Stage I
Diffuse synovitis, intact articular cartilage, volar capsular laxity
Stage II
Central focal articular cartilage loss of trapezium, deep metacarpal base loss, and synovitis
Stage III
Widespread articular cartilage loss, deep osteophyte on trapezium
The arthroscopic staging was gradually developed as a result of nearly 20 years of performing an arthroscopic assessment for recalcitrant basal joint arthritis which did not improve after often extensive conservative treatment. The condition is, of course, staged radiographically as per Eaton’s criteria [23]. Obvious exceptions were in patients with advanced (Eaton stage IV) arthritis with significant scaphotrapezial-trapezoidal (STT) arthrosis or trapezial collapse who then underwent a trapezial excisional suspensionplasty using a slip of abductor pollicis longus similar to Thompson’s description [24]. The advanced stage of disease really required excision of the entire trapezium, while stage IV patients with mild STT changes were still often treated via arthroscopy. Cobb describes a technique where both trapeziometacarpal and STT joints can simultaneously undergo arthroscopic treatment although I did not consider that in my treatment algorithm here described [25]. An additional exception was for older, low demand patients who did well using a cemented total joint arthroplasty as this required almost no immobilization and minimal therapy [26, 27]. This open surgery also allowed me to correct z-deformities by performing intrinsic releases of the adduction contracture coupled with an MCP volar capsulodesis. The last exception to arthroscopic management was the occasional young, usually male laborer who underwent a trapeziometacarpal joint fusion in good position of function for heavy pinch and grip. This indication for arthrodesis has been amply described in the literature and remains a good option, although arthroscopic hemitrapeziectomies may soon obviate even that procedure in some cases [28].
Except in clear-cut radiographic stages, where one can predict the arthroscopic stage, one performs the procedure with understanding that several therapeutic options are available once the arthroscopic stage is defined. These stages will later be delineated. The arthroscopic surgery is performed under wrist block regional anesthesia, usually only requiring several cc’s of lidocaine at median and radial sensory nerves of the wrist, 2–3 cm proximal to volar wrist crease. It is performed with tourniquet control and the upper arm is secured to arm board over this tourniquet via either wide tape or a Velcro strap. A single large Chinese finger trap is used on the thumb with 5–8 lbs. of longitudinal traction using a shoulder holder directly in line with the elbow flexed at 90° so that the thumb tip points to the ceiling. One can utilize the specialized wrist arthroscopy traction tower but is superfluous and more costly, since easy unencumbered access to the thumb is later necessary to drive a K-wire and fluoroscopy can be more easily introduced into the field. The trapeziometacarpal (TM) joint is then identified by palpating the more prominent metacarpal base. The joint is best localized by using an 18 gauge needle on a small syringe containing either lidocaine or lactated ringer’s solution so that the joint can be insufflated and distended. The needle needs to be introduced a bit more distal than expected and aimed cephalad since the metacarpal dorsal flare/lip needs to be cleared (Fig. 27.1). One can usually only introduce 1–2 cc due to small nature of the joint and the degree of laxity and joint swelling will influence this. Caution must be used to ensure the STT joint is not actually distended and less experienced surgeons should use fluoroscopy when the needle is in the joint to both confirm precise location and help determine trajectory of the soon to be placed trochar/sheath assembly. The location for this initial distention will often vary based upon which hand (left or right), and location of occasional large, interfering prominent osteophytes. The longitudinal portal stab wound incision is then made in line with the needle penetration and will likely be at either the 1-R or 1-U portal as described by Berger [5]. The incision for the 1-R (radial) portal is placed just volar to the abductor pollicis longus (APL) tendon and is typically used for clear assessment of the dorsoradial ligament (DRL), posterior oblique ligament (POL), and ulnar collateral ligament (UCL). The incision for the 1-U (ulnar) portal, which allows better evaluation of the anterior oblique ligament (AOL-volar/oblique) and UCL, is made just ulnar to the extensor pollicis brevis (EPB) tendon but palmar to the extensor pollicis brevis (EPL). The portals should be just distal to the dorsal branch of radial artery which lies across the ST joint, and should avoid any sensory radial nerve branches since the portals are, again, longitudinal, but one should always enter the capsule and spread with a straight small mosquito clamp. This will push the sensory nerves away from the portal sites. A short-barrel 1.9 mm 30° inclination arthroscope is usually used for complete visualization of the TM joint articular surfaces, capsule, and intrinsic ligaments. A 2.7 mm scope may be preferred when a more advanced Eaton stage is indicated since the larger scope may scuff the articular cartilage but is irrelevant in that scenario. The larger scope will actually assist in distracting the joint and provide a better field of view, while not risking the more delicate, and costly, 1.9 scope. A 2.0 mm full radius mechanical shaver with suction is used in most cases, particularly for initial debridement and visualization. Again, the larger 2.9 mm more aggressive shaver or cutter may be used in advanced cases where a hemitrapeziectomy is fully expected to be undertaken. The larger shavers allow for much better suction and evacuation of debrided joint material. Many cases utilize radiofrequency, for either ablation or thermal shrinkage as discussed, so need to be available per surgeon’s choice. Radiofrequency can also be used to perform chondroplasty in less advanced cases demonstrating focal articular cartilage wear or fibrillation. Ligamentous laxity and capsular attenuation are treated with thermal capsulorrhaphy also using the same RF shrinkage probe. One must be careful to avoid thermal necrosis and consequently, a striping technique is used to tighten the capsule of redundant or lax joints. Ample joint irrigation fluid is necessary during this treatment in order to minimize any thermal injury. In lesser stages of arthrosis, the arthroscopic treatment is completed once the joint synovectomy is performed, arthroscopic stage has been assigned, and the joint adequately debrided. Decision to use RF is made at this point but no further arthroscopic procedure is done in the early stages. Decision will have been made if adjunctive corrective metacarpal osteotomy is to be performed. In advanced cases, the shaver is now substituted for a mechanical shaver in order to proceed with partial trapeziectomy. A 2.9 mm long barrel type burr is then used to remove the distal 3–5 mm of remaining articular cartilage and subchondral bone. This is preferable to the round burrs due to speed and ease of use while some surgeons (Berner, Cobb etc.) try to utilize a larger, 3.5 mm burr since this will quickly remove the necessary trapezial surface. A strategic plan of joint resection is needed in order to avoid leaving significant prominent ridges or sections of the trapezium that may cause later impingement and persistence of pain. My strategy has usually been to divide the trapezial surface into four quadrants, two dorsal and two volar, or radial and ulnar. One begins at the area of shaver entry since the bone to resection is directly afoot, and this will create space to easier approach the other quadrants (Fig. 27.2). If the scope is in 1-R portal of a right thumb, then the burr would be in the 1-U portal facilitating subchondral resection of the dorsoulnar quadrant first. Once that side of the joint is cleared, the arthroscope can be changed to the opposite portal allowing the resecting burr to now enter the opposite portal, namely the 1-R portal in the previous example delineated. The radial palmar/dorsal quadrants can now be better approached for resection. At this point, several options are possible in order to encourage fibrous tissue ingrowth to create a new pseudojoint. Menon described a variety of materials including gore-tex, graft jacket, or tendon to interpose [4]. In my early experience, spanning nearly 10 years, I used a tendon graft which would serve as an “arthroscopic anchovy” and function as a biologic, albeit now inert, material to encourage fibrous ingrowth. This was quite successful and was even utilized in Ehlers-Danlos patients, notoriously known for poor results in basal joint reconstruction due to their extreme underlying joint laxity, the proposed cause for the current arthritic process. Several patients did well enough to request the opposite thumb be similarly addressed, and my first experience in handling this challenging clinical scenario was published as a case report [29]. However, the dead tissue being pushed into the joint was not easily controllable via portals and I did not feel the complete joint surface was well lined by this flimsy material, despite being autogenous. Around 2004, a synthetic but biologically compatible material known as artelon began to be used for open thumb CMC joint stabilization. This material degraded into lactic acid chains and CO2 over time, and there were basic science studies suggesting the neoformation of fibrocartilage in animals [30]. This material demonstrated good clinical results in several early studies, particularly showing improved pinch strength recovery as opposed to classic complete trapezial resection procedures [31]. While I too utilized it in a number of open cases, it soon became apparent that the material could naturally be used for an arthroscopic interposition (Fig. 27.3). The material “wings” did not need to be secured as the joint capsule itself would keep the material in place and it would serve as a scaffold for fibrous tissue ingrowth. This was described in a technique journal article but after many years, was largely abandoned by this author due to cost issues and other unrelated matters [32]. It should be noted that in my experience, and that of many others, there was never an adverse reaction clinically seen. However, a recent trend to simplifying the trapezial resection procedures led me to consider not interposing any material at all. Meals gave rebirth to the simple concept that resection of the trapezium alone would suffice and he added simple k-wire pinning of the joint in a distracted position soon termed “hematoma distraction arthroplasty” or HDA. He demonstrated very comparable results to much more complex procedures traditionally utilized [33]. This was simply a fancier delineation of complete trapeziectomy published by Gervin a half century ago [34]. However, it appears that the pinning provides several beneficial effects, including keeping the joint distracted so ample fibrous tissue can form within a maintained biologic cavity. The other advantage for the arthroscopic technique is that little joint stabilization is provided in this minimally invasive surgery; therefore, pinning of the metacarpal base over the trapezium keeps the joint well reduced and the metacarpal “centralized” over the functional center of the trapezium (Fig. 27.4). A thumb spica cast is typically worn for 5–6 weeks to allow for hematoma maturation and fibrous tissue ingrowth; hence any decrease in swelling, or unopposed pull of the APL tendon, might allow for dorsal re-subluxation of the metacarpal base, possibly hindering the formation of this stabilizing tissue. New techniques, including suture/bone button stabilization devices, allow for “suspension” of the metacarpal base without the need for pinning. However, complications such as impingement against the second metacarpal base, or bone fracture at the tunnel location, must be taken into account [35].

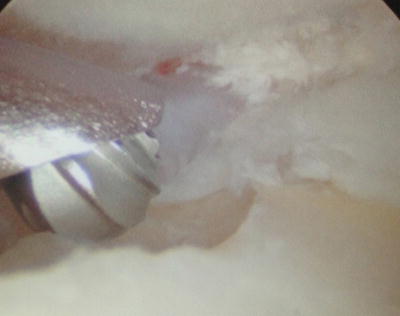



Fig. 27.1
Joint insufflation of the thumb basal joint in preparation for arthroscopic exploration. Note the needle trajectory which follows course of thumb metacarpal base flare and helps orient for correct arthroscope insertion angle
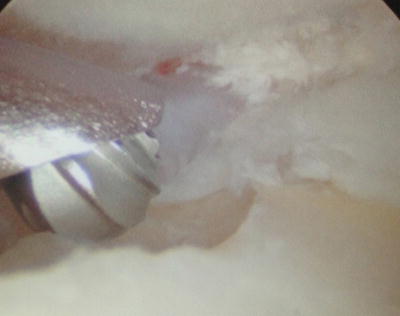
Fig. 27.2
Arthroscopic view of thumb trapeziometacarpal joint demonstrating dorsoradial resection of trapezial surface using a 2.9 mm burr in a Badia stage III arthritic joint

Fig. 27.3
Arthroscopic view of artelon polyurethane urea sheet lining the trapezium after arthroscopic limited hemiresection

Fig. 27.4
X-ray demonstrating transfixing pin of the thumb trapeziometacarpal joint in palmar abduction after arthroscopic hemiresection of the trapezium in a Badia stage III joint. The immobilization allows for fibrous tissue ingrowth in the new space created and now maintained by the temporary pin fixation
These arthroscopic interposition arthroplasties are obviously indicated for more advanced arthritis, but a joint modification might only be needed if the joint can be debrided and stabilized; hence a discussion on arthroscopic staging [8] is necessary to delineate when and how metacarpal base osteotomy is performed.
Staging by arthroscopy (Badia) is critical in order to indicate what further joint procedure, articular or extra-articular, is performed once the assessment has been made after synovectomy and appropriate debridement. Arthroscopic stage I patients are characterized by diffuse synovitis but with minimal, or no, articular cartilage loss (Fig. 27.5). Capsular or specific ligamentous laxity is a typical finding at this stage. This arthroscopic appearance is not commonly seen, since most patients present late, having dealt with symptoms for a prolonged period, or referred at a delayed time, once conservative means have been exhausted. Primary care physicians, orthopedic surgeons, and even hand specialists typically feel there are few options available to these patients failing traditional nonoperative treatment. These patients will undergo synovectomy, by both mechanical shaving and radiofrequency, with frequent shrinkage capsulorrhaphy performed depending on findings. The joint is then stabilized in a thumb spica cast from 1 to 4 weeks depending on the extent of capsular laxity. More unstable joints required longer immobilization in order to achieve joint stability and might also be pinned in a reduced position with thumb in palmar abduction. Stabilization of the capsule and aggressive synovectomy is hoped to slow the progression of articular cartilage degeneration.


Fig. 27.5
Arthroscopic view of Badia stage I basal joint arthritis illustrating the synovitis but intact articular cartilage surface on both trapezium and metacarpal base
Arthroscopic stage II patients are typified by focal articular wear on the central to dorsal aspect of the trapezium. It can be argued that this likely represents an irreversible degenerative process and demands a joint modifying procedure in order to alter joint deforming forces and progression of subluxation. Once synovectomy, debridement, and any loose bodies are removed, the joint is evaluated to determine the degree of instability and extent of capsular incompetence. A thermal shrinkage capsulorrhaphy is then often performed, with thermal chondroplasty occasionally done to anneal the cartilage borders (Fig. 27.6). The scope is then removed and an open incision usually extended from the ulnar portal is performed in order to identify the metacarpal base and metaphyseal-diaphyseal junction. A dorsoradial closing wedge osteotomy, according to Wilson’s original technique [36], is then performed in order to place the thumb in a more extended and abducted position altering the joint force vector (Fig. 27.7). Usually, only a 2–3 mm wide dorsoradially based wedge of bone is excised by combination of oscillating saw/osteotome. The idea is to minimize the tendency for metacarpal subluxation as well as change the contact points of degenerative articular cartilage. The osteotomy is stabilized usually by a single oblique Kirschner wire, also placed across the TM joint in a reduced position so that the metacarpal base sits squarely over the trapezium. This fixation allows for healing of the osteotomy in the reduced position and hopefully leads to a correction of the metacarpal subluxation, typically seen in this stage. A thumb spica short arm cast is worn during osteotomy bone healing and the wire is removed at 5–6 weeks post-op. While the osteotomy has been published as solely an open surgery by multiple authors, only arthroscopy can truly determine which patients should undergo this osteotomy. This has demonstrated good results in the past, including a more recent paper by Tomaino [37], but we can surmise that perhaps any poor results achieved were due to a poor indication; namely that only patients with a moderate stage of arthritis should undergo osteotomy, and this can now be determined arthroscopically. I published a modest series of patients having undergone this technique of combined arthroscopic debridement with metacarpal osteotomy while further outlining specifics of the technique [38]. This represented only a fraction of the potential patient series that underwent this surgery and, interestingly, even late follow-up on my patients has demonstrated that the metacarpal remains “centralized.” It is frankly unclear if the capsular shrinkage played a major role versus the alteration of joint mechanics by the osteotomy but suffice it to say that I have yet to convert any of these arthroscopic-assisted joint modifying procedures into any type of trapeziectomy or salvage procedure.



Fig. 27.6
Radiofrequency stabilization of the edge of a focal cartilage defect in a thumb Badia arthroscopic stage II. The joint contact points will subsequently be altered by a dorsoradial closing wedge osteotomy during same procedure

Fig. 27.7
X-ray showing centralized metacarpal base and pin fixation after dorsoradial closing wedge osteotomy in order to alter joint force vector and minimize further cartilage wear
Arthroscopic stage III is characterized by nearly complete trapezial articular cartilage loss (Fig. 27.8). The metacarpal base can also demonstrate loss of cartilage to varying degrees. Arthroscopic findings indicate that this is not an articulation that can be salvaged and a simple debridement or even joint modifying osteotomy would not provide a good result in this scenario. At this point, an arthroscopic hemitrapeziectomy, as earlier described, is performed by burring away the remaining articular cartilage and subchondral bone to achieve a bleeding surface. This acts to not only increase the joint space, but provides the key bleeding which creates the so-called hematomaplasty. Whether interposition material is placed or not, an oblique transfixing K-wire is used, coupled with a thumb spica cast in an abducted position, and maintained for about 6 weeks in order to encourage fibrous tissue ingrowth within the interposition space. This is followed by generally a minimal period of hand therapy to focus on pinch strengthening as joint motion is rapidly restored no matter what therapy is done. While Artelon material for interposition represents a good option obviating tendon procurement, it has become increasingly apparent that generous resection of the trapezial surface without specific interposition material should suffice.


Fig. 27.8
Arthroscopic view of the scaphotrapezial-trapezoidal (STT) joint showing scaphoid distal pole to be burred down limiting painful impingement from overlying trapezium and trapezoid
It should always be noted that arthroscopic stage III can also be treated by any traditional open technique such as excisional arthroplasty, arthrodesis, or even total joint replacement. This will largely depend on surgeon preference as well as patient needs and wishes.
Since arthroscopy remains underutilized and joint images are not readily available to study, we must take note of the correlations between arthroscopic and radiographic staging in order to better understand the role of arthroscopy and the typical findings at each stage. The most consistent arthroscopic findings in the group of patients who displayed radiographic changes compatible with stage I of the disease included fibrillation of the articular cartilage on the ulnar third of the base of the first metacarpal, disruption of the dorsoradial ligament, and diffuse synovial hypertrophy. We also noted attenuation of the anterior oblique or beak ligament (AOL) often being able to visualize the thenar muscles below the capsule, almost as a veil. The frequent injection of steroids likely influences this factor and a future study correlating frequency/amount of corticosteroids with joint findings would be quite valuable.
Typical arthroscopic findings seen in patients determined to be stage II arthritis were significant but focal wear of the distal surface of the trapezium, loss of metacarpal base cartilage near insertion of the AOL ligament, disruption of the dorsoradial ligament, and more significant attenuation of the AOL. We typically would also see more intense synovial hypertrophy. Most of the patients with this arthroscopic stage also presented as stage II radiographically, but it is not uncommon to discover patients deemed stage I may actually have more advanced findings once the joint is accurately assessed. This represents the great advantage of this technology since there is little other way to see what the true joint status is. Only rarely did we find less cartilage wear than was supposed or predicted on the plain X-rays. Therefore, radiographic stage III is only rarely considered stage II arthroscopically, but that finding would greatly influence and expand the treatment options. Since arthroscopic findings in early disease may have the most clinical impact on our decision making for definitive treatment, due to lack of good options for conservative treatment, it is important to review the patient outcomes for arthroscopic stage II disease.
In 2003, a retrospective assessment evaluated arthroscopic stage II patients with adequate follow-up in the prior 3-year period [38]. Forty-three patients (38 female and 5 male) had been arthroscopically diagnosed as having stage II basal joint osteoarthritis of the thumb between 1998 and 2001. All the procedures were performed by me with follow-up data generated by visiting fellows for objectivity. The average age was 51 with range of 31–69 years of age. The right thumb was involved in 23 patients and the left in 20. There was no improvement after a minimum 6 weeks of conservative treatment under my direction although most patients had been failing conservative measures by referring doctors for over a year. The surgical procedure consisted of arthroscopic synovectomy, debridement, frequent thermal capsulorrhaphy followed by an extension-abduction closing wedge osteotomy in all cases. A .045-in. Kirschner wire provided stability to the osteotomy site while a short arm thumb spica cast was maintained for 4–6 weeks until pin removal. The average follow-up was 43 months (range: 24–64 months).
Consistent arthroscopic findings in the selected group were frank eburnation of the articular cartilage of the ulnar third of the base of the first metacarpal and central third of the distal surface of the trapezium, disruption of the dorsoradial ligament, attenuation of the anterior oblique ligament, and synovial hypertrophy. The osteotomy healed within 4–6 weeks in all the cases. Radiographic studies at final follow-up depicted maintenance of centralization of the metacarpal base over the trapezium and no appreciable progression of arthritic changes in almost all 42 patients. Average range of thumb metacarpophalangeal (MP) joint motion was 5–50° and thumb opposition reached the base of the small finger in all cases. The average pinch strength was 9.5 lbs (73 % from non-affected side). At final follow-up patients were evaluated by Buck-Gramcko score, which takes into account both the subjective as well as objective outcomes [39]. The mean total Buck-Gramcko score in our series was 48.4 representing a “good outcome.” The constant pain in one of the patients was due to progressive osteoarthritis after the procedure. She did not respond to steroid injections and finally had to undergo arthroscopic-assisted hemitrapeziectomy due to progressive arthritis. A long-term follow-up should be obtained in future to better assess the utility of this technique and publish these findings specifically in stage II patients after minimum 10-year follow-up.
Arthroscopy in patients who had radiographic features of stage III and IV generally displays widespread full thickness cartilage loss with or without a peripheral rim on both articular surfaces, paradoxically less severe synovitis although we do note more frayed volar ligaments and often less laxity. This clearly constitutes arthroscopic stage III and the treatment options here are quite varied. The arthroscope can be removed and the most appropriate open procedure performed. I prefer the arthroscopic interposition arthroplasty in most of the cases. Based on the above findings and clinical experience, I proposed the arthroscopic classification and treatment algorithm as outlined in Table 27.1.
Trapeziometacarpal Arthroscopy: Clinical Utility
Clinical assessment and radiographic studies used to be the only tools available for the selection of treatment modalities for thumb CMC arthritis. Eaton and Glickel proposed a staging system for this disease that has been widely applied [20]. Later, Bettinger et al. [40] described the trapezial tilt as a parameter to predict further progression of the disease. They found that in advanced stages (Eaton III and IV) the trapezial tilt was high (50° ± 4°; normal: 42° ± 4°). Barron et al. concluded that there appears to be no indication for magnetic resonance imaging (MRI), tomography, or ultrasonography in the routine evaluation of basal joint disease [41].
While I believe that a radiographic classification is important for a stepwise interpretation of the progression of this entity, my experience has demonstrated instances when it is very difficult to make an accurate diagnosis of the extent of disease based solely on radiographic studies. Recent advances in arthroscopic technology have allowed complete examination of smaller joints throughout the body with minimal morbidity [1]. Moreover, arthroscopy has already proved to be reliable for direct evaluation of the first carpometacarpal joint as previously discussed [5].
In early stages of thumb basal joint arthritis, for instance, in Eaton stage I, it is very common to find essentially normal radiographic studies despite the presence of painful limitation of the thumb. In our experience, we have found that this group of patients displays mild to moderate synovitis which could benefit from a thorough joint debridement combined with thermal shrinkage of the ligaments to enhance the stability. This, of course, after assuming they have not responded well to conservative treatment including splinting, NSAID use, and corticosteroid injection. This stage is typically seen in middle-aged women who are not suitable candidates for more aggressive procedures. Arthroscopic treatment provides a particularly good option for this ubiquitous subset of the patients.
Tomaino concluded that first metacarpal extension osteotomy is a good indication for Eaton stage I [37]. This may not be necessary in the occasional patient who undergoes arthroscopy at an early time and demonstrates no focal cartilage loss. Future studies may indicate that synovectomy, and perhaps thermal capsulorrhaphy, may avoid progression of disease and the need for a mechanical intervention. However, the arthroscopic findings that I previously described for arthroscopic stage II of the disease demand a joint modification such as osteotomy, in order to minimize the chance of further articular degeneration. My retrospective study indicates that this approach is efficacious with only one out of 43 thumbs developing progressive arthritis requiring further surgery.
There remains little doubt that if complete articular cartilage loss is the arthroscopic scenario; the logical further step is to perform some type of trapezium excision with interposition arthroplasty. Menon described a technique demonstrating arthroscopic debridement of the trapezial articular surface and interposition of autogenous tendon, fascia lata, or Gortex patch into the CMC joint in patients with stage II and III with excellent results [2]. I have demonstrated that this arthroscopic technique is even effective in patients with underlying severe ligamentous laxity, as in Ehrler-Danlos syndrome [33]. Newer techniques may allow the arthroscopic insertion of Artelon, which has proven successful with open techniques and confirmed histologically [30]. In either case, complete excision of the trapezium may not be desirable, particularly in younger patients. The stage III treatment needs to be further assessed by evaluating long-term clinical results.
According to the arthroscopic classification proposed, I recommend arthroscopic synovectomy and debridement of the basal joint in patients with stage I arthritis. In patients with stage II disease, synovectomy and debridement is combined with dorsoradial osteotomy of the first metacarpal. In both these stages, thermal shrinkage is used to manage ligamentous laxity. Finally, for stage III of the disease, arthroscopic interposition arthroplasty is my treatment of choice, although other factors must be considered in making this determination.
Arthroscopic assessment of the trapeziometacarpal joint allows direct visualization of all components of the joint including synovium, articular surfaces, ligaments, and the joint capsule. It also allows for the extent of joint pathology to be evaluated and staged with intraoperative management decisions making based on this information. I recommend this arthroscopic staging to ensure better judgment of this condition in order to provide the most adequate treatment option to patients who have this disabling condition.
Future studies assessing the clinical long-term results utilizing arthroscopy will likely ensure its place in the treatment armamentarium for trapeziometacarpal osteoarthritis.
STT Arthroscopy (Scaphotrapezial-Trapezoidal)
Arthroscopy of the STT joint was a natural offshoot to the thumb CMC joint since the former is frequently involved when advanced basal joint arthritis is present. While Cobb reported simultaneous arthroscopic management of both TM and STT joints [42], the role of arthroscopy for the STT joint is likely best suited for focal disease where a minimally invasive option is sought. Ashwood and Bain described simple arthroscopic debridement for isolated STT arthritis demonstrating 90 % good and excellent results in their small series [43]. Fontes also described simple resection of the distal pole of the scaphoid as a useful technique for painful STT arthrosis [44].
The technique is relatively simple since instability is not an issue and the goal is to increase the joint space and avoid painful impingement. The joint is localized by ascending the scaphoid from the radial midcarpal portal, followed by creating a working portal that can be volar [44] or more recently, a radial portal has been described by Carro et al. [45]. Simple debridement is done using a 2.0 mm full radius shaver and then limited resection of the distal pole of the scaphoid is performed using burr (Fig. 27.9). The joint space is markedly widened but one must be careful to not resect the critical volar ST ligaments, one advantage of this procedure as opposed to open techniques.
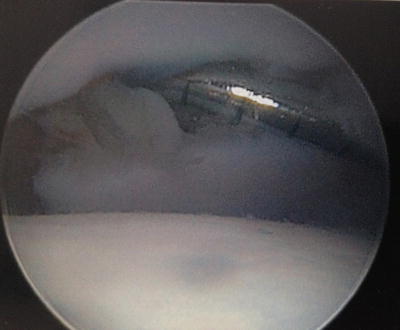
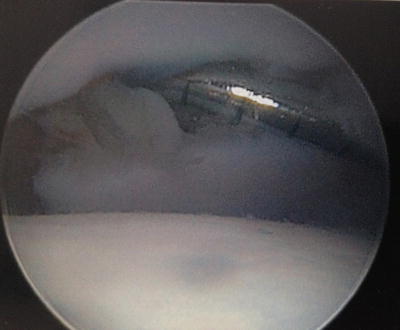
Fig. 27.9
Arthroscopic view of the thumb MCP joint illustrating how a hook probe can derotate an avulsed bony gamekeeper fragment, obviating the need for joint arthrotomy to reduce
Minimal post-op immobilization is another surgical advantage of this methodology, and pain relief is generally excellent assuming patient selection was properly performed.
A long-term study is necessary to determine the late outcomes and secure the role of STT arthroscopy amongst the various techniques used for treatment of this common arthritic malady.
Metacarpophalangeal Arthroscopy
While arthroscopy of the metacarpophalangeal joints of the hand was first described almost three decades ago, the clinical utility and indications remain poorly understood. Many orthopedic surgeons are unfamiliar with this possibility, hence unable to offer it to their patients as an option. Furthermore, hand surgeons rarely utilize this technology despite the fact that both acute injury and chronic pain are commonly found in the MCP joint, thumb, and digits alike. It seems that minimal exposure within the literature as well little hands on training has contributed to the underutilization of what is a very useful technique to manage certain pathology in the hand.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








