is suggested, though unproven, that pedicled graft tissue has greater potential
for sustained viability when judged against nonvascularized tissue transfers, such as subcutaneous fat or an adipose fascial graft. When properly fixed to the underlying bone, these pedicled flaps can sustain aggressive postoperative range-of-motion exercises that might dislodge less robust tissue such as fat alone or adipose-fascial grafts. We prefer the anconeus muscle pedicle flap when available and tensor fascia lata allograft when the anconeus is not available or not large enough.
for sustained viability when judged against nonvascularized tissue transfers, such as subcutaneous fat or an adipose fascial graft. When properly fixed to the underlying bone, these pedicled flaps can sustain aggressive postoperative range-of-motion exercises that might dislodge less robust tissue such as fat alone or adipose-fascial grafts. We prefer the anconeus muscle pedicle flap when available and tensor fascia lata allograft when the anconeus is not available or not large enough.
Historically, contraindications to excision of heterotopic bone with or without soft tissue interposition flaps included immature ossification and an unreliable soft tissue envelope. In the past decade there have been a number of reports documenting the efficacy of early excision of heterotopic bone. It is our experience that patients suffer less soft tissue contracture and have superior function with early release of a stiff elbow. The recurrence of heterotopic bone in the posttraumatic setting has not been shown to be predicated on the timing of the excision. Outcomes of surgical excision, however, will be threatened by a poor soft tissue envelope. Once the posttraumatic or post-burn wounds have healed, soft tissue swelling has abated, and nerve recovery has plateaued, patients may safely undergo elbow contracture release.
Contraindications to pedicled soft tissue interposition flaps depend on the specific muscle selected. For an anconeus muscle interposition, previous traumatic or surgical disruption of its primary vascular supply (the medial collateral artery from the profunda brachii) jeopardizes the viability of the raised muscle flap. The brachioradialis “wrap around” flap should not be raised if there is a nonfunctioning biceps brachii or brachialis, as the brachioradialis provides assistance with elbow flexion as well as supination when the forearm is fully pronated. Assuming that the arm and forearm musculature is intact, using the anconeus or brachioradialis as a pedicled interposition flap causes little functional loss.
Preoperative Planning
Before operative release and soft tissue interposition, patients must be carefully evaluated. The history should focus on the primary complaint. Patients must verbalize appropriate frustration with their disability from elbow stiffness to warrant release. It is also imperative that patients demonstrate the willingness and capacity for intensive rehabilitation. If the presenting complaint is predominantly pain, then contracture release will be futile. A focused surgical history needs to be elicited. Previous injuries and surgeries of the involved extremity offer critical information about the status of osseous and cartilaginous structures as well as the elbow’s soft tissue envelope. Operative reports from previous surgeries help understand the integrity and location of possibly transposed neurovascular structures.
Elbow range of motion, stability, pain, and functional ability are assessed. The Mayo Elbow Performance Score serves as a summary of these findings. In addition, the examination includes assessment of forearm rotation and wrist and hand function. If there is physical evidence of nerve dysfunction, electrodiagnostic studies should be obtained to confirm the location of compression and to act as a baseline of nerve function. All of our patients have had previous surgeries, and as such, a careful assessment of incisions about the elbow with regard to the palpable and radiographic location of heterotopic ossification is essential. The integrity of the skin and subcutaneous tissues should be evaluated. Lingering soft tissue swelling, edema, or erythema may all point to additional diagnoses to be contended with before deciding on heterotopic bone excision.
Standard radiographs of the elbow are obtained with oblique views to improve visualization of ectopic ossification. We routinely perform computed tomography (CT) on cases of elbow heterotopic ossification where the congruity of the articular surface is in question and in all cases with proximal radioulnar synostosis. An axial CT scan with coronal and sagittal reformatted images is currently the most helpful method to visualize the location and extent of a bony bridge between the radius and ulna (Figs. 13-1 and 13-2). Vascular study of the elbow and proximal forearm should be considered if there are concerns about the integrity of the regional blood supply, especially in cases of pedicled soft tissue interposition. Unless there are specific historical or physical findings suggesting potential or indolent infection, we limit blood studies to those required for a prolonged general anesthetic.
The timing for intervention is somewhat nebulous and is certainly directed by physician bias. We do not believe there is sufficient scientific evidence to suggest that nuclear medicine scans or blood alkaline phosphatase levels are beneficial in the assessment or timing of surgical intervention. In reviewing the literature and comparing our experience, it would appear that waiting for fracture healing
and ectopic bone maturation, defined as well-delineated borders, is the most commonly used parameters. This would suggest that operative intervention be carried out 4 to 12 months after injury.
and ectopic bone maturation, defined as well-delineated borders, is the most commonly used parameters. This would suggest that operative intervention be carried out 4 to 12 months after injury.
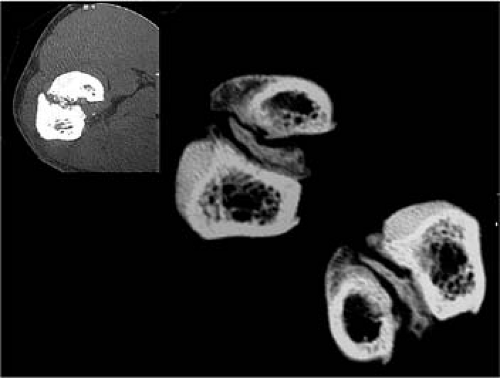 FIGURE 13-2 Coronal CT image reveals the extent of heterotopic bone involvement in the region of the bicipital tuberosity. |
Excision of heterotopic ossification and soft tissue flap interposition does not require a great deal of special equipment. We have listed a few items that facilitate operative intervention and postoperative rehabilitation in Table 13-1. In addition to the tools listed in the table, we have the following items readily available: a hinged fixator, radial head prosthetics, allograft tendon for ligament reconstruction, allograft fascia lata if local interposition material is not available, and a total elbow arthroplasty set when all else fails and the patient is the appropriate age.
Surgery
Patient Positioning
Operative approach and patient positioning are determined by previous incisions, location of heterotopic bone or synostosis, and shoulder mobility. While many surgeons prefer to operate on the elbow with the affected extremity positioned across the patient’s supine chest, we prefer to position
the patient with the affected extremity abducted onto a radiolucent table. The extremity is draped free up to the clavicle. If the shoulder is mobile, external rotation will present the medial and anterior aspects of the elbow while internal rotation presents the lateral and posterior elbow. The flexibility to effortlessly alternate between lateral and medial approaches facilitates complete excision of heterotopic bone about the elbow.
the patient with the affected extremity abducted onto a radiolucent table. The extremity is draped free up to the clavicle. If the shoulder is mobile, external rotation will present the medial and anterior aspects of the elbow while internal rotation presents the lateral and posterior elbow. The flexibility to effortlessly alternate between lateral and medial approaches facilitates complete excision of heterotopic bone about the elbow.
Table 13-1. Soft Tissue Interposition Flaps for Elbow Heterotopic Ossification: Operative Equipment | ||||
|---|---|---|---|---|
|
Technique
Exposure
We do not use tourniquets for these cases. They are a detriment to tissue mobilization, mask small arterial bleeding, and lead to venous engorgement during prolonged cases. The initial increase in bleeding at the time of incision is mitigated by injecting the proposed incision with 0.25% bupivacaine and 1/200,000 dilute epinephrine solution. The incision is delayed 7 to 10 minutes to allow the epinephrine to affect local capillaries.
It is our preference to use a posterior skin incision for elbow release surgery. This window allows a “global” approach to the elbow and can be used to access the medial, lateral, and anterior sides of the joint. The skin incision is typically straight, passing 2 cm medial or lateral to the tip of the olecranon, but may be curvilinear to incorporate previously placed posteromedial or posterolateral surgical scars. Depending on the required heterotopic bone excision or hardware removal, the incision may extend from the proximal arm to the distal forearm. This dissection avoids injury to both the medial and the lateral brachial cutaneous nerves, preserving sensibility to the proximal forearm.
When employing this approach, it is critical to create thick soft tissue flaps. The skin incision is carried down to and includes the triceps fascia proximally and the extensor fascia of the forearm distally. This effectively creates robust fasciocutaneous flaps that can be elevated circumferentially about the elbow. The extent of elevation is dictated by the location of the joint involvement. If there is medial joint involvement, as determined by CT scan, or ulnar nerve symptoms, we address these first. If there is no involvement we go directly to the lateral elbow and proximal forearm. The dissection is carried to the medial intermuscular septum, and the ulnar nerve is identified as it passes from the anterior to the posterior compartment approximately 8 to 10 cm proximal to the medial epicondyle. Even if the ulnar nerve has been “transposed anteriorly” in previous procedures, we believe that it is critical to identify the entire medial intermuscular septum, and follow it to the humerus (Fig. 13-3). In cases in which the medial intermuscular septum has been excised in part or in whole, the dissection follows the medial border of the triceps until the humerus is encountered. When the ulnar nerve is found, it should be mobilized from the cubital tunnel, preferably with a small cuff of medial triceps to protect the nerve’s vascular supply. The nerve is followed into the forearm until disappeared deeply between the heads of the flexor carpi ulnaris. Any tight scar or fascial bands crossing the nerve in this dissection are divided. The medial intermuscular septum is removed in its entirety. By following the ulnar nerve proximally in the arm, the median nerve and its accompanying brachial artery can be located along the anterior margin of the intermuscular septum. Alternatively, in arms that are not densely scarred the median nerve and brachial artery can be identified in the distal arm superior to the leading edge of the pronator teres origin as it runs medial to the substance of the biceps and brachialis muscles and just beneath the fibers of the bicipital aponeurosis. Excision of heterotopic bone involving the medial posterior and anterior elbow joint is conducted and described in greater detail in the next section.
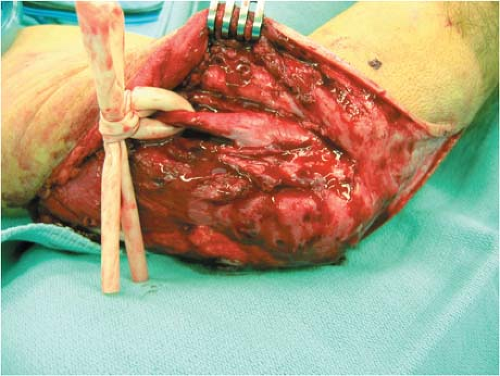
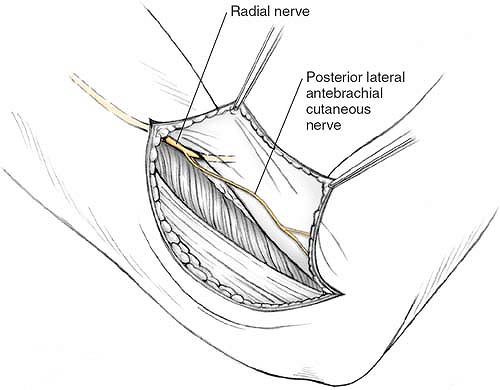
Next, the lateral side of the elbow and involvement of the proximal forearm are addressed. In cases of anterolateral heterotopic ossification, the radial nerve is identified at mid-arm and followed distally. This is done by elevating the lateral flap in the same tissue plane as the medial dissection, between the muscular investing fascia and the muscle belly of the triceps. When the lateral intermuscular septum is encountered, the radial nerve should be identified and protected. Identifying the radial nerve in a scarred bed can be daunting. We therefore use the following strategies. First, inspect the undersurface of the flap; frequently the posterior antebrachial cutaneous branches of the radial nerve to arm and forearm are visible. These branches can be followed proximally into the lateral intermuscular septum where they are found to take off from the radial nerve proper (Fig. 13-4). If this landmark is not readily available, our second approach is to dissect the distal portion of the flap toward the lateral epicondyle. On reaching the lateral intermuscular septum, the dissection is directed cephalad. The triceps muscle belly is freed from the posterior aspect of the intermuscular septum. Small vessels and nerves seen entering the triceps muscle should be followed proximally; they will lead to the radial nerve proper. If these markers fail to lead to the nerve, cautiously proceed along the posterior intermuscular septum. Somewhere between 6 and 10 cm proximal to the tip of
the lateral epicondyle, the nerve will be encountered passing along the spiral groove to pass through the lateral intermuscular septum to enter the anterior aspect of the arm. Once the radial nerve is identified, the lateral intermuscular septum is removed and the nerve followed distally. At the level of the elbow, the nerve is easily followed into the internervous plane between the proximal aspect of the brachioradialis and the distal aspect of the brachialis. Simple blunt dissection between these two muscles just superior to the joint line will reveal the radial nerve before it dives under the supinator more distally.
the lateral epicondyle, the nerve will be encountered passing along the spiral groove to pass through the lateral intermuscular septum to enter the anterior aspect of the arm. Once the radial nerve is identified, the lateral intermuscular septum is removed and the nerve followed distally. At the level of the elbow, the nerve is easily followed into the internervous plane between the proximal aspect of the brachioradialis and the distal aspect of the brachialis. Simple blunt dissection between these two muscles just superior to the joint line will reveal the radial nerve before it dives under the supinator more distally.
Excision of Heterotopic Bone
The excision of heterotopic bone and the scarred joint capsule follows. Anterior heterotopic bone frequently resides in the distal aspect of the brachialis muscle. It can extend medially and laterally encasing the collateral ligaments or even neighboring neurovascular structures. If a medial approach is chosen, entrance to the joint capsule and distal aspect of the brachialis can be achieved by exploiting the internervous plane between the ulnar innervated
flexor carpi ulnaris and the median innervated palmaris longus, flexor carpi radialis, and pronator teres. Alternatively, the flexor-pronator muscle mass can be sharply elevated off the medial epicondyle, carefully preserving the underlying anterior band of the medial collateral ligament. In severely contracted elbows, this exposure affords uncompromised visualization of the anterior capsule and crossing neurovascular bundle. This elevated myofascial flap can be reattached to the medial epicondyle with multiple suture anchors or sutured down to the epicondyle through bone tunnels. If the flexor-pronator mass is released, consideration can be given to submuscular transposition of the ulnar nerve.
flexor carpi ulnaris and the median innervated palmaris longus, flexor carpi radialis, and pronator teres. Alternatively, the flexor-pronator muscle mass can be sharply elevated off the medial epicondyle, carefully preserving the underlying anterior band of the medial collateral ligament. In severely contracted elbows, this exposure affords uncompromised visualization of the anterior capsule and crossing neurovascular bundle. This elevated myofascial flap can be reattached to the medial epicondyle with multiple suture anchors or sutured down to the epicondyle through bone tunnels. If the flexor-pronator mass is released, consideration can be given to submuscular transposition of the ulnar nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree