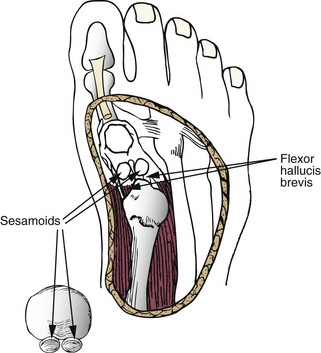
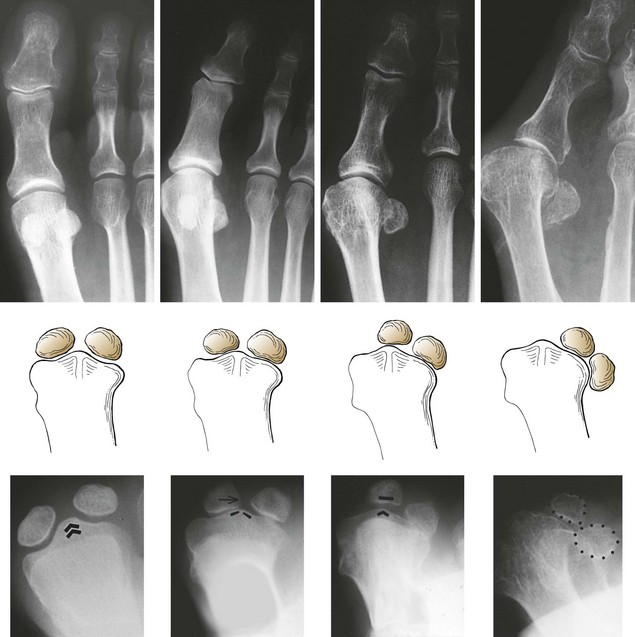
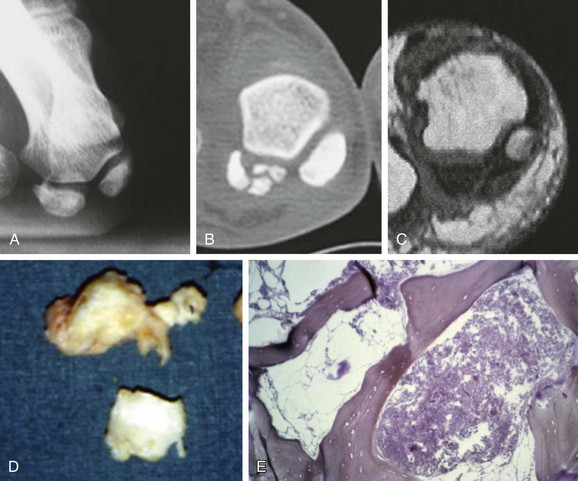
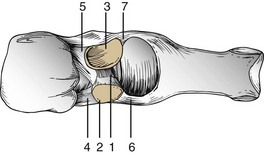
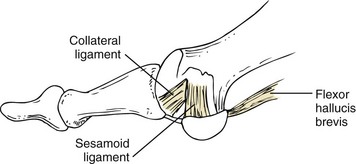
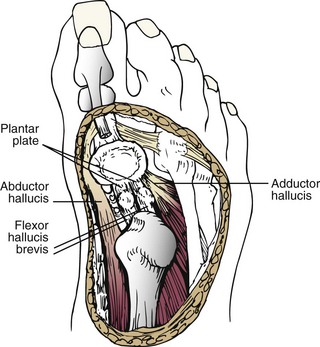
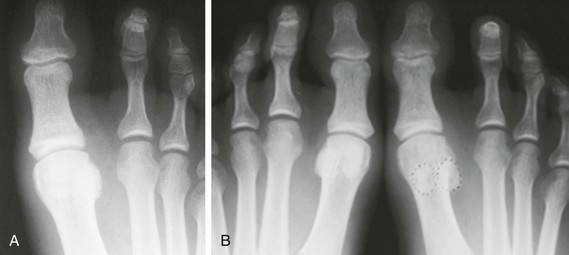
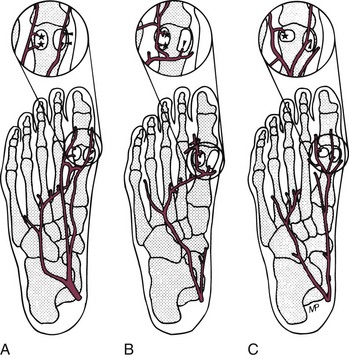
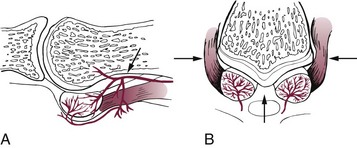
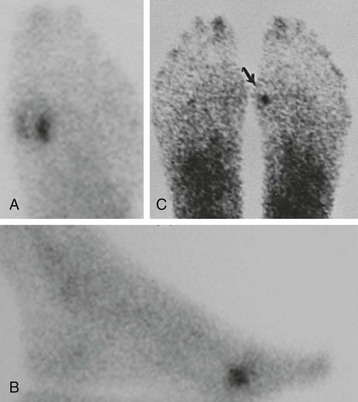
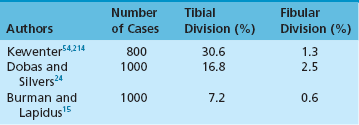
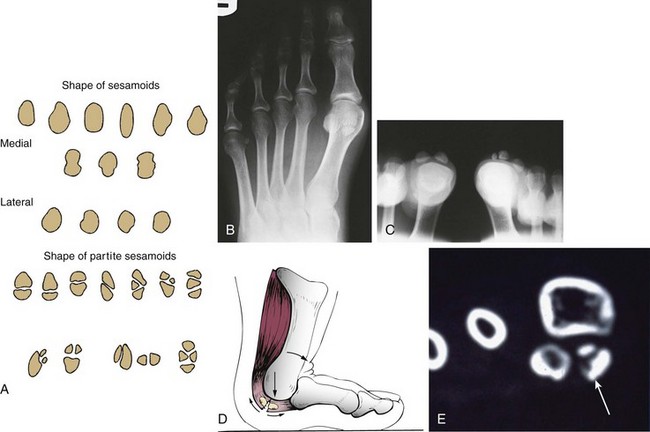
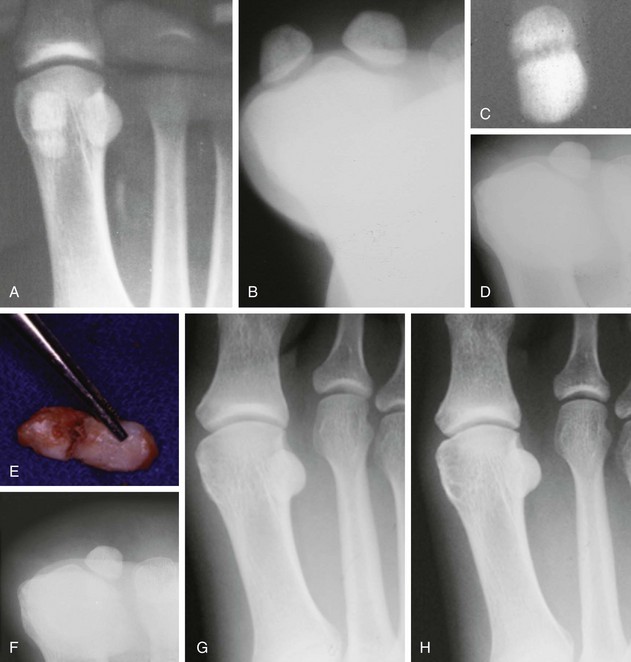
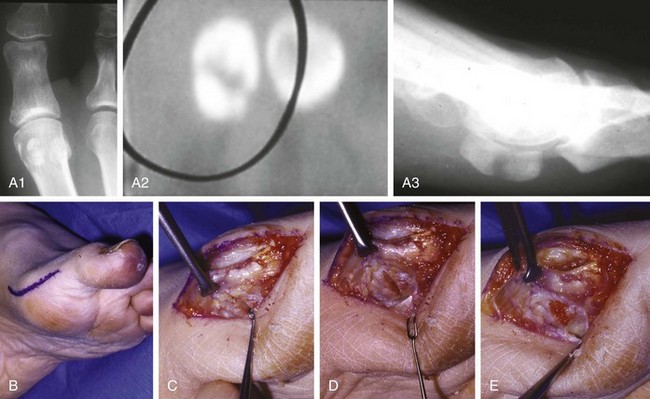
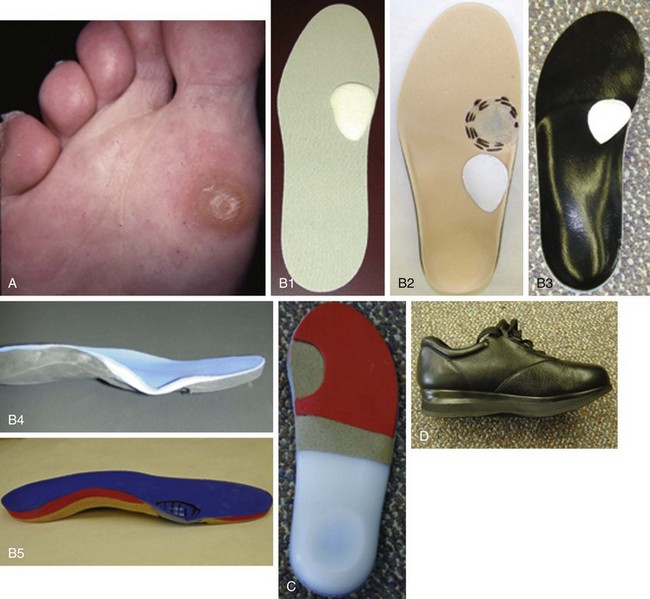
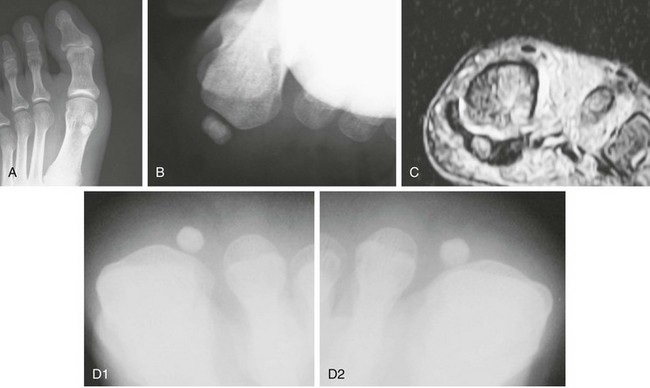
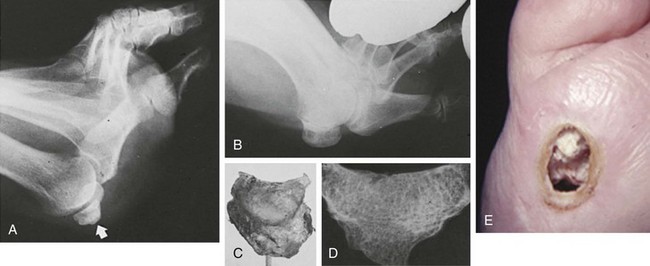
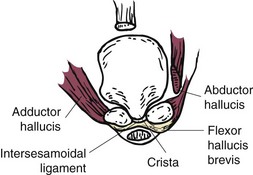
Chapter 10 SESAMOIDS OF THE FIRST METATARSOPHALANGEAL JOINT BIPARTITE SESAMOIDS AND FRACTURES CONGENITAL ABSENCE OF THE SESAMOIDS DISTORTED OR HYPERTROPHIED SESAMOIDS SUBLUXATION AND DISLOCATION OF THE SESAMOIDS OSTEOCHONDRITIS OF THE SESAMOIDS INTERPHALANGEAL SESAMOID OF THE HALLUX ACCESSORY BONES OF THE FOOT AND THE UNCOMMON SESAMOIDS SESAMOID OF THE TIBIALIS POSTERIOR TENDON SESAMOID OF THE TIBIALIS ANTERIOR TENDON OS SUBCALCIS AND OS APONEUROSIS PLANTARIS OS TALONAVICULARE DORSALE, OS SUPRATALARE OS CUNEO-I METATARSALE-I PLANTARE, OS CUNEO-I METATARSALE-II DORSALE Galen is reported to have first coined the term sesamoid because of the resemblance of these small rounded bones to the sesame seed.44 The anatomic location of several of the sesamoids is constant, but the frequency of occurrence of other sesamoids is quite variable.40 The sesamoids function to alter the direction of muscle pull, diminish friction, and modify pressure. Sesamoids occur in the substance of their corresponding tendon. They may be totally or partially contained within the tendinous structure. Some sesamoids totally ossify, some remain entirely cartilaginous, and some partially ossify with a fibrocartilaginous interface between the ossified fragments. This variability in ossification might explain the radiographic absence or presence of various sesamoids, as well as the incidence of bipartism of sesamoids.91 The sesamoid mechanism and intrinsic musculature of the hallux differentiate the first ray from the lateral toes. The hallucal sesamoids, enveloped within the double tendon of the flexor hallucis brevis (Fig. 10-1), articulate on their dorsal surface with the plantar facets of the first metatarsal head. A crista, or intersesamoid ridge (Fig. 10-2), separates the medial and lateral metatarsal facets. This intersesamoid ridge provides intrinsic stability to the sesamoid complex. In severe cases of hallux valgus, with substantial subluxation of the sesamoid complex in relation to the first metatarsal head, the intersesamoid ridge atrophies and at times is obliterated (Fig. 10-3). Close inspection of the plantar articular surface of the first metatarsal frequently reveals substantial cartilage erosion and degenerative arthritis in this area (Fig. 10-4).10 Figure 10-2 A cross section of the first metatarsal head demonstrates the sesamoid and the intersesamoidal ridge. The sesamoids are connected to the plantar base of the proximal phalanx through the plantar plate (Fig. 10-5), which is an extension of the flexor hallucis brevis tendon. The inferior surface of the sesamoids is covered by a thin layer of the flexor hallucis brevis tendon, whereas the superior surface is articular in nature. These sesamoids are entirely intratendinous, except dorsally, where they articulate with the first metatarsal head. The sesamoids are suspended by a slinglike mechanism composed of the collateral ligaments of the MTP joint and the sesamoid ligaments (Fig. 10-6) on both the medial and lateral aspects of the MTP joint. The flexor hallucis brevis, through its sesamoid mechanism, provides a significant plantar flexion force at the MTP joint. The sesamoids also have an insertion into the joint capsule and the plantar aponeurosis; this provides both stabilization and a static plantar flexion force at the MTP joint. On the medial aspect of the MTP joint, the abductor hallucis tendon (Fig. 10-7) inserts into the plantar-medial base of the proximal phalanx as well as the medial sesamoid and functions to stabilize the sesamoid mechanism medially. On the lateral aspect, the adductor hallucis tendon inserts into the lateral base of the proximal phalanx and into the lateral sesamoid to stabilize the sesamoid mechanism laterally. The medial and lateral sesamoids are connected by the intersesamoidal ligament, which forms the base of the tendinous canal enveloping the tendon of the flexor hallucis longus. Distal to the sesamoids, the phalangeal-sesamoid ligament is a thin-layered structure that interdigitates with the collateral ligaments, extension of the plantar aponeurosis, and tendons of the flexor hallucis brevis to form the plantar plate. These structures are not individually distinguishable but, rather, coalesce to form the plantar plate. Complete or partial rupture of the plantar plate attachement may lead to a turf toe deformity with retraction of the sesamoids, restricted motion, and degenerative arthritis of the first metatarsophalangeal joint.18 When a person is in a standing position, the sesamoids are located posterior to the metatarsal head; however, with dorsiflexion of the hallux, the sesamoids move distally, thereby protecting the otherwise exposed plantar surface of the first metatarsal head. When a person rises onto the toes, the sesamoids (especially the medial sesamoid) act as the main weight-bearing focus for the medial forefoot (Fig. 10-8). Kewenter54,214 noted that the medial sesamoid is located slightly more distal than the lateral sesamoid and is slightly larger. Orr73 quantitated sesamoid size and reported that the tibial sesamoid averaged 9 to 11 mm in width and 12 to 15 mm in length. The fibular sesamoid was noted to have an average width of 7 to 9 mm and an average length of 9 to 10 mm. Although ossification of the hallucial sesamoids is variable, Kewenter reported that ossification usually occurs between the sixth and seventh years. Ossification of the sesamoids often occurs from multiple centers, and this may be the reason for the development of multipartite sesamoids.54,214 The arterial anatomy of the first ray was evaluated in 22 anatomic specimens by Rath et al.78 They found that the first plantar metatarsal artery provided the main arterial supply to the medial and lateral sesamoids. It anastomosed with a branch of the medial plantar artery in 90% of cases they dissected. They demonstrated both proximal and distal vessels branching off the two major arteries. Pretterklieber and Wanivenhaus,77 in dissections of 29 cadavers, reported three different types of arterial circulation. The most common type (type A, 52%), was characterized by arterial circulation derived from the medial plantar artery and the plantar arch. In the less common types, circulation was derived mainly from either the plantar arch or only from the medial plantar artery (Fig. 10-9). Both authors concluded that the course and distribution of the arterial circulation to the sesamoids might have a significant bearing on the development of avascular necrosis after injury and possible inadvertent injury during surgical exploration of this area. The number of arterial branches can affect healing of fractures as well as the incidence of avascular necrosis after trauma.13 Multiple arterial branches can protect an injured sesamoid, whereas a single arterial branch to a damaged sesamoid may be interrupted by a fracture or injury and lead to delayed healing or a nonunion. Sobel et al97 and Rath et al,78 in their evaluation of sesamoid vascularity, mapped the vascular supply as well of both the medial and lateral sesamoids. The major vascular supply enters the sesamoids from the proximal and plantar aspect, with a minor arterial supply entering through the distal pole of the sesamoids (Fig. 10-10A). The distal vascular supply originates through distal capsular attachments providing, in most cases, a limited arterial supply. The proximal arterial supply, through the flexor hallucis brevis, supplies one third to two thirds of the proximal sesamoid. Vascular anastomoses occur between the proximal supply and that derived from the plantar surface to the body of the sesamoid (Fig. 10-10B). The distal portion of the sesamoid has the most tenuous vascular supply, and this can lead to delayed or unsuccessful healing after injury. The orientation of the hallux must be inspected for lateral (hallux valgus) or medial (hallux varus) deviation or for clawing of the hallux. Progressive insidious deviation of the hallux can develop with sesamoid disruption caused by trauma or fracture. Progressive hallux valgus or hallux varus can also develop as a result of a previous sesamoid resection. Hyperextension of the hallux because of discontinuity of the sesamoid complex can occur after traumatic rupture of the plantar plate (see Fig. 10-8). Examination of the sensory nerves of the first ray is important in diagnosing a compressed digital nerve,39 which can manifest with isolated neuritic symptoms or numbness. With compression of either the medial or lateral digital nerve by either the tibial or fibular sesamoid, a Tinel sign can be elicited along the border of the sesamoid. Routine dorsoplantar and lateral radiographs (Fig. 10-11A and 10-11B) can provide limited information in the evaluation of a painful sesamoid. On the dorsoplantar view, the metatarsal head overlies both the medial and lateral sesamoid and often obscures detail; on the lateral projection, the medial and lateral sesamoids overlap each other. The fibular sesamoid is best demonstrated in a lateral oblique radiograph (Fig. 10-11C), where it can be seen between the first and second metatarsal heads. The tibial sesamoid is best seen on a medial oblique radiograph (Fig. 10-11D).81 With the MTP joint dorsiflexed approximately 50 degrees, the roentgen beam is directed 15 degrees cephalad from a lateral position and is centered over the first metatarsal head. Often, however, the most useful radiograph is the axial sesamoid view (Fig. 10-11E).43,63 Where radiographs appear normal in spite of a patient’s subjective symptoms, a technetium-99m (99mTc) bone scan may be useful (Fig. 10-12A, B, and C). A bone scan can demonstrate increased uptake before the development of any significant radiographic change, such as sclerosis, fragmentation, or disintegration. Computed tomography (CT) examination can define osseous changes, such as acute fracture or fragmentation, and magnetic resonance imaging (MRI) examination may demonstrate bone edema, avascular regions, fragmentation or degeneration of a sesamoid early before radiographic changes are demonstrated on plain radiographs (see Fig. 10-4A). The incidence of partite sesamoids as well as their cause has been the subject of substantial discussion in the literature (Table 10-1). Kewenter54,214 examined 800 feet and found a 31% incidence of bipartite tibial sesamoids (Fig. 10-13), and Dobas and Silvers24 examined radiographs of 1000 feet and found a 19% incidence of combined tibial and fibular sesamoid bipartism (Fig. 10-14). Dobas and Silvers reported that 80% of bipartite sesamoids involve the tibial sesamoid. Rowe87 noted a 6% to 8% frequency of bipartite sesamoids and stated that 90% of these were bilateral. Dobas and Silvers24 stated that approximately 25% of partite tibial sesamoids had an identical bipartite tibial sesamoid on the contralateral side, whereas the remaining sesamoids were asymmetric when division was concerned. Jahss46 noted that bipartism was 10 times more common in the medial sesamoid. Giannestras32 stated that the occurrence of bipartite sesamoids was typically symmetric, but this is obviously not the case. The medial sesamoid is often divided into two, three, or four parts, whereas the lateral sesamoid is rarely divided into more than two parts (Fig. 10-15). Figure 10-14 Anteroposterior radiograph demonstrating asymptomatic bipartite medial and lateral sesamoids. Inge and Ferguson44 reported that 85% of the bilateral partite sesamoids had asymmetric divisions. They also reported that the incidence of division decreased with time, thus implying that osseous union occurs with time in the divided sesamoid. They further reported that histologic evaluation of congenital bipartite sesamoids demonstrated that articular cartilage tended to dip down between the two osseous fragments. This can predispose a bipartite sesamoid to fracture or disruption of the synchondrosis with minimal injury (see Fig. 10-13D). They speculated that the medial sesamoid has a higher frequency of bipartism than the lateral sesamoid because it is more often traumatized, a result of its greater weight-bearing capacity. It has not been determined whether continued trauma with ambulation prevents the union of divided sesamoids or whether some of these partite sesamoids are actually nonunions of fractures. The incidence of irregular ossification with bipartism in the medial sesamoid is well recognized. Kewenter54,214 examined a series of sesamoids in cadavers and found that congenitally divided sesamoids fracture with much less force than normal sesamoids when experimental trauma was introduced. Although fractures of sesamoids are relatively rare, numerous cases have been reported in the literature.* Substantial trauma with MTP joint dislocation and simultaneous fractures of both sesamoids have been reported23,103; in general, the most frequently reported mechanism of injury is a fall onto the forefoot, sudden loading of the forefoot, or a crush injury. It can be difficult to distinguish between a fractured sesamoid (see Fig. 10-15) and a symptomatic bipartite sesamoid.30,104 With a divisionary line between two segments of a sesamoid, a careful physical examination and history must be correlated with radiographic findings to differentiate between a partite sesamoid and a superimposed fracture.30 With a sesamoid fracture, pain is localized to the region of the specific sesamoid. Symptoms are typically exacerbated with ambulation and reduced with rest. Often, the patient ambulates with weight bearing on the lateral aspect of the foot to avoid motion and loading of the sesamoid complex. On physical examination, forced passive dorsiflexion and plantar flexion can cause discomfort. Synovitis or nonspecific swelling on the plantar aspect of the sesamoid complex may be observed. The development of pain after minimal trauma in the presence of a bipartite sesamoid should alert the examiner to the possibility of a superimposed fracture of a bipartite sesamoid. An acute fracture may be noted on a radiograph with a sharp radiolucent line (Fig. 10-16); however, Inge and Ferguson44 suggested that a fracture should not be diagnosed unless callus is present. Delay in diagnosis of a sesamoid fracture is therefore common because of the difficulty of confirming the fracture by radiography.102,110 Although rarely is a preinjury film available to help differentiate a partite sesamoid and a fracture, increased separation between fragments can be a definitive finding in the presence of a disruption of a partite sesamoid (Fig. 10-17). Richardson81 recommends a bone scan to aid in diagnosis of a fracture in the presence of a bipartite sesamoid. MRIs may demonstrate increased vascularity, bone edema, or acute changes, indicating a disruption of a partite sesamoid49 (see Fig. 10-37D). Hobart40 recommended non–weight bearing and casting until the sesamoid fracture had healed, which usually occurred in 6 to 8 weeks (Fig. 10-18). Anderson and McBryde2 reported on 21 patients treated with bone grafting for symptomatic tibial sesamoid nonunions (Fig. 10-19). They curetted and bone grafted the diastasis, which was typically 1 mm wide. All patients were noted to have a positive bone scan before surgery. In two cases in which articular surface deterioration was noted, a sesamoidectomy was performed. Three other patients had excessive motion at the diastasis site and were not considered candidates for bone grafting. Through an inferior extraarticular approach, they curetted and bone grafted the diastasis “nonunion site.” No internal fixation was used. The patients were placed in a below-knee cast and kept non–weight bearing for 4 weeks. At final follow-up, 19 of 21 sesamoids had healed. Two patients had a persistent nonunion. Reports in which internal fixation has been used for acute sesamoid fracture75 or chronic nonunions9,82 have noted success. Riley and Selner82 used a circlage wire and bone grafting in one case, and Blundell et al9 used a percutaneous screw in nine cases and reported successful union. Pagenstert et al75 reported two cases in which simultaneous correction of a hallux valgus deformity was combined with open reduction and internal fixation of a nonunion of a medial sesamoid. Rodeo et al83 reported on four cases of injuries to the hallux with progressive diastasis of bipartite sesamoids. The patients were treated with a distal resection of a smaller fragment and repair of the sesamoid mechanism. Biedert and Hintermann7 reported on five athletes who developed stress fractures of the medial sesamoids. Surgical excision of the proximal fragment and repair of the flexor hallucis brevis were performed. After casting for 6 weeks after surgery, full return to sports activity was allowed at 8 weeks. Kuo et al57 reported a case of nonunion of the fibular sesamoid in association with chronic gout that required surgical excision. Brodsky et al13 retrospectively reviewed a series of 37 patients with fractured sesamoids. Avascular necrosis secondary to fracture was noted in 9 cases, 16 cases were diagnosed as stress fractures, and 12 cases were related to direct trauma. After surgical excision of the fractured sesamoid, an average postoperative American Orthopaedic Foot and Ankle Society (AOFAS) score of 93 was achieved. Saxena and Krisdakumtorn93 reported on 24 patients at a mean follow-up of 86 months after sesamoidectomy. There were 10 fibular and 16 tibial sesamoidectomies. Eleven patients were professional or varsity athletes and returned to activity in 7.5 weeks. The other patients returned to normal activities in 12 weeks. Complications included one varus deformity, one valgus deformity, and two cases of neuroma formation associated with fibular sesamoidectomy. Patients took longer to recover from surgery for tibial sesamoidectomy, which the authors surmised was probably due to increased weight bearing. Patients with fibular sesamoidectomies had an earlier return to activity. They noted that a dorsolateral approach may be more difficult for fibular sesamoidectomy and that the two nerve problems both occurred with a dorsolateral approach. Custom and prefabricated orthotics and scaphoid and metatarsal pads can relieve pressure in the sesamoid region, diminishing symptoms. Taping of the toe to reduce dorsiflexion can also relieve symptoms. If conservative methods fail, surgical removal of the involved sesamoid may be necessary (see Fig. 10-20). Rosenfield and Trepman85 have described the use of a rocker-soled walking shoe with a full-length steel shank. An orthotic insole is added with a recess beneath the sesamoid region (Fig. 10-21). Congenital variations in regard to ossification of the tibial and fibular sesamoids are common. Congenital absence of a sesamoid has been infrequently reported; however, it is probably more prevalent than is realized.48,58 Patients are typically asymptomatic with absent sesamoids. Inge and Ferguson44 reported two cases of congenital absence of the tibial sesamoid. Goez and DeLauro,35 Zinsmeister and Edelman,111 and others21,52 have reported absence of the tibial sesamoids as well. Jeng et al48 and others60,108 have reported cases of an absent fibular sesamoid (Fig. 10-22). Although absence of a sesamoid can be asymptomatic, removal of a sesamoid for painful plantar keratosis can cause postoperative pain beneath the remaining sesamoid. The absence of a tibial sesamoid can produce a clawing of the hallux or development of a progressive postoperative hallux valgus deformity (see Fig. 10-22D).35,108 Jahss47 has reported that congenital absence of both sesamoids is extremely rare (Fig. 10-23DE). Wright107 reported one case of bilateral absence of both sesamoids associated with hallux varus deformity, and Williams et al106 reported a case of bilateral congenitl absence with associated metatarsalgia (Fig. 10-23A, B, and C). Congenital variations of the sesamoids can lead to localized discomfort if the plantar surface of the sesamoid is irregular. Hypertrophy of a sesamoid can create an extraordinarily large or thickened projection on the plantar surface and lead to development of a hyperkeratotic lesion (Fig. 10-24). Mowad et al70 described an osteochondroma of the tibial sesamoid manifesting with a painful plantar mass and a hypertrophic plantar keratosis (Fig. 10-25A and B).
Sesamoids and Accessory Bones of the Foot
Sesamoids
Sesamoids of the First Metatarsophalangeal Joint
Anatomy
Location, Function, and Size
Ossification
Circulation
Preoperative Evaluation
Physical Examination
Radiographic Examination
Bipartite Sesamoids and Fractures

Congenital Absence of the Sesamoids
Distorted or Hypertrophied Sesamoids
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine