Smith-Petersen Osteotomy and Pedicle Subtraction Osteotomy
Lukas P. Zebala
Keith H. Bridwell
DEFINITION
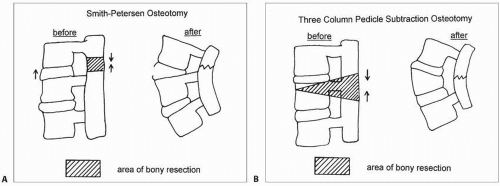
Smith-Petersen osteotomy (SPO) is a chevron resection of the posterior elements that shorten the posterior column and lengthen the anterior column upon closure (FIG 1A). The chevron osteotomy is called a Smith-Petersen osteotomy if performed through a prior fusion or a Ponté osteotomy if done through a nonfused spinal segment.
Pedicle subtraction osteotomy (PSO) is a posterior-based osteotomy that requires resection of the posterior elements, pedicles, and decancellation of the vertebral body in a V-shaped fashion through the transpedicular corridor (FIG 1B). The osteotomy hinges on the anterior column with closure of the middle and posterior columns creating a large cancellous bone footprint for fusion.
ANATOMY
A thorough understanding of spinal anatomy including spinal cord, nerve root, and vertebral segments is needed to safely perform these procedures. For an SPO, understanding the relationship of the interspinous ligaments, ligamentum flavum, facet joints, nerve roots, and spinal cord is important to resect enough posterior elements to allow osteotomy closure without posterior impingement. In a PSO, it is important to understand these same relationships, but in addition, the relationship of the exiting and traversing nerve roots to the corresponding pedicle is necessary to allow safe osteotomy closure.
SPO involves creating a chevron trough in the posterior elements by resecting the posterior elements through the facet joints and pars intra-articularis and posterior ligaments (supraspinous, intraspinous, and ligamentum flavum). A mobile disc space allows for closure of the middle and posterior columns and spontaneous opening of the anterior column.
A PSO requires a wide laminectomy from the pedicle above to pedicle below the osteotomy level, resection of the bilateral pedicles at the PSO level, and vertebral body decancellation to the anterior vertebral body in a wedge shape.
PATHOGENESIS
Sagittal imbalance is classified into type I and type II.
Type I sagittal imbalance is when there is a region of the spine that is fused in a hypolordotic or kyphotic position, but overall sagittal balance is satisfactory (sagittal C7 plumb falling through the L5-S1 disc space or slightly behind it on a standing long cassette lateral radiograph) as the patient is able to compensate through nonfused segments.
A type II imbalance is one in which the patient cannot compensate due to adjacent level degeneration resulting in a positive sagittal imbalance (patient leans forward in the sagittal plane).
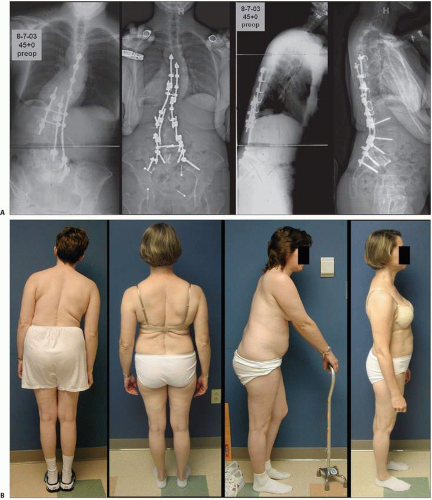
Type I patients often maintain their balance by hyperextending through mobile lumbar segments below the kyphotic segment. In type II imbalance, vertebral segments above or below the kyphotic area are substantially degenerated or fused and, therein, the spine is unable to hyperextend and maintain balance (FIG 2).
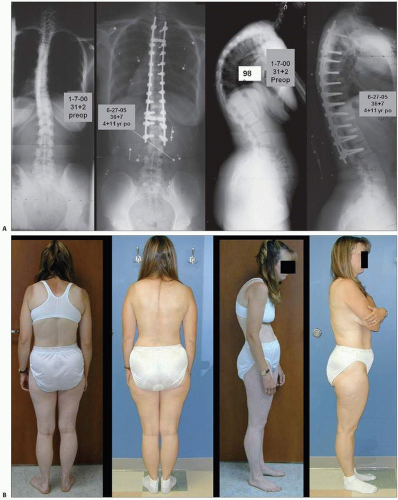
Kyphosis can be smooth and span several segments, such as in Scheuermann kyphosis (FIG 3), or sharp and angular, over one or two segments, such as in congenital or posttraumatic kyphosis.
These osteotomies are most often used for the correction of sagittal imbalance or kyphosis. SPOs are most often used to correct sagittal imbalance between 5 and 10 cm or smooth gradual kyphosis, whereas a PSO is used to treat sagittal imbalance greater than 10 cm or sharp, angular kyphosis within the lumbar spine. An asymmetric PSO can be done for a deformity that has both a coronal imbalance and sagittal imbalance together. A vertebral column resection (VCR) can be used to treat sharp, angular kyphosis within the thoracic or thoracolumbar spine.
NATURAL HISTORY
The natural history of the diseases/conditions leading to sagittal imbalance and kyphosis are variable, and a complete workup is necessary before recommending an osteotomy as a corrective operation.
Deformities that progress become rigid and, uncompensated, may present with intolerable pain, decreased ability to perform activities of daily living, or myelopathy and nerve root impingement.
PATIENT HISTORY AND PHYSICAL FINDINGS
The thorough history should include an understanding of the patient’s main reason(s) for seeking treatment, for example, progressive deformity, pain, loss of function, and neurologic deterioration.
The history should include a careful assessment of current pain medication usage as preoperative narcotic usage may complicate the perioperative care. Additionally, any medications that may confer a risk of increased bleeding (eg, acetylsalicylic acid) should be noted, and the patient is cautioned to stop them prior to surgery.
Patients should be questioned on their use of nicotinecontaining products, particularly cigarettes, as the risk of perioperative complications and pseudarthrosis is increased in these patients and may be a relative contraindication to these procedures.
Those patients with diabetes mellitus must have well-controlled blood glucose levels before and after surgery, as uncontrolled blood glucose levels are associated with increased risk of perioperative infection.
A patient’s nutritional status should be assessed and optimized prior to surgery. In addition, a bone density test should be performed to assess for osteoporosis, and appropriate treatment of these deficiencies or referral for their treatment should be initiated.
Patients with respiratory disease may require consultation with a pulmonologist or assessment of lung function by pulmonary function tests. Cardiac history should be assessed with the assistance of a cardiologist. Often, coordination with the patient’s primary care physician is necessary to get the patient ready for these surgeries.
The overall coronal and sagittal plane balance should be observed with the patient standing upright.
The deformity should be assessed for its flexibility by placing the patient prone and supine on the examination table. Several minutes of supine positioning will allow one to assess the flexibility of a kyphotic deformity.
A detailed neurologic examination assessing sensation, strength, reflexes, and pathologic reflexes is necessary. A complete neurologic examination should assess for signs of myelopathy (gait disturbance such as a wide-based gait, imbalance) or nerve root palsies (foot drop). In addition, assessment of hip and knee contractures is required as these conditions may make osteotomy correction and postoperative recovery more difficult.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographic assessment includes a series of standing fulllength 36-inch radiographs in the anteroposterior (AP) and lateral planes, left and right side bending radiographs if coronal deformity is present, and full-length supine or prone radiographs to assess spontaneous deformity correction.
Hyperextension radiographs (bolster placed at apex of kyphosis) and hyperflexion radiographs (bolster at apex of lordosis) help assess sagittal plane rigidity.
For sagittal plane deformity, comparison of standing AP and lateral radiographs to prone and/or supine fulcrum hyperextension long-cassette radiographs will help assess deformity flexibility.
Computed tomography (CT) scan is often obtained to assess prior fusion masses, bone quality, relevant bone anatomy at proposed osteotomy site, and bone anomalies (small pedicles) that may preclude safe fixation point placement. A CT myelogram may help assess areas of stenosis.
Magnetic resonance imaging (MRI) is often obtained to evaluate the spinal cord and nerve roots in addition to assessing for neural axis anomalies.
If SPOs are planned, assessment for mobile disc spaces is paramount as this is a requirement for this osteotomy.
DIFFERENTIAL DIAGNOSIS
Smooth global kyphosis (Scheuermann kyphosis)
Sharp angular kyphosis (posttraumatic)
Sagittal imbalance (types I and II) (flat back syndrome, postlaminectomy kyphosis)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree