Soft Tissue and Bony Impingement
James Stone
SOFT TISSUE ANKLE IMPINGEMENT
Until 1950 the concept that abnormal soft tissue within the ankle joint could be responsible for pain and mechanical symptoms was not the subject of orthopedic investigation. In 1950, Wolin and associates published a paper on soft tissue impingement lesions of the ankle joint, which they termed “meniscoid” lesions because of their tactile resemblance to knee meniscus tissue (1). They reported on nine patients with chronic ankle pain after inversion ankle sprains, who were found at open surgery to have impingement lesions in the lateral gutter and improved after removal of the abnormal soft tissue. Although patients often complained of instability, they did not demonstrate objective signs of joint laxity, and their instability symptoms resolved after excision of the synovial-based lesion. The authors proposed that the inciting factor was the inversion injury that caused tissue disruption and bleeding. Although most patients gradually resolve such injuries, the ones who develop synovial impingement lesions develop a chronic synovitis with gradual thickening and fibrosis of the material in the anterolateral gutter of the ankle joint. Japanese investigators performed some of the earliest arthroscopic evaluations of the ankle joint and may have been the first to describe similar lesions on arthroscopic examination.
In 1987, McCarroll et al. (2) reported on four soccer players who developed chronic ankle symptoms after recurrent ankle sprains and did not improve with nonoperative treatment. Arthroscopic examination revealed abnormal fibrous tissue bands in each patient, and after resection of the lesions and appropriate rehabilitation, each patient returned to competitive soccer. Martin et al. (3) reported on 16 patients undergoing ankle arthroscopy for chronic ankle pain mainly after inversion sprains and found that all patients demonstrated hypertrophic synovial tissue at arthroscopy, and good or excellent results were noted in 75% of the patients after excision. Ferkel and Fischer (4) reported on 100 ankle patients who underwent ankle arthroscopy, 24 of whom had chronic anterolateral impingement symptoms. Pain and instability were common symptoms, but stress radiographs failed to document objective ligament laxity. Plain radiographs were not helpful in predicting these synovial lesions, but the authors suggested that MRI could be useful in delineating abnormal anterolateral soft tissues. In a followup study, Ferkel et al. (5) reported on 31 patients with chronic anterolateral ankle joint pain following inversion ankle sprain. None had objective evidence of joint laxity and the preoperative MRI scan was found to reliably show abnormal soft tissue synovial thickening in the anterolateral gutter. At the time of arthroscopy these patients were noted to have “proliferative synovitis and fibrotic scar tissue,” sometimes associated with adjacent chondromalacia of the talar articular cartilage. There were good or excellent results in 26 of the patients after arthroscopic excision of the abnormal tissue. Numerous other studies in the orthopedic literature support the utility of arthroscopy for resection of soft tissue impingement lesions of the ankle joint with good results in patients who do not have associated degenerative changes in the joint (6, 7, 8, 9, 10 and 11).
Bassett (12) has delineated a specific type of anterior ankle soft tissue impingement caused by mechanical impingement of the distal fascicle of the anterior inferior tibio fibular ligament on the adjacent talus. The anatomy and clinical relevance of the syndrome have been explored by others (13)
We generally refer to these problems as posttraumatic synovial impingement lesions rather than meniscoid lesions because there is a wide range of lesions varying in organization or “hyalinization” from a localized inflammatory synovitis to a well-organized mass of firm tissue. In addition, we have recognized that impingement lesions can occur in any part of the ankle including the lateral gutter, medial gutter, anterior joint, or posterior joint.
History
Patients with soft tissue ankle impingement present to the physician with persistent ankle symptoms after ankle ligament injury that fail to resolve with standard treatment of the ankle sprain. When evaluated soon after an ankle sprain, conservative measures including rest, ice,
elevation, compression, nonsteroidal anti-inflammatory medications, and a limited period of nonweight bearing immobilization in a removable orthosis may be instituted. Most patients will recover with a physician-directed rehabilitation protocol emphasizing range of motion exercises, strengthening exercises, and gradual return to weightbearing functional activities. However, other patients with more severe injuries or those who participate in high demand work or sports activities may benefit from a supervised exercise and rehabilitation program under the direction of a physical therapist.
elevation, compression, nonsteroidal anti-inflammatory medications, and a limited period of nonweight bearing immobilization in a removable orthosis may be instituted. Most patients will recover with a physician-directed rehabilitation protocol emphasizing range of motion exercises, strengthening exercises, and gradual return to weightbearing functional activities. However, other patients with more severe injuries or those who participate in high demand work or sports activities may benefit from a supervised exercise and rehabilitation program under the direction of a physical therapist.
A small group of these patients may present to the orthopedic surgeon with persistent symptoms of pain, catching, or giving way of the ankle despite a reasonable period of rehabilitation of up to 12 weeks. In general the pain symptoms are well localized either medially or laterally but may be more diffuse anteriorly and on occasion may occur posteriorly. Persistent or intermittent swelling associated with attempts to resume activities may occur.
Physical Examination
The physical examination of the patient with soft tissue impingement of the ankle joint is not specific. The clinician should first observe the ankle for signs of localized or generalized swelling or ecchymosis, which may direct the examination to a specific anatomic location. The range of motion of the ankle and the subtalar joints should be assessed and compared with the opposite ankle to detect subtle or obvious limitations. It is very important to assess the hindfoot alignment for fixed valgus or varus deformities as the presence of alignment abnormality may predispose the patient to recurrent injury and may influence the nature of the nonoperative intervention, for example using orthotic devices, or of the surgical procedures to be considered should nonoperative treatment fail to alleviate symptoms.
The examiner then assesses for specific areas of tenderness and correlates those areas with the area where the patient complains of pain. Specific examination must attempt to determine whether the tenderness is, for example, over the joint line and therefore potentially associated with soft tissue impingement versus tenderness localized to the bony structures of the ankle or possibly abnormal bony structures such as osteophytes. Soft tissue impingement lesions may be associated with palpable soft tissue prominence and perhaps palpable clipping or snapping beneath the examining finger with passive or active motion of the joint.
Much of the physical examination is dedicated to other structures to exclude other diagnoses from the differential diagnosis list. In particular, the examiner should assess the tendons about the anterior ankle to be certain that there is no evidence of chronic tendinitis or tendon tearing. For patients complaining of posterior ankle pain, the examiner must carefully palpate and assess the strength of the posterior tibial tendon, flexor digitorum tendon, flexor hallucis longus tendon, the peroneal tendons, along with the Achilles tendon. The examination of these tendons should include palpation to assess tenderness and palpation during active and passive motion of the isolated tendons to assess for crepitus, snapping, or weakness.
The neurovascular structures must also be assessed carefully. Pulses should be assessed along with a careful sensory and motor examination of the ankle and foot.
Radiographic Studies
Patients presenting to the orthopedic surgeon with ankle pain should have routine anteroposterior (AP), lateral, and mortise views of the ankle. In addition, patients with potential foot complaints should have weight-bearing AP, lateral, and oblique radiographs of the foot. Standing radiographs of the ankle may assist in assessing the degree of degenerative changes in the ankle joint and in assessing the alignment of the hindfoot joints.
A CT of the ankle and subtalar joints can be useful for assessing the bony characteristics of osteochondral lesions of the talar dome or bony osteophytes. However, this study will not contribute to the workup of soft tissue abnormalities.
Early studies of the use of MRI to assess for soft tissue impingement lesions of the ankle gave equivocal or contradictory results regarding sensitivity, specificity, and diagnostic accuracy (14, 15). The more recent orthopedic and radiologic literature has suggested that with improved equipment and image quality along with increased awareness of these lesions, the MRI is able to diagnose these lesions with a high level of accuracy (16, 17 and 18). It is also the most appropriate study to assess other soft tissue causes of ankle pain such as tendinitis or tendon tearing. In addition, the MRI visualizes bone to assess for chondral or osteochondral abnormalities in the bones comprising the ankle and subtalar joints, and the presence of bone edema in an area of the talus or tibia may be the only radiographic manifestation of injury, for example, owing to posterior impingement.
Treatment of Soft Tissue Impingement Lesions
Most patients with an acute ankle sprain will recover uneventfully from their injury with standard nonoperative treatment. In some patients there may be a propensity to develop excessive scar tissue after injury, or in the case of recurrent injury the ankle is never given adequate opportunity to complete the healing sequence with gradual resorption of inflammatory tissue associated with the healing ligament injury.
An adequate period of nonoperative treatment of up to 12 weeks should be pursued. During this time, the conservative measures mentioned above will usually decrease pain and swelling and allow the gradual resumption of weight bearing, range of motion, and strengthening.
In patients with persistent discomfort an intra-articular corticosteroid injection may be useful for both diagnostic and therapeutic purposes. When combined with a local anesthetic and injected into the ankle joint, the patient with a soft tissue impingement lesion should have at least temporary relief of their symptoms. The corticosteroid may control inflammation in the joint and allow further healing without need for surgery. If the patient denies even temporary relief during the period of anesthetic effectiveness, the evaluating physician should entertain the possibility that the patient’s problem does not emanate from the ankle joint. At this point another injection into the subtalar joint may be indicated to assess the possibility that the symptoms are arising from that joint rather than the ankle joint. Some patients may have communication between the two joints that may make interpretation of the diagnostic injection difficult. If neither injection affords symptom relief, the evaluating physician must consider other causes of persistent ankle pain arising from the soft tissue structures in the vicinity of the ankle or ankle pain secondary to a completely different source such as neurologically mediated ankle pain.
Surgical treatment is reserved for those patients with symptoms and signs consistent with soft tissue impingement of the ankle joint who fail to respond to nonoperative measures. Ankle arthroscopy is performed with the patient positioned supine on the operating table with the hip and knee of the affected side flexed and supported by a well-padded leg holder (Fig. 89.1). The leg holder should have a long thigh support segment and a short portion extending past the posterior knee crease so that when traction is applied to the joint, the force is placed against a broad area of the thigh rather than being concentrated over a short area in the popliteal fossa, which might contribute to increased venous obstruction and increase the chance of deep vein thrombosis.
After routine skin preparation and sterile draping, a noninvasive commercially available ankle distraction apparatus is placed and gentle traction is applied to the ankle joint (Fig. 89.2). The author recommends routine placement of anteromedial, anterolateral, and posterolateral portals on every patient (Fig. 89.3). The inflow is placed posteriorly, the arthroscope is initially placed anteromedially, and instruments are introduced through the anterolateral portal. Every ankle should be surveyed in an organized and reproducible manner by the operating surgeon. The author begins the evaluation from the anteromedial portal at the tip of the medial malleolus visualizing the deltoid ligament and then proceeds up the anteromedial gutter to the dome of the talus. The arthroscope is then directed in a posterolateral direction so that the entire talar dome and tibial plafond are visualized and palpated. The posterior joint is evaluated at this point and gentle manual pumping of the posterior soft tissues may help to visualize any hidden posterior loose bodies. The arthroscope is then turned laterally to visualize the “trifurcation” where the distal tibia, distal fibula, and the lateral talar dome are seen. The inferior bundle of the anterior inferior tibiofibular ligament is visualized as a vertically oriented structure at the anterior margin of the trifurcation. Bassett has suggested that hypertrophy of this structure may cause anterolateral impingement and may be associated with adjacent chondromalacia of the talar dome. The arthroscope is then directed into the anterolateral gutter to visualize the anterior talofibular ligament and the tip of the lateral malleolus. As the arthroscope is withdrawn across the anterior joint, the distal tibia and the talar neck can be evaluated. This exposure may be improved by diminishing the traction applied to the joint in combination with ankle dorsiflexion, which relaxes the anterior capsule to create increased space anteriorly.
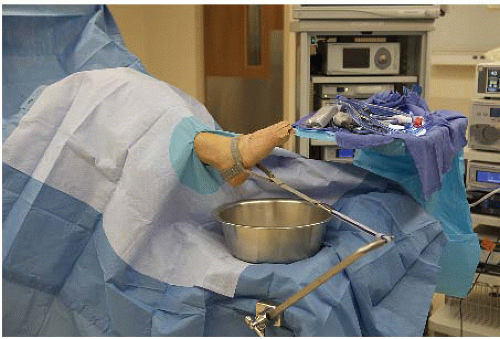 FIGURE 89.2. After routine skin preparation and sterile draping, the commercially available noninvasive joint distraction apparatus is attached. The distractor is completely sterile and allows the leg to hang in a plantigrade position, with good access to both anterior and posterior portals and with free intraoperative joint motion possible.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|






