Fig. 15.1
MRI in ABER position showing partial articular rotator cuff tear
A study suggests that CT and MR arthrography have similar diagnostic performance for the evaluation of rotator cuff tendon tears. There was no statistically significant difference in sensitivity and specificity between CT arthrography and MR arthrography in depiction of rotator cuff lesions [19].
15.2.1.2 Imaging Findings in Impingement Syndrome and Rotator Cuff Tears
Radiographs should be obtained to evaluate possible bony abnormalities of the coracoacromial arch. Routine radiographs include AP and Grashey views (AP radiograph of the shoulder in the plane of the scapula) as well as outlet and axillary views. The outlet view provides visualization of acromial morphology, and the axillary view best demonstrates evidence of os acromiale, which may lead to secondary impingement.
Acromioclavicular joint osteoarthritis with inferior osteophyte formation, acromial enthesophytes or sclerosis, and cystic changes of the humeral head are the more common radiographic findings related to impingement. However, all of these findings may be present in asymptomatic subjects, making the relationship of such findings to the diagnosis of impingement controversial.
MRI provides a detail of potential sites of subacromial impingement through the supraspinatus outlet. Ossification of the coracoacromial ligament (CAL) or the presence of a subacromial spur can be best identified in the sagittal oblique plane; however, differentiation of a pathologic spur and the normal CAL can be difficult. MRI also may demonstrate findings of subacromial-subdeltoid bursitis. Findings that indicate this condition include bursal thickness >3 mm, the presence of fluid medial to the acromioclavicular joint, and the presence of fluid in the anterior aspect of the bursa [20].
Subacromial Bursitis-Bursal Effusion
Fluid distending the subacromial-subdeltoid bursa is a nonspecific finding, as it may be encountered in association with subacromial impingement, partial or complete rotator cuff tears, and calcifying tendinitis.
During impingement of the supraspinatus tendon, the subacromial-subdeltoid bursa becomes compressed between the greater tuberosity of the humeral head and the anterior portion of the acromion. This chronic compression can result in an inflammatory reaction of the bursal synovium and secretion of fluid into the bursa. Fluid is not detected in the normal bursa [21]. Fluid in the bursa is recognized on T2-weighted images as the increased signal intensity of the subacromial-subdeltoid bursa indicates local bursal inflammation [22].
Tendinosis
A normal supraspinatus tendon should exhibit low signal intensity on all pulse sequences. There is general agreement that a focal area of increased signal intensity on a T1-weighted image without increased signal intensity on a T2-weighted image and without thickening or thinning of the tendon is due to the magic angle artifact or is without clinical relevance.
A tendon with focal or diffuse increased signal intensity on proton density-weighted images without further increase of signal intensity on T2-weighted images and an indistinct margin at the articular side of the supraspinatus tendon corresponds to eosinophilic, fibrillar, and mucoid degeneration and scarring. Tendons with areas of increased signal intensity on T2-weighted images are associated with severe degeneration and disruption of the supraspinatus tendon [23] and have increased signal intensity also on STIR and T1-weighted images. No focal or linear area of water-equivalent signal intensity is seen.
Tendinosis in many cases is a result of impingement syndrome. Fluid collections can be present in the subacromial-subdeltoid bursa, findings similar to that of inflammation. This early stage of rotator cuff disease is frequently called tendinitis.
Partial-Thickness Tears
Partial-thickness tears of the rotator cuff can be articular-sided, bursal-sided, intratendinous, or a combination thereof. Partial-thickness tears are subdivided based on location and thickness of tear.
Throwing athletes may show a predilection for articular surface tears [24]. Most tears affect the supraspinatus tendon. The infraspinatus, subscapularis, and teres minor tendons are much less commonly involved [25, 26].
Isolated intratendinous tearing of the supraspinatus tendon is rare, and most cases are associated with bursal or joint side cuff tears [10]. If fluid is present, water-equivalent signal intensity is seen in the area of the defect (Fig. 15.2). Partial-thickness tears are usually circumscribed and rarely exceed 10 mm, measured in the AP or sagittal direction. They can be missed by MRI and arthrography [27].
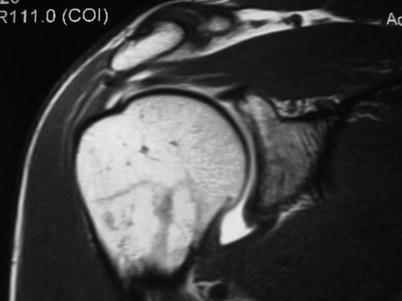
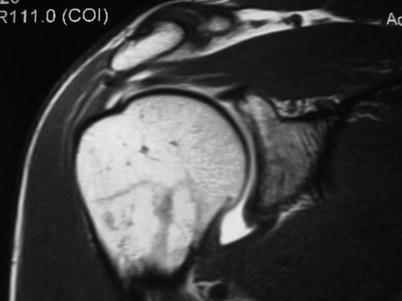
Fig. 15.2
Partial intra-articular rotator cuff tear. An MRI image
Consistent differentiation of tendinosis, partial-thickness tears, and full-thickness tears of the rotator cuff tendons is more difficult on non-enhanced MR images when no fluid is present in the joint cavity or in the bursa [28].
Partial-thickness tears or a horizontal splitting of the tendon beginning from the joint surface or the bursal surface is only detectable if there is fluid signal present in the defect or between the tendon layers. Frequently this fluid is absent, and sensitivity for partial-thickness tears of non-enhanced MR imaging of the shoulder is low.
Unfortunately partial-thickness tears originating from the bursal surface of the tendon are still missed, as long as there is no communication of the joint cavity with the bursa. MR arthrography can solve the problem of partial-thickness tears originating from the joint surface of the tendon.
Rotator Cuff Tears
Small full-thickness tears will enlarge over time. When the tear is only a few millimeters, the humeral head remains in place and keeps its relationship to the glenoid. In tears greater than 10 mm in diameter, the humeral head is slowly moved upward by those shoulder muscles, centering the humeral head underneath the coracoacromial arch.
In cases of massive tears, which exceed 20 mm in diameter, the infraspinatus tendon in addition to the supraspinatus tendon and, in rare cases, the subscapularis tendon become torn and insufficient. The humeral head migrates upward and finally articulates with the undersurface of the acromion.
Goutallier et al. [29] introduced the concept of fatty degeneration of the rotator cuff in 1989. They devised a staging system and noted that degeneration of the rotator cuff muscles was associated with rotator cuff tears.
In the initial iteration of the Goutallier staging system, axial CT was used to evaluate the supraspinatus, subscapularis, and infraspinatus muscles [30, 31]. The supraspinatus was evaluated on the axial image with the most muscle surface area (approximately 5 mm above the humeral head). The subscapularis and infraspinatus were evaluated superiorly at the level of the tip of the coracoid and inferiorly at the level of the lower glenohumeral joint. The muscles were then assigned a stage: Stage 0 is normal muscle. Stage 1 some fatty streaks. Stage 2 is less than 50 % fatty muscle atrophy. Stage 3 is 50 % fatty muscle atrophy. Stage 4 the fatty muscle atrophy is greater than 50 % (Fig. 15.3).
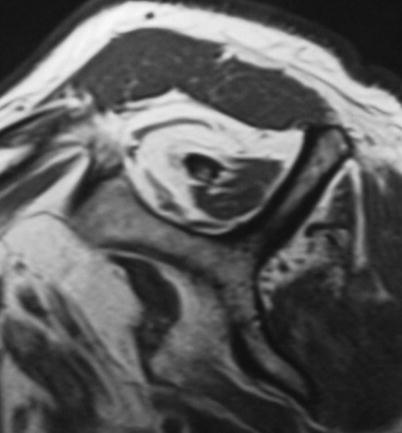
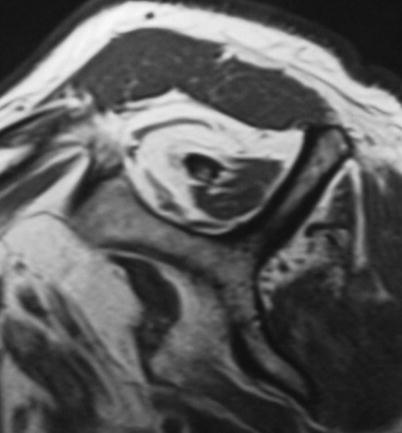
Fig. 15.3
Goutallier stage 4
Ultrasonography can be used as the primary diagnostic imaging modality for fatty changes in rotator cuff muscles.
Rotator cuff atrophy has generally been evaluated using either an occupation ratio, as described by Thomazeau et al. [32], or the tangent sign introduced by Zanetti et al. [33]. The occupation ratio was defined as the surface area supraspinatus muscle/surface area supraspinatus fossa [28]. The tangent sign is negative if the supraspinatus crosses a line between the superior aspect of the coracoid and the superior border of the scapular spine. MRI evaluation is performed using the most lateral image where the scapular spine is in contact with the body of the scapula [34].
Subscapularis Tears and Biceps Tendon Lesions
Lafosse et al. [35] proposed a subscapularis tear classification system based on CT findings and intraoperative assessment. Four types of subscapularis tendon lesions are described: Type I involves partial lesion of superior one-third of the subscapularis tendon. Type II involves complete lesion of superior one-third of the tendon. Type III tears represent complete lesion of superior two-thirds of the tendon rupture. Type IV are those with complete lesion of the tendon but head centered and fatty degeneration classified as less than or equal to Goutallier stage III.
Only 2 % of rotator cuff tears predominantly or exclusively involve the subscapularis tendon [36].
Imaging studies are also useful for evaluating subscapularis tears and concomitant shoulder pathology. Typically, routine radiographic evaluation is normal in the setting of a subscapularis tear. However, AP, outlet, and axillary lateral radiographs should be carefully assessed for anterior humeral head subluxation, proximal humeral head migration, and/or the presence of glenohumeral degenerative changes, all of which could indicate more chronic rotator cuff tear pathology.
Ultrasonography offers the ability for dynamic, noninvasive, real-time, and even bilateral comparison of the rotator cuff tendons. It is also less expensive than MRI. Ultrasound sensitivity increases with the size of the rotator cuff tear, reaching 100 % for massive full-thickness tears that involve the subscapularis.
CT arthrography, magnetic resonance arthrography, and routine MRI are commonly used to evaluate the subscapularis. On CT arthrography, extravasation of intra-articular contrast onto the lesser tuberosity is seen in the setting of an isolated subscapularis tear [37]. Also, it will show communication with air reaching from the glenohumeral joint to the bicipital groove. A medial dislocation of the biceps tendon is indicative of a complete rupture of the subscapularis tendon. Along with the coracohumeral and transverse humeral ligaments, which are parts of the rotator cuff interval, the subscapularis tendon is a major stabilizer of the long biceps tendon. Degeneration or disruption of the subscapularis tendon has been reported to be a common predisposing factor to medial dislocation of the biceps tendon [38, 39].
On MRI, in the presence of a tear of the subscapularis tendon, the contours of the tendon are poorly defined and of abnormally high signal intensity on T2-weighted images. Discontinuity and frank retraction is seen in 78 % of patients. Subscapularis tears are well detected in the sagittal oblique plane with the deltoid muscle seen in direct apposition to the anterior humerus and the lesser tuberosity [29].
Subscapularis tears are often missed on MRI. Complete and appropriate image sequencing, including T2-weighted axial images, parasagittal images, and the use of magnetic resonance arthrography, allows for improved detection of subscapularis tears [40–43].
Incomplete tears of the subscapularis tendon occur in conjunction with small- or medium-sized tears of the supraspinatus tendon. This combination is common in older patients, and most subscapularis lesions are incomplete tears on the articular side [44].
15.3 Instability
The glenohumeral joint is the most frequently dislocated major joint, and most cases involve an anterior dislocation. Glenohumeral instability is common in young athletes [45]. Athletes competing in contact sports are at especially high risk of recurrent instability [46, 47]. Almost half of all anterior shoulder dislocations occur in persons aged 15–29 years, and the incidence is nearly three times higher in males than in females [48]. This diagnosis encompasses a large spectrum of injury, from microinstability to glenohumeral dislocation. The imaging evaluation of an athlete with glenohumeral instability includes diverse modalities: radiography, CT, and MRI. Many missed dislocations result to an incomplete radiographic evaluation [25, 49, 50].
15.3.1 Shoulder Imaging Techniques
15.3.1.1 Radiography
X-ray evaluation is always recommended. Standard imaging of the shoulder should include a scapular AP view with the humerus in internal and external rotation as well as an axillary view of the shoulder. The contour of the anteroinferior glenoid should be readily visible on both the AP and the axillary views; a blurry or poorly defined contour suggests bone loss, especially in the setting of recurrent instability. Radiographs will also identify an associated Hill-Sachs lesion of the humeral head as well as greater tuberosity fracture or other associated fractures. Additional views that are particularly useful in assessing the unstable shoulder include the West Point axillary view, the Stryker notch view, and the Bernageau view. When X-rays are negative, more precise exploratory methods such as CT arthrography, MRI, or MR arthrography are usually indicated.
15.3.1.2 CT and CT Arthrography
Axial CT scans are helpful in determining the extent of glenoid bone loss and humeral head impaction. Accurate quantification of bone loss is often difficult to achieve. However, its efficiency seems to be improved by such technical refinements as helical acquisition, which enables high-quality multiplanar and three-dimensional (3D) reconstructions. Three-dimensional rendered images are preferred for defining the orientation and degree of glenoid bone loss and the extent of a Hill-Sachs lesion [26, 51, 52].
15.3.1.3 MRI and MR Arthrography
The value of MRI in shoulder disorders is continuously changing frequently due to the constant improvements of equipment and pulse sequences. MRI is very sensitive for confirming the clinical suspicion of a labral tear. MRI also identifies associated injuries to the rotator cuff and cartilage.
The image of the different anatomical structures of the shoulder varies according to the different pulse sequences used. The best results are usually obtained with the fast spin-echo moderately T2-weighted sequence associated with a fat suppression signal (Fat Sat). The echo train length must not be set too high in order to limit blurring artifacts.
Intra-articular gadolinium injection is used because of its usefulness in defining the extent of labral tears. This technique improves the analysis of the labrum, ligaments, and capsular structures as it increases intra-articular contrast and distends the capsule.
Two different techniques have been adopted [53]. Firstly, T1-weighted sequences are obtained after intra-articular gadolinium injection, diluted either with physiological serum or iodinated contrast media. This technique is widely used due to its excellent ability to detect articular abnormalities. In the second procedure, iodinated contrast media (or physiological serum) is injected solely and fast spin-echo T2-weighted sequences are obtained. The last method offers substantial advantages as it combines two widely used methods (arthrography and MRI) and does not require any complex manipulation of contrast media. It does not involve intra-articular gadolinium injection. Moreover, examinations are of high quality, and images are rapidly available. Finally, T2-weighted sequences used in this technique constitute the basis of shoulder exploration [54].
To put stress on the anteroinferior labrocapsular structures and therefore to obtain a higher definition of their lesions, acquisition with abduction and external rotation of the arm (ABER) or in the apprehension test position can be performed [54, 55]. ABER positioning is also recommended for exploring the painful athlete’s shoulder [18].
15.3.2 Imaging Findings in Instability
15.3.2.1 Anterior Instability
Unidirectional anterior shoulder instability usually begins with a discrete traumatic event. Imaging is fundamental in exploring instabilities.
In anterior instability, a standard X-ray evaluation is usually sufficient. The three anteroposterior views of the glenohumeral joint (external, neutral, and internal rotation), apical oblique view, and the Bernageau view (glenoid profile) are standard procedures.
In order to identify bony lesions, CT scan may eventually be used. CT arthrography or MRI gives more specific details as to the severity of the lesions, particularly soft tissue alterations.
In subtle forms of instability, diagnosis or instability direction is not clearly assessed clinically, and standard X-ray evaluation is usually normal. In this case, further imaging with CT arthrography, MRI, or MR arthrography are recommended to confirm the diagnosis of instability and to evaluate its direction. The technique of choice is undoubtedly MR arthrography; however, the imaging technique used depends mostly on several factors, principally quality, performance, and access to the machines.
15.3.2.2 Bony Lesions: Humeral Head Defect
Bony lesions associated with anterior instability are mainly represented by the Hill-Sachs lesion. Depending upon the direction of the displacement, the impaction may be observed higher or lower on the humeral head.
Reverse Hill-Sachs lesions are associated with posterior shoulder dislocation.
Humeral head defect is usually outlined by the anteroposterior (AP) view of the shoulder with the arm in internal rotation or by the apical oblique view [56]. Other less applied methods have been described such as the “Stryker notch view.”
CT scan or CT arthrographies are more efficient than the abovementioned methods to diagnose these abnormalities, as they are more efficient in detecting small bony defects. Finally, MRI is a valuable method to detect humeral head fractures, especially if performed shortly after the accident. These cases show bone marrow edema as well as the bony compression fracture at the posterolateral aspect of the humeral head. However, when bone marrow edema is no longer visible, small defects are less detectable with MRI than with CT scan.
15.3.2.3 Anteroinferior Lesions of the Glenoid Rim
The most common lesion is an anteroinferior capsulolabral avulsion from the glenoid rim [57, 58], typically with associated capsular attenuation. In addition, acute fracture and/or attritional glenoid bone loss may contribute to recurrent instability by altering the glenohumeral contact area and the function of the static glenohumeral restraints [59, 60].
In general, plain radiographs are moderately accurate at demonstrating glenoid bone loss [61]. A bony shadow or displaced bony Bankart fragment may be visualized on a standard AP view or in other projections parallel to the glenoid face, such as the axillary or glenoid profile view [62]. The highest yield projections, however, are angled relative to the glenoid face, such as the apical oblique [18]. The Stryker notch view and AP view with the humerus in internal rotation should also be obtained, given their utility in visualizing potential Hill-Sachs lesions on the humeral side [63].
Beyond standard radiography, MRI or magnetic resonance arthrography (MRA) studies may suggest the degree of bone loss in the most lateral glenoid cut on the sagittal oblique series. However, the current standard imaging modality for quantifying glenoid bone loss is CT.
Standard CT scans can be used to estimate bone loss and detect rim fracture fragments; Three-dimensionally reconstructed scans is the most reliable modality for predicting glenoid bone loss [64]. CT scan can also be performed with digital subtraction of the humeral head. By use of this modality, glenoid osseous deficiency is quantified as a percentage of the normal inferior glenoid surface area [65]. A best-fit circle is drawn on the inferior two-thirds of the glenoid image, which has been shown to be a consistent anatomic configuration [66]. The amount of bone missing from the circle, as a percentage of the total surface area of the inferior circle, is then determined with digital measurements.
15.3.2.4 Capsulolabral Detachments
The ALPSA (anterior labroligamentous periosteal sleeve avulsion) lesion is an avulsion of the anteroinferior glenoid labrum with an intact scapular periosteum. The ALPSA lesion differs from the Bankart lesion in that the ALPSA lesion has an intact anterior scapular periosteum allowing the labroligamentous structures to displace medially and rotate inferiorly on the scapular neck. In the Bankart lesion, the anterior scapular periosteum rupture results in displacement of the labrum and attached ligaments anterior to the glenoid rim.
CT arthrography, MRI, or MR arthrography can show different pathological patterns whose relationship with arthroscopic data can be difficult to establish. A fibrous scar may mimic an intact labrum on CT arthrography, and a wear and tear of the anteroinferior glenoid rim can be observed with a pseudo-intact labrum. In this case, MRI with intravenous gadolinium injection can show a tissue enhancement at the base of the pseudolabrum indicating the presence of fibrous tissues.
An irregular or severed anteroinferior recess is due to a fibrous scar and is usually well defined when the joint is filled with contrast media. Therefore, it can be demonstrated with CT arthrography or MR arthrography but is barely visible with MRI. A slight periosteal reaction is due to an extension of the tearing of the capsule at its insertion together with a periosteal tearing. This process is better observed with CT or CT arthrography.
The value of the different imaging methods in the diagnosis of labral tears remains controversial. The data obtained from different studies supports the use of indirect MRA as standard practice in patients with shoulder instability due to suspected labral pathology where further investigative imaging is indicated [67–69].
It is difficult to assess whether standard MRI is more efficient than CT arthrography, when their sensitivity and specificity vary, respectively, from 73 to 93 % and from 73 to 80 % [70]. Taking into account these large variations in accuracy, many authors advocate the use of MR arthrography as the most reliable method with a 95 % accuracy to evaluate labrocapsular structures and to detect labral tears [71].
Traumatic shoulder dislocation or subluxation may result in avulsion of the IGHL from its humeral attachment (HAGL lesion). Although both traumatic lesions occur with the arm in hyperabduction, HAGL lesions are more likely to occur with hyperabduction and external rotation [72]. HAGL lesions result in incompetence of the IGHL complex, which leads to glenohumeral instability, particularly in abduction and external rotation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






