Thorough evaluation of the athlete with persistent shoulder instability and appropriate use of imaging modalities, such as 3-dimensional computed tomography, can help quantify the severity of bony deficiency. Based on obtained imaging and examination, surgical and nonsurgical methods can be considered. In many situations both the humeral- and glenoid-sided bone loss must be addressed. Depending on the extent of bone loss, athletic demands, and surgeon experience, arthroscopic or open surgical options can provide shoulder stability and return athletes to their prior level of activity.
Key points
- •
The prevalence of clinically relevant bone loss is likely underestimated, with critical bone deficiency present in a high percentage of patients with multiple recurrent dislocations or prior failed stabilization surgery.
- •
Of the several options for the imaging quantification of bone loss, 3-dimensional computed tomography reconstruction is the current gold standard.
- •
As little as 6 mm of bone loss can translate into approximately 20% to 25% of the native glenoid surface; when glenoid bone loss exceeds 20%, glenoid bone augmentation is the currently accepted form of surgical management.
- •
Adopting an algorithmic approach to the athlete with glenohumeral instability and associated bone deficiency will help achieve the most predictable outcomes with regard to stability and return to activities.
Introduction
Shoulder instability is common in athletes, often resulting from an initial traumatic dislocation event. Glenohumeral dislocations and subluxations, especially those occurring at a young age, can lead to recurrent instability events, which can jeopardize performance in elite athletes. Following initial traumatic dislocation, repeated trauma to the glenoid can result in glenoid rim fractures, attritional bone loss, and soft-tissue injury. Over time this may lead to glenoid, humeral, or dual-sided bony deficiency and a change in the overall architecture of the shoulder. Previous failed fixation of bony Bankart and labral abnormality may also lead to insufficiency, prompting consideration of further options.
Thorough evaluation of the athlete with persistent shoulder instability and appropriate use of imaging modalities can help quantify the severity of bony deficiency. Based on obtained imaging and examination, surgical and nonsurgical methods can be considered. In many situations both the humeral-sided and glenoid-sided bone loss must be addressed. Depending on the extent of bone loss, athletic demands, and surgeon experience, arthroscopic or open surgical options can provide shoulder stability and return athletes to their prior level of activity.
Introduction
Shoulder instability is common in athletes, often resulting from an initial traumatic dislocation event. Glenohumeral dislocations and subluxations, especially those occurring at a young age, can lead to recurrent instability events, which can jeopardize performance in elite athletes. Following initial traumatic dislocation, repeated trauma to the glenoid can result in glenoid rim fractures, attritional bone loss, and soft-tissue injury. Over time this may lead to glenoid, humeral, or dual-sided bony deficiency and a change in the overall architecture of the shoulder. Previous failed fixation of bony Bankart and labral abnormality may also lead to insufficiency, prompting consideration of further options.
Thorough evaluation of the athlete with persistent shoulder instability and appropriate use of imaging modalities can help quantify the severity of bony deficiency. Based on obtained imaging and examination, surgical and nonsurgical methods can be considered. In many situations both the humeral-sided and glenoid-sided bone loss must be addressed. Depending on the extent of bone loss, athletic demands, and surgeon experience, arthroscopic or open surgical options can provide shoulder stability and return athletes to their prior level of activity.
Natural history of bone loss
The ability to counsel athletes presenting with varying degrees of bone loss depends on a proper understanding of the natural history of glenoid and humeral bone defects. The unconstrained nature of the glenohumeral joint in terms of osseous stability imparts a predisposition for recurrent joint instability. Young athletes and those who participate in contact sports are most prone to developing recurrent dislocation or subluxation events after an initial traumatic dislocation. These events most commonly result in anterior inferior “Bankart” labral tears, occurring in approximately 97% of dislocations.
Age has long been regarded as the most important factor for recurrence. Sachs and colleagues reported on predictive factors for recurrence and identified young age and contact sports as primary risk factors for recurrence. Glenoid fractures and Hill-Sachs lesions can be present from the initial dislocation event as well, and may go unrecognized; this can alter the necessary bony constraint within the glenohumeral joint. Burkhart and De Beer identified that failure to address the bony aspect of injury, including Hill-Sachs lesions, may lead to failed instability surgery. This finding has led to recent discussion regarding proper treatment of first-time dislocators. Even if there is not an initial bony lesion, repeated dislocation events over time will often lead to glenoid erosion and development of a characteristic pattern of bone loss, known as the “inverted pear” glenoid.
Some athletes may be predisposed to glenohumeral instability based on their native glenoid architecture and glenoid version. Some amount of bony deficiency is present in approximately 22% of patients after initial dislocation. The incidence climbs to nearly 90% after failed prior stabilization surgery. Most of these defects are located on the anterior inferior glenoid between 2 and 6 o’clock, consistent with the common direction of instability events. Posterior glenoid fractures and insufficiency do occur, though much less commonly.
The type of sport may also influence the morphology of the glenoid lesion depending on the mixture of direction of axial and shear force applied to the joint at the time of injury, as demonstrated by Burkhart and De Beer. Smooth-appearing lesions without a clear fracture fragment may be found in the setting of lower-energy chronic dislocations presenting over a longer term, whereas glenoid rim fractures are more common among football players presenting more acutely. In the setting of recurrent dislocations persistent for longer than 6 months, the glenoid may remodel completely.
The Hill-Sachs lesion is a compression defect of the humeral head that is associated with shoulder instability. This lesion occurs in approximately 40% to 90% of athletic shoulder instability and generally occurs in the abducted, externally rotated position. Those humeral-sided lesions that do not engage are typically not parallel to the glenoid face when the shoulder is in abduction and external rotation. Reverse Hill-Sachs lesions (anterosuperomedial humerus lesion) occur in posterior shoulder instability.
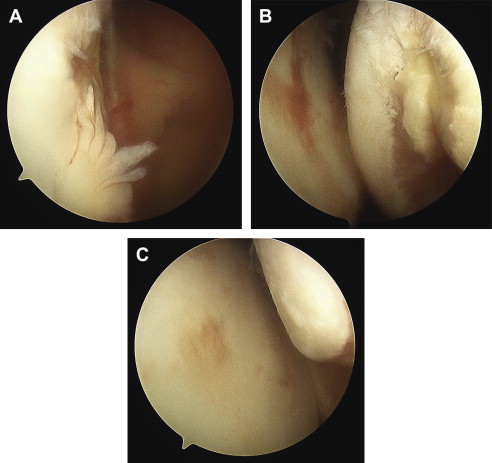
The humeral head defect may also remodel, and the progression on the humeral side combined with attritional glenoid-sided loss can combine to lead to an “engaging” Hill-Sachs lesion ( Fig. 1 ). These bipolar lesions need to be assessed by quantification of both the glenoid and humeral involvement, and treatment in this setting can be challenging. In the setting of isolated humeral-sided bone loss with engagement, which is less common than isolated glenoid-sided loss, a specific subset of surgical options can be considered.
Biomechanical effects of bone loss
The stability of the native glenohumeral joint depends on both static and dynamic restraints. Provencher and colleagues identify 3 key contributors to joint stability: concavity-compression and the bony architecture, the glenohumeral capsuloligamentous structures (static stabilizers), and the coordinated contraction of the rotator cuff and periscapular musculature (dynamic stabilizers).
Bone loss on the glenoid and/or humeral sides can lead to a well-described cascade of events. Loss on the glenoid side can create a discrepancy in the articular area. The concave surface of the glenoid provides a point on which the humerus can be compressed, assisted by the labrum, which deepens the concavity of the glenoid and serves as a site of ligament attachment. Lack of the labral buttress and disruption of bony architecture can lead to instability events, which can contribute to a cycle whereby both the glenoid-sided and humeral-sided lesions increase in size, compounding the problem. The cancellous architecture of the posterolateral humerus is prone to continued compression injury, with the cortical anterior glenoid bone as the assailant. In addition, the capsule has been demonstrated to stretch in the setting of recurrent instability. Restoration of the proper glenoid articular arc is one method to help restore stability that is affected by these numerous disadvantageous factors.
The concept of glenoid track is influenced by bone loss. As described by Yamamoto and colleagues, the glenoid contact area shifts from inferomedial to superolateral portion of the posterior aspect of the humeral head, termed the glenoid track. These investigators reported that a Hill-Sachs lesion is at higher risk of engagement if it extends medially over the medial margin of the glenoid track. For the athlete, increased glenoid bone loss decreases the size of this glenoid track, making engagement and recurrent instability more common. In the setting of more substantial loss of glenoid bone, the bipolar nature of these lesions makes it possible that less humeral-sided bone involvement is needed for significant instability to occur, and vice versa.
Clinical evaluation
History
Crucial to treating recurrent instability with bone loss in the athlete is a comprehensive understanding of the patient’s history of instability. First and foremost, the details of the initial instability event should be identified. Patients with a history of shoulder instability have been determined to have a 5-fold increased risk of further instability. The direction of dislocation can be helpful in determining the expected pathology (anterior, posterior, multidirectional). The mechanism of injury, including the position of the arm at the time of both the initial dislocation, is important to ascertain. In addition, the point at which the patient feels initial subluxation and apprehension may provide information on the degree of bone loss. The method by which the patient has been reduced may also assist in the initial approach to the injury. In addition, reported dislocation events that occur during low-energy activity such as sleeping and reaching for an object are concerning for more severe pathoanatomy associated with recurrent instability, especially concomitant bone loss on one or both sides of the joint.
Understanding the patient’s prior treatment to date is also critical in creating a plan moving forward. An initial period of attempted nonsurgical management may or may not be advised depending on the patient’s presentation, time in season, and the existing soft-tissue and bony abnormality.
An expanding volume of literature is available on the significance of instability following previous stabilization attempts. These prior attempts may increase the likelihood of bony insufficiency. Every effort should be made to obtain prior arthroscopic photos and imaging to assist in formulating an appropriate strategy for each individualized patient.
Physical Examination
The approach to physical examination of the patient with suspected glenohumeral instability should be both comprehensive and standardized. The patient should be examined with both shoulder girdles well visualized. Examination should always begin with examination of the unaffected side to provide a framework within which to compare the pathologic side. Observation of the active shoulder motion from behind the patient may reveal scapular dyskinesis, scapular winging, or muscular atrophy. Joint range of motion, both active and passive, should be measured and compared with the unaffected side, looking for both laxity and adaptive loss of motion such as internal rotation deficit, which can be seen in the overhead athlete.
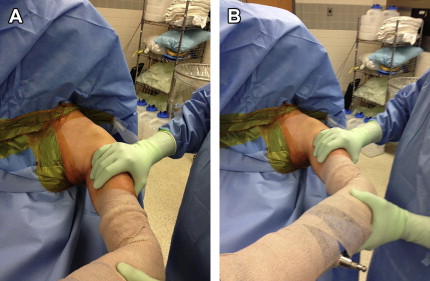
Separate from general range of motion testing is evaluation of stability in specific planes. Provocative maneuvers include the load and shift test ( Fig. 2 ), which may be used to evaluate translation of the humeral head over the glenoid rim. The apprehension sign is a useful test to evaluate shoulder instability. This test is best performed with the patient lying flat on the examination table. In the case of bone loss, nearly all patients will exhibit a positive apprehension test at 90° abduction and maximal external rotation of the involved shoulder. Of note, patients with critical bone loss will frequently demonstrate apprehension in a lower position of abduction (20°–60°), likely indicating engagement at this position. Inferior shoulder laxity can be tested by the sulcus sign, which is achieved with inferior traction on the humerus and measurement of the distance from the lateral acromion to the humerus, and comparison with the contralateral side. Position of subluxation or engagement of a Hill-Sachs lesion is often better quantified under anesthesia.
Side-to-side comparison of strength testing should be performed next. Although structural injury to the rotator cuff with a dislocation event is more common in older individuals, rotator cuff strength should also be closely evaluated in the younger athlete. Subscapularis function, as delineated by strength testing of internal rotation as well as the lift-off and belly-press tests, should be documented, especially in patients who have had previous anterior open procedures. Knowledge of the management of subscapularis should be obtained in the referral situation.
Imaging Analysis
On initial presentation plain radiographs are helpful in confirming reduction, and may show a bony Bankart fragment, best detected on a variation of the axillary lateral. Hill-Sachs lesions can be visualized best on an anteroposterior variant called the Stryker Notch view. This internal-rotation view of the humerus brings the posterior and lateral aspect of the humerus, the typical Hill-Sachs area, into view. Certain radiographs provide more accurate assessment of the glenoid articular surface, including the West Point view and Garth apical oblique view.
Advanced imaging, which should be considered in the further workup of glenohumeral instability in most patients, may often include magnetic resonance (MR) imaging or MR arthrography, which best evaluates the soft-tissue structures such as the labrum, joint capsule, rotator cuff, and cartilage. When there is suspicion for bone loss, the optimal study is currently a computed tomography (CT) scan.
Glenoid rim fragments and attritional bone loss can be best characterized by CT scan with 3-dimensional (3D) reconstruction. Two-dimensional (2D) CT depends on orienting the beam perpendicular to the glenoid face, which thereby depends on the version. If not entirely perpendicular, the bone loss may be either overestimated or underestimated. The surgeon must also understand the role of the slice distance to quantify bone loss.
Sugaya and colleagues evaluated 100 shoulders with recurrent instability using en-face 3D reconstructed CT. Fifty osseous Bankart fragments of varying sizes were identified, with large fragments occupying 26% of the glenoid fossa. In addition, 90% of those evaluated had a glenoid-rim lesion of some type.
Deficiency measurement and classification
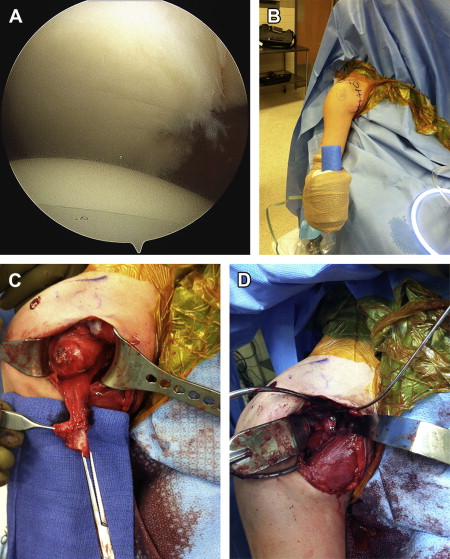
Preoperative quantification of bone loss is crucial for surgical decision making. CT has been shown to be superior to plain radiography when evaluating the glenoid, as it provides an en-face oblique view. 3D CT with digital subtraction of the humerus is now considered the gold standard, and allows reliable surgical planning and quantification of glenoid defects ( Fig. 3 ). The humerus can also be included and later subtracted to allow for evaluation of Hill-Sachs defects.
Bigliani and colleagues defined 3 types of glenoid lesions based on plain radiographs, with type I being an avulsion fracture, type II a medially displaced fragment, and type III an erosion of the glenoid. Typically the critical value of 25% of total glenoid surface (or 6–8 mm defect in most glenoids) is used when discussing the need for open techniques and augmentation procedures, because of the known failure of standard Bankart repairs in this subset of patients.
Itoi and colleagues performed a biomechanical study testing shoulder instability with progressive bone loss, in which they osteotomized the glenoid sequentially and identified a critical drop-off in glenohumeral stability when 21% of the glenoid was removed. Patients with glenoid bone loss and inferior hyperlaxity are particularly at risk for recurrent instability, according to Boileau and colleagues’ analysis of risk factors for recurrent instability. The key question is how this 25% is accurately calculated.
There are several methods to determine bone loss by imaging and arthroscopy ( Fig. 4 ). One technique involves measuring the distance from the bare spot to the posterior or unaffected rim, and then from the bare spot to the edge of the area of bony deficiency. The percentage of attritional loss is then calculated using the following formula: ([B − A]/2B) × 100%. Another method involves using the en-face view of the glenoid on 2D CT imaging and measuring the width-to-length ratio and glenoid bone defect length calculations which, when compared with glenoid diameter, are predictive of recurrent instability.
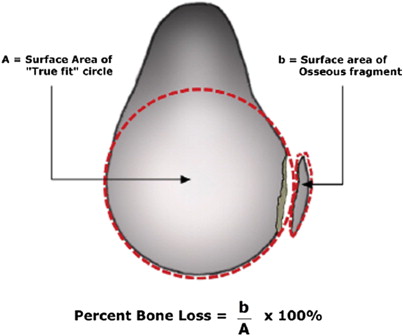
As discussed previously, glenoid bone loss can also be perhaps most accurately assessed using CT with multiplanar reconstructions and digital subtraction of the humeral head. Once the en-face view is obtained, the defect can be measured directly. In addition, a true best-fit circle around the inferior glenoid can be drawn with the center at the approximate bare area ( Fig. 5 ). Once the circle is drawn, the amount of bone loss can be calculated relative to this by dividing the surface area of the bony defect by the area of the circle. Measuring the length of the glenoid defect alone has also been shown to provide prognostic information regarding recurrent instability.
Arthroscopy also can be used to qualify and quantify glenoid bone loss. The glenoid bare-spot method can be used, although this may overestimate bone loss depending on the location of the bony defect in relation to the bare spot, which may be difficult to identify in all shoulders. The bare-spot method has been scrutinized and found to be unreliable by some surgeons. It is best at estimating those defects that occur parallel to the long axis of the glenoid.
Classification of humeral-sided lesions has also been described. Most of these descriptions use either CT-scan quantification based on the humeral defect as a percentage of the circumference of the humeral head, or direct visualization of the humeral-sided defect. To date, no consensus has been reached on the clinical utility of these classifications in guiding treatment. Some classifications focus on significance, whereas others focus on size or grade of injury.
Finally, it is important to consider the athlete who has undergone multiple attempts at stabilization. Inflammatory reaction to retained devices may provide a larger relative zone of damaged bone. Glenoid rim fractures that propagate through prior anchor sites can occur and can be technically challenging to treat. Previous arthroscopic images coupled with current imaging consisting of both MR arthrography and 3D CT can demonstrate expected bone loss after debridement of the glenoid edge. It is clear that even 1 to 2 mm of bone can make a large difference for the athlete in terms of stability.
Nonsurgical care
Following history, physical examination, and imaging quantification of both soft-tissue abnormality and glenoid-sided or humeral-sided bone loss, a decision must be made regarding treatment. Whether to treat young athletes with surgery after first-time dislocation remains an area of controversy. Buss and colleagues evaluated 30 athletes with shoulder instability over a 2-year period. Although nearly all returned to play, 37% had recurrent instability when treated nonoperatively. Another recent study demonstrated that primary arthroscopic stabilization may in fact be more cost effective than nonoperative management for first-time dislocation. Risk factors for recurrence after arthroscopic stabilization include bone loss, fewer than 4 anchor points, and shoulder hyperlaxity. Given that bone loss is a risk factor for recurrent instability, there is little room for nonoperative care in the athlete presenting with bone loss.
The options for nonsurgical management in the athlete with recurrent instability include rest, physical therapy/rehabilitation with an emphasis on rotator cuff and periscapular strengthening and dynamic stability, and bracing for competition. In-season bracing has been evaluated by Buss and colleagues and is an option for some athletes, primarily based on their sport and position. In a cohort of 30 patients who were managed in season with a shoulder brace or harness for anterior instability, 26 were able to return to sports. Of these, 10 reported at least 1 episode of recurrence in the brace and 16 eventually required surgical stabilization at the completion of the season.
If immobilization and physical therapy is pursued, some evidence has suggested that doing so in external rotation can decrease recurrence rates. Although the initial data on this approach offered some promise, the timeliness required to institute this intervention combined with difficulties with patient compliance have led to inferior results in duplicated studies of external-rotation bracing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






