Small Joint Arthrodesis of the Hand
W. Lee Richardson
Warren C. Hammert
INDICATIONS
Arthrodesis of the small joints in the hand can be useful for a variety of conditions. Although arthritis is the most common indication, irreparable tendon loss from trauma, reconstruction after tumor resection, contractures, and some neurologic conditions can be treated with arthrodesis, preserving function of the hand (1,2).
Small joint arthrodesis of either the proximal interphalangeal (PIP) or distal interphalangeal (DIP) joints (interphalangeal joint of thumb—IP joint) is most commonly performed for arthritis (osteoarthritis, posttraumatic arthritis, and occasionally rheumatoid or other inflammatory arthritides). Pain and stiffness associated with these arthritides are common indications for arthrodesis. In addition, joint deformity in the coronal plane may interfere with function, and contractures in nonfunctional positions can be problematic. In the thumb, the metacarpophalangeal (MCP) joint can be fused and provide good outcomes with minimal loss of function, assuming there is good function of the IP and trapeziometacarpal joints. Arthrodesis of the MCP joints of the fingers can be more limiting and thus, arthroplasty is often preferred (2).
There are multiple fixation techniques for arthrodesis in the hand including K-wire and tension band, intramedullary screws, and plate and screws. Overall, comparable results can be achieved using any of these fixation techniques. Ultimately, surgeon comfort with a particular technique should guide the surgical decision (3,4,5,6,7,8).
CONTRAINDICATIONS
Infection or poor soft-tissue coverage may be contraindications for arthrodesis. Every attempt should be undertaken to eradicate infectious organisms and provide adequate soft-tissue coverage prior to surgery. Shortening of the digit during the arthrodesis can improve the soft-tissue coverage. Additionally, the patient must be able to comply with the postoperative program to ensure healing of the arthrodesis site.
PREOPERATIVE PREPARATION
Orthogonal x-rays should determine the presence of arthritis in the joint and potential joint deforming entities such as cystic change or bone loss.
If intramedullary screw fixation is considered, the intramedullary size should be evaluated prior to surgery as differences will often dictate screw diameter.
Specific lab workup (e.g., rheumatoid factor, ANA, uric acid) and rheumatology consultation for suspected inflammatory or erosive arthritides can be ordered at this time if desired but may not change surgical tactic (9,10).
Proposed angles of fusion for specific joints are as follows:
DIP joints fused in 0 to 10 degrees flexion
PIP joints fused in 40, 45, 50, and 55 degrees of flexion from index through small finger
MCP joints fused at 25, 30, 35, and 40 degrees of flexion from index through small finger
Thumb IP joint 0 to 10 and MCP 10 to 30 degrees of flexion
TECHNIQUE
General Approach
For the DIP joint, a midline incision or H-incision is normally employed with release of the terminal extensor tendon over the joint. Care is taken to avoid the germinal matrix when preparing the distal phalanx. The tendon is repaired during closure to provide soft-tissue coverage over the joint.
The PIP joint can be approached through a dorsal curvilinear incision with release of the central slip. Upon completion of the arthrodesis, the central slip is closed similar to the terminal extensor tendon at the DIP joint.
Excise collateral ligaments from both sides of the joint.
Expose the entire proximal and distal joint surfaces with hyperflexion of the joint.
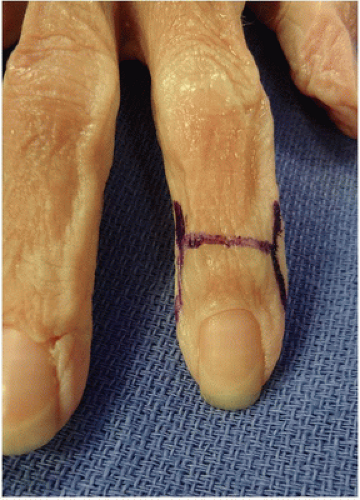
Use a curette, rongeur, or burr to remove remaining cartilage and subchondral bone until cancellous bone is present on both surfaces. The joint surfaces should be prepared so they create a fusion angle as noted above. It is important that fusion surfaces correspond to each other as symmetrically as possible. This allows for a larger contact area for more reliable fusion and may be accomplished by creating cartilage-free flat surfaces or utilizing the cup-and-cone technique where the convex surface of the proximal joint surface corresponds to the distal concave surface (Figs. 23-1, 23-2, 23-3 and 23-4) (11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree