Smith-Petersen Osteotomy for the Management of Sagittal Plane Spinal Deformity
Selvon St. Clair
William C. Horton III
DEFINITION
A number of osteotomy techniques have been described to treat severe or rigid sagittal plane spinal deformity.
These include multilevel anterior interbody radical discectomy and release, posterior pedicle subtraction osteotomy (PSO), vertebral column resection (VCR), and Smith-Petersen osteotomy (SPO).
This chapter reviews the SPO (also known as chevron or Ponté osteotomy), a mainstay in the treatment of sagittal deformity since it was first described in 1945 by Smith-Petersen and associates.16
ANATOMY
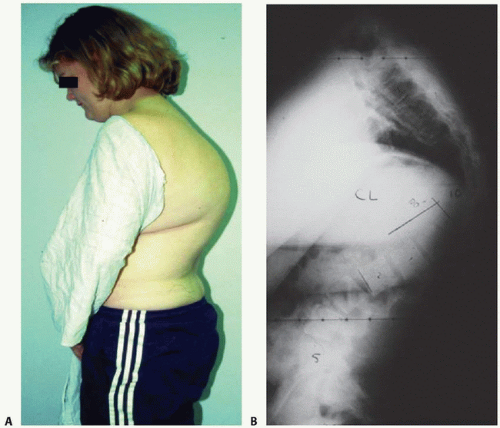
The SPO is indicated for correction of a fixed or partially fixed sagittal plane spinal deformity, including hyperkyphosis typified by Scheuermann kyphosis (FIG 1).
Although commonly used in the thoracic spine, it has also been used in the lumbar region to correct flat back syndrome or loss of normal lordosis.
PATHOGENESIS
The various causes of flat back syndrome include Harrington distraction instrumentation,5,11,12 anterior column degeneration, chronic vertebral compression fractures, adjacent segment degeneration, and iatrogenic causes with pseudarthrosis resulting in loss of sagittal plane correction.1,4
Additionally, the concepts behind SPO have been applied at the cervicothoracic junction for kyphosis such as in ankylosing spondylitis.
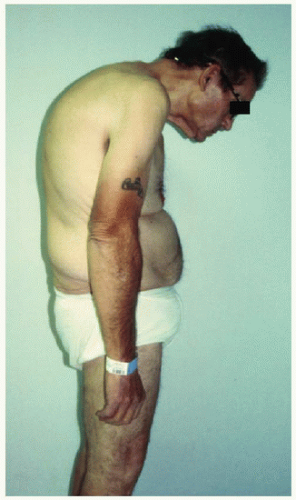
Regardless of the etiology, the clinical presentation of patients with sagittal plane spinal deformity is quite similar.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The flexibility of the deformity should be evaluated by both physical examination and preoperative planning radiographic evaluation.
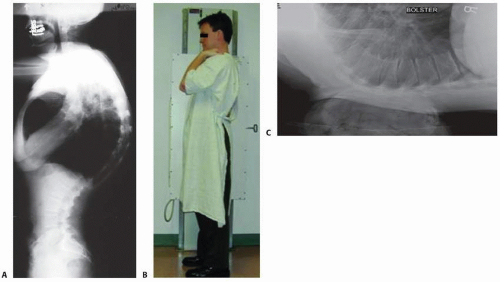
Radiographically, sagittal spinal deformity is evaluated with anterior posterior (AP), posterior anterior (PA), and lateral full-length radiographs with the knees extended and the hands resting on the clavicles (FIG 3A,B).9
The bolster supine hyperextension lateral radiograph or the push prone radiograph is also helpful to assess the rigidity of the deformity (FIG 3C). Further detailed analysis of coronal plane and segmental anatomy can be determined by computed tomography (CT) scan.
Sagittal imbalance is usually determined by the vertical plumb line technique9,10,13 as assessed on 36-inch plain film.
Neutral sagittal balance: Vertical plumb line falls at the center of dens or middle of C7 vertebral body aligned with the posterior-superior aspect of the S1 endplate on standing upright films.
Positive sagittal balance: Vertical plumb line falls anterior to posterior-superior aspect of S1 by a minimum of 2 to 3 cm.
Types of sagittal imbalance include the following:
Compensated abnormalities with neutral sagittal balance
Uncompensated abnormalities with positive sagittal balance that can be rigid or fixed
Attention must also be placed on the femurs and on pelvic parameters in evaluating global balance and in preoperative planning.14
SURGICAL MANAGEMENT
Standard SPO essentially involves complete resection of the facet complex bilaterally as well as any overlapping lamina and spinous process.
The posterior column bone resection must extend from pedicle to pedicle in a cephalocaudal direction. Facetectomies allow for shortening of the posterior column and a component of subsequent lengthening of the anterior column with middle column as fulcrum (FIG 4).
If done in the thoracic spine, the rib head and costovertebral articulation will also act with the middle column as the fulcrum for extension.
The end objective is increased lordosis by shortening the posterior column to restore the sagittal balance such that the head is centered over the sacrum.13
Modification of the SPO involves placement of an interbody graft or spacer in the disc space after complete discectomy and interbody arthrodesis. This method permits a greater degree of lordosis without compromising neural foraminal height and can be used to address coronal plane deformity by placing the interbody spacer asymmetrically in the disc space.13
It must be recognized that the degree of correction is governed by the flexibility of the anterior column and the effective preoperative disc height.
Ankylosis or bridging anterior osteophytes may significantly block the correction (FIG 5). In cases of rigid deformity, true anterior column osteoclasis helps to achieve a correction of up to 40 to 50 degrees, as may be seen with ankylosing spondylitis.15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree