Abstract
Objectives
To describe the frequency with which members of the French general population in the 30-to-69 age class sought care for lower back pain (LBP) from various healthcare professionals and to identify associated parameters.
Material and methods
Data were collected in the 2002–2003 Décennale Santé survey, which is representative of ordinary households in continental France. We assessed the frequency with which the 17,792 surveyed individuals sought care for LBP by considering consultations with healthcare professionals in general and consultations with general practitioners and physiotherapists in particular.
Results
Among the survey subjects, 4.5% reported that they had sought treatment for LBP from a healthcare professional at least once during the 2-month survey period. The decision to seek care was correlated with the characteristics of the LBP. The duration of the pain was associated with the frequency of all types of consultation studied here. Sociodemographic, economic and occupational risk factors were also involved. Consultation with a physiotherapist was related to income.
Conclusion
These results from a representative sample of the French general population show that the factors associated with seeking treatment for LBP differ according to the type of healthcare professional consulted.
Résumé
Objectifs
Décrire la fréquence du recours aux soins pour lombalgie dans la population française de 30 à 69 ans et mettre en évidence les facteurs associés.
Matériel et méthodes
Les données sont issues de l’enquête Décennale santé 2002–2003, enquête représentative des « ménages ordinaires » résidant en France métropolitaine. La fréquence du recours aux soins pour lombalgie a été étudiée parmi les 17 792 personnes enquêtées. Trois types de recours ont été considérés : le recours à un professionnel de santé (en général), à un médecin généraliste et à un kinésithérapeute.
Résultats
Dans cette étude, 4,5 % des personnes déclarent avoir eu recours au moins une fois à un professionnel de santé pour lombalgie sur la période d’étude (deux mois). Le recours aux soins est associé à des critères de sévérité de la lombalgie telle que la durée de la lombalgie qui est associée à tous les types de recours étudiés. Des facteurs sociodémographiques, économiques et des facteurs d’exposition professionnelle interviennent également. Le revenu est lié au recours au kinésithérapeute.
Conclusion
Ces premiers résultats sur l’ensemble de la population française montrent que les facteurs associés aux recours aux soins pour lombalgie diffèrent selon le type de recours.
1
English version
1.1
Introduction
The frequency and the socioeconomic repercussions of lower back pain (LBP) constitute a major public health problem in France (as in most industrialised countries).
The direct cost of medical treatment for LBP in France was estimated at € 1.4 billion (1.6% of healthcare expenditure) in the 2003 GTNDO/INSERM report for the French government .
A French study of data from the 2002–2003 Décennale Santé survey provided an estimation of the frequency of LBP in the general population aged from 30 to 64 . The prevalences of LBP “for at least one day in the previous 12 months” and “for over 30 days in the previous 12 months” were 55% and 17%, respectively.
These high observed values prompt the following questions: which is the frequency of care seeking for LBP and which factors are linked to the decision to seek care or not?
Several surveys performed in various countries have sought to answer this question . A study performed in the Netherlands (based on an interview and examination of medical records for a population of over 25 years) found that the majority of LBP sufferers did not seek treatment . Although 13% percent of the population stated having sought treatment for LBP in the previous year, the percentage having actually consulted (according to medical records) was only 8.9%. Furthermore, in a phone study performed by Carey et al. in North Carolina, 7.6% of the survey population stated having experienced at least one episode of acute LBP over a one-year period . Only 39% of the LBP sufferers had actually sought care for this condition from a healthcare professional.
To the best of our knowledge, the frequency with which the French general population seek care for LBP and the factors associated with this decision have not been investigated.
The goal of the present study was to describe the frequency which with individuals sought treatment for LBP over a 2-month period (corresponding to the duration of the survey) and the types of healthcare professional consulted and to identify the factors associated with the decision to seek care.
1.2
Material and methods
1.2.1
The survey
In the French nationwide Décennale Santé survey performed in 2002–2003, the sample comprised 16,449 households and a total of 40,867 individuals. The target population consisted of “ordinary households” in continental France and excluded communities (such as retirement homes, student residences, hostels, etc.).
The survey included three interviews (performed by specially trained staff) and a self-questionnaire, which notably included a French-language version of the LBP-specific Nordic questionnaire and the SF-36 questionnaire .
The survey data enable the individuals’ sociodemographic and economic characteristics to be cross-correlated against their healthcare status and health care consumption.
1.2.2
Study population
The study population was constituted by all the subjects in the 30 to 69 age category in the 2002–2003 Décennale Santé survey who were able to complete the self-questionnaire and had participated in the three face-to-face interviews with survey staff, i.e., a total of 17,792 people (8,403 men and 9,389 women).
We excluded 210 people unable to complete the self-questionnaire and 5,723 people who did not participate in all three face-to-face interviews.
The 30–69 age category was chosen in order to take account of the subjects’ professional status and in view of the known relationship between age and LBP, since LBP-related factors probably change beyond a certain age.
1.2.3
Variables describing LBP
In the present study, the main healthcare variable was consultation with a specified healthcare professional for LBP at some point during the 2-month survey period. We considered that a subgroup of survey subjects was more likely to seek care from healthcare professionals for LBP: those who had reported the presence of LBP in the previous 12 months in the self-questionnaire and those who had spontaneously mentioned LBP as a chronic healthcare problem during the interview. Three variables were used to characterize the severity of LBP in these subjects: its duration over the 12 months examined by the self-questionnaire, the pain site (sciatic radiation to the legs, etc.) and the SF-36 Physical Functioning score.
1.2.4
Other parameters taken into account
Of the many variables recorded during the Décennale Santé survey, we selected three categories in view of the literature in this field and our starting hypotheses (particularly with respect to potential geographic disparities):
- •
sociodemographic and economic variables: gender, age, highest degree or qualification, marital status, living alone or not, income per unit of consumption, socioprofessional category (SPC), receipt of “minimum guaranteed income” state benefits (RMI), full public health insurance coverage (CMU), private health insurance cover, geographical region (ZEAT), the number of inhabitants in the locality of residence and, lastly, residency in a deprived area (ZUS) ;
- •
individual variables: height, weight, body mass index (BMI, calculated as weight/[height] 2 ) and the SF-36 Mental Health score ;
- •
variables related to occupational exposure as noted on the self-questionnaire: carrying heavy loads during work, uncomfortable and tiring work.
1.2.5
Statistical methods
Our statistical analyses were performed separately on men and women; most analyses were restricted to the sub-group of subjects who were likely to seek care from a healthcare professional for LBP, i.e. those who had actually reported LBP.
First, univariate analyses were performed in order to study potential associations between consultation with a healthcare professional (physiotherapists and/or physicians) and the selected variables. We also sought to identify any factors related specifically to consultation with a general practitioner (GP) or with a physiotherapist (regardless of whether or not other healthcare professionals were also consulted).
In a second step, the individuals having reported LBP in the 12 months (in the self-questionnaire or spontaneously during the survey interview) were analyzed in stepwise backward multivariate logistic regression models by incorporating the significant ( p < 0.05) variables from the univariate analysis and for all three types of consultation (healthcare professionals in general, GPs and physiotherapists).
Significant variables ( p < 0.1) and age were included in the final models. This approach means that the variables included in the final models (and thus the adjustment factors) may differ for men and women. Variables significant at the p < 0.1 level but not the p < 0.05 level in the final model can be considered to be adjustment variables (like age).
In view of the results of a preliminary analysis and as briefly explained in the discussion, we decided to present results that do not take account of the ZEAT regional variable. In fact, this variable was significantly associated with the three types of consultation for both genders. However, no one region stood out clearly and the results were very difficult to interpret. Furthermore, our other findings were not affected by inclusion or non-inclusion of the ZEAT variable.
All statistical analyses were performed with SAS software, version 9.1 (SAS Institute Inc, Cary, NC, USA).
1.3
Results
1.3.1
Frequency of lower back pain and seeking care
Of the 17,792 individuals in the survey as a whole, 44.9% stated (either in the self-questionnaire or spontaneously during the interview) that they had suffered from LBP in the previous 12 months.
A total of 808 subjects (4.54%) said that they had sought care from a healthcare professional for LBP at least once during the 2-month period (962 medical consultations and 245 consultations with a physiotherapist).
By restricting the analysis to the 8,792 individuals having stated (in the self-questionnaire or spontaneously) that they had suffered from LBP in the previous 12 months, nearly 9.19% stated that they had sought care for the condition from a healthcare professional at least once over the 2-month survey period.
1.3.2
The medical specialties of the physicians consulted for lower back pain
GP accounted for 77% of the 962 medical consultations for LBP ( Fig. 1 ). The second most consulted medical specialty for LBP was rheumatology (9%). Surgeons accounted for the third most consulted specialty for LBP, with nearly 3% of the total. Each of the other specialties corresponded to just a few consultations.

1.3.3
Factors associated with consultation for lower back pain
1.3.3.1
Consultation with a healthcare professional
Table 1 presents the factors associated with seeking care from at least one healthcare professional (a physician or a physiotherapist) for LBP in each gender. Subjects having reported a consultation for LBP during the 2-month survey period were compared with those who had reported LBP in the previous 12 months (in the self-questionnaire or during the interview) but had not consulted for the condition.
| Men ( n = 363 vs n = 3622) | Women ( n = 445 vs n = 4362) | |||
|---|---|---|---|---|
| Variables | OR | p | OR | p |
| Age | ns | ns | ||
| Health insurance | 0.0406 | |||
| Minimal insurance coverage | Reference | |||
| Private health insurance or CMUC | 1.6 | 0.0522 | ||
| Carrying heavy loads at work | 0.0716 | |||
| No | Reference | |||
| Yes | 1.1 | 0.3152 | ||
| Unknown | 0.7 | 0.0953 | ||
| Duration of Low Back Pain (in a 12 month period) | < 0.0001 | < 0.0001 | ||
| 1 to 7 days | Reference | |||
| 8 to 30 days | 1.7 | 0.0055 | 2.7 | < 0.0001 |
| More than 30 days but not everyday | 3.6 | < 0.0001 | 4.0 | < 0.0001 |
| Everyday | 5.1 | < 0.0001 | 5.7 | < 0.0001 |
| Unknown duration | 4.5 | < 0.0001 | 2.6 | 0.0054 |
| Type of pain | 0.0001 | < 0.0001 | ||
| Other type of low back pain | Reference | |||
| Sciatica, pain radiating above the knee | 2.0 | < 0.0001 | 2.3 | < 0.0001 |
| Acute low back pain | 1.1 | 0.5601 | 1.3 | 0.1991 |
| Sciatica, pain radiating below the knee | 1.2 | 0.2756 | 1.7 | 0.0003 |
| Unknown | 0.5 | 0.0380 | 1.1 | 0.7439 |
| SF36 Physical functionning score | 0.0014 | 0.0200 | ||
| >95 | Reference | |||
| < 80 | 2.0 | 0.0001 | 1.7 | 0.0023 |
| ≥ 80 and ≤ 95 | 1.4 | 0.0306 | 1.3 | 0.0852 |
| Unknown | 1.8 | 0.1164 | 1.5 | 0.2477 |
| Income per unit of consumption (in euros) | 0.0520 | |||
| < 7345.295 | Reference | |||
| > 7345.295 and < 14690.59 | 1.5 | 0.0610 | ||
| > 14690.59 | 1.6 | 0.0196 | ||
The two models were adjusted for age. The model for men included the presence of private health insurance, whereas the final model for women included income and exposure to carrying heavy loads at work.
1.3.3.1.1
In men
The longer the duration of LBP in the previous 12 months, the more likely subjects were to consult with a healthcare professional: a man suffering from LBP every day was about five times as likely to consult as one who had suffered from LBP for 1 to 7 days.
When compared with “other types of LBP”, the “sciatica not radiating below the knee” category of the “pain site” variable was also linked to seeking care for LBP (odds ratio [OR]: 2.0; 95% confidence interval [CI]: [1.4–2.8]). The other pain sites were not significantly associated with consultation.
A lower SF-36 Physical Functioning score (i.e. greater functional disability) was associated with a greater likelihood of at least one consultation with a healthcare professional. Relative to men with a good (above-median) SF-36 Physical Functioning score (i.e. low functional disability), men with a score in the lowest quartile were twice as likely to consult (OR: 2.0; CI: [1.4–2.8]).
1.3.3.1.2
In women
Women from households in which the annual income per unit of consumption was above € 14,690 consulted a healthcare professional more frequently than those with an annual income per unit of consumption below € 7,345; the higher the income, the greater the probability of consultation.
As was seen for the men, the probability of consulting a healthcare professional increased with the duration of LBP. Women suffering from LBP every day were almost six times as likely to consult a healthcare professional than those having suffered from LBP for 1 to 7 days in the previous 12 months (OR: 5.7; CI: [3.9–8.3]).
Compared with other types of LBP, sciatic pain (regardless of whether or not it radiated below the knee) doubled the frequency of consultation with a healthcare professional (OR sciatic pain not radiating below the knee : 2.3; CI: [1.7–3.2]; OR sciatic pain radiating below the knee : 1.7; CI: [1.3–2.2]).
As was seen for the men, a lower SF-36 Physical Functioning score was associated with a higher probability of seeking care. A woman with a score in the lowest quartile (i.e. many functional physical disabilities) was nearly twice as likely to consult for LBP as one with an above-median score (i.e. optimal physical function) (OR: 1.7; CI: [1.2–2.3]).
1.3.3.2
Consultation with a general practitioner
Table 2 presents the factors associated with consultation with a GP for LBP in men and in women. Subjects who reported consulting a GP for LBP during the 2-month study period (regardless of whether or not they had also consulted one or more other types of health professional) were compared with those who had reported LBP in the previous 12 months (in the self-questionnaire or spontaneously in an interview) but had not consulted a GP. In women, the final model was adjusted for occupational exposure to carrying heavy loads, as well as age.
| Men ( n = 263 vs n = 3722) | Women ( n = 295 vs n = 4512) | |||
|---|---|---|---|---|
| Variables | OR | p | OR | p |
| Age | ns | 0.0996 | ||
| 30–39 years | Reference | |||
| 40–49 years | 1.0 | 0.8595 | ||
| 50–59 years | 1.0 | 0.8223 | ||
| 60–69 years | 0.7 | 0.0500 | ||
| Diploma | 0.0440 | |||
| No diploma or unknown | Reference | |||
| Primary or primary + 4 years (general) | 0.9 | 0.6172 | ||
| Basic vocational training | 0.8 | 0.1802 | ||
| Medium | 0.7 | 0.0873 | ||
| University level | 0.5 | 0.0051 | ||
| Carrying heavy loads at work | 0.0506 | |||
| No | Reference | |||
| Yes | 1.2 | 0.1979 | ||
| Unknown | 0.7 | 0.1293 | ||
| Duration of low back pain (in a 12 month period) | < 0.0001 | < 0.0001 | ||
| 1–7 days | Reference | |||
| 8–30 days | 1.5 | 0.0854 | 2.8 | < 0.0001 |
| More than 30 days but not everyday | 3.4 | < 0.0001 | 3.8 | < 0.0001 |
| Everyday | 4.5 | < 0.0001 | 5.0 | < 0.0001 |
| Unknown duration | 4.8 | 0.0002 | 2.9 | 0.0065 |
| Type of pain | 0.0003 | < 0.0001 | ||
| Other type of low back pain | Reference | |||
| Sciatica, pain radiating above the knee | 2.3 | < 0.0001 | 2.6 | < 0.0001 |
| Acute low back pain | 1.4 | 0.2170 | 1.3 | 0.3222 |
| Sciatica, pain radiating below the knee | 1.4 | 0.0551 | 2.0 | < 0.0001 |
| Unknown | 0.6 | 0.2301 | 1.1 | 0.7219 |
| SF36 Physical Functionning score | 0.0022 | 0.0123 | ||
| >95 | Reference | |||
| < 80 | 2.2 | 0.003 | 1.9 | 0.0026 |
| ≥ 80 and ≤ 95 | 1.4 | 0.0709 | 1.3 | 0.1440 |
| Unknown | 1.3 | 0.5962 | 2.0 | 0.0900 |
| SF36 Mental Health score | 0.0390 | |||
| >68 | Reference | |||
| < 56 | 1.4 | 0.0456 | ||
| ≥ 56 and ≤ 68 | 0.9 | 0.6823 | ||
| Unknown | 1.8 | 0.0787 | ||
1.3.3.2.1
In men
The results for consultation with a GP did not greatly differ from those concerning consultation with a healthcare professional in general. The duration of LBP, the presence of sciatica and the SF-36 Physical Functioning score were associated with consultation with a GP.
However, a low score at the SF-36 Mental Health score was significantly correlated with consultation with a GP, relative to the highest-scoring category (OR: 1.4; CI: [1.0–2.0]).
1.3.3.2.2
In women
On the whole, a woman’s age was not significantly associated with consultation with a GP. Nevertheless, the proportion of women aged 60 to 69 consulting was 30% lower than that for women aged 30 to 39 years. This difference was statistically significant.
Compared with the “no qualification or missing data” value, women with at least 2 years of higher education were 2-fold less likely to consult a GP for LBP (OR: 0.5; CI: [0.4–0.8]).
As noted for health professionals in general, longer periods of LBP were related to more frequent consultation with a GP. Compared with the other types of LBP, sciatic pain (regardless of whether or not it radiated below the knee) doubled the frequency of consultation with a GP (OR sciatic pain not radiating below the knee : 2.6; CI: [1.8–3.7]) (OR sciatic pain radiating below the knee : 2.0; CI: [1.4–2.9]).
Furthermore, women with the lowest SF-36 Physical Functioning scores were almost twice as likely to consult a GP for LBP as women with the highest scores (OR: 1.9; CI: [1.2–2.8]).
1.3.3.3
Consultation with a physiotherapist
Table 3 presents the factors associated with consultation with a physiotherapist for LBP, in men and in women. Subjects having reported a consultation with a physiotherapist for LBP in the 2-month survey period were compared with those who reported LBP in the previous 12 months (in the survey interview or the self-questionnaire) but had not consulted a physiotherapist.
| Men ( n = 100 vs n = 3885) | Women ( n = 145 vs n = 4662) | |||
|---|---|---|---|---|
| Variables | OR | p | OR | p |
| Age | ns | ns | ||
| SPC (most recent occupation) | 0.0470 | 0.0184 | ||
| Professionals | Reference | |||
| Farmers | 1.1 | 0.7883 | 0.8 | 0.7206 |
| Own account workers | 0.6 | 0.3166 | 0.2 | 0.0794 |
| Intermediate | 0.9 | 0.6078 | 1.1 | 0.6765 |
| Clerks, Sale employees | 0.9 | 0.7546 | 0.7 | 0.1558 |
| Blue collar workers | 0.4 | 0.0070 | 0.4 | 0.0329 |
| Unknown or unoccupied (women) | 0.4 | 0.2436 | ||
| Income per unit of consumption (in euros) | 0.0320 | 0.0071 | ||
| < 7345.295 | Reference | |||
| >7345.295 and < 14690.59 | 2.8 | 0.0978 | 1.7 | 0.2079 |
| >14690.59 | 3.8 | 0.0307 | 2.8 | 0.0191 |
| Rural or urban, size of the town | 0.0143 | |||
| Rural | Reference | |||
| Small town, between 5000 and 19999 inhabitants | 1.2 | 0.4678 | ||
| Medium size town, 20000 to 99999 inhabitants | 1.2 | 0.6410 | ||
| Large town or Paris | 0.5 | 0.0293 | ||
| Duration of Low back Pain (in a 12 month period) | < 0.0001 | < 0.0001 | ||
| 1–7 days | Reference | |||
| 8–30 days | 1.7 | 0.1566 | 3.0 | 0.0006 |
| More than 30 days but not everyday | 4.2 | < 0.0001 | 4.8 | < 0.0001 |
| Everyday | 4.9 | < 0.0001 | 7.3 | < 0.0001 |
| Unknown | 1.0 | 0.9569 | 1.5 | 0.2916 |
| SF36 Physical functionning score | 0.0240 | |||
| >95 | Reference | |||
| < 80 | 1.8 | 0.0751 | ||
| ≥ 80 and ≤ 95 | 1.2 | 0.4268 | ||
| Unknown | 5.0 | 0.0015 | ||
1.3.3.3.1
In men
Consultation with a physiotherapist for LBP was most strongly associated with the household’s income per unit of consumption and with the SPC.
Men with the highest incomes were nearly four times more likely to consult a physiotherapist for LBP than those with lower incomes were (OR: 3.8; [1.1–12.7]).
Workers were only half as likely to consult a physiotherapist as managers and the learned professions were (OR: 0.4; [0.2–0.8]).
The duration of LBP in the previous 12 months was also associated with consultation with a physiotherapist, with a threshold corresponding to a duration of 30 days. Men suffering from LBP every day were five times more likely to consult with a physiotherapist for LBP than men who had suffered for 1 to 7 days were.
Lastly, the number of inhabitants in the subject’s locality of residence was related to consultation with a physiotherapist. Subjects living in an urban area with over 100,000 inhabitants or in the Paris urban area were significantly less likely to consult a physiotherapist than subjects living in the countryside (OR: 0.5; [0.3–0.9]).
1.3.3.3.2
In women
As was seen for men, two societal markers were associated with consultation with a physiotherapist for LBP: the SPC and income per unit of consumption.
Women in the “worker” SPC were only half as likely to consult a physiotherapist as managers and learned professions were (OR: 0.4; [0.2–0.9]).
The women from households with the highest incomes were nearly three times more likely to consult a physiotherapist than the less affluent women were (OR: 2.8; CI: [1.2–6.6]).
As was the case for consultations in general, the probability of consulting a physiotherapist increased with the duration of LBP. A woman suffering from LBP every day was seven times more likely to consult a physiotherapist than a woman who had suffered from LBP for just 1 to 7 days was (OR: 7. 3; CI: [3.9–13.6]).
1.3.4
Consultation with a physiotherapist, severity of lower back pain and income
Fig. 2 provides a more detailed illustration of some of the results from the previous models – particularly those dealing with the impact of LBP severity and income. The figure shows the percentage of subjects consulting a physiotherapist (for subjects of both genders having reported LBP in the previous 12 months in the self-questionnaire or during the interview) as a function of income per unit of consumption and the SF-36 Physical Functioning score (with a higher score corresponding to less functional problems).
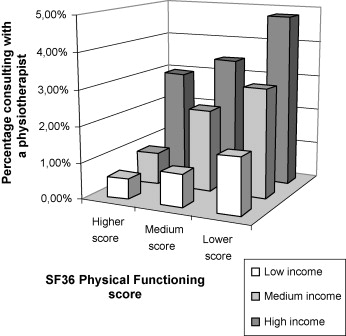
The lower the physical capacity score, the more the subjects consulted with a physiotherapist (regardless of the level of income). We also observed that the level of income appeared to be a determinant of consultation, regardless of the Physical Functioning score.
1.4
Discussion
1.4.1
Study limitations
One important limitation of this study is that it did not enable us to document the links between the various consultations with healthcare professionals. A 2-month survey of the general population is not appropriate for describing patient pathways between professionals who differ in terms of their access conditions. In particular, the survey did not enable us to distinguish between direct consultations on one hand and referrals by another health professional on the other.
Comparing France with other countries poses specific problems, even when considering the definition of the medical specialties consulted; in some countries, consultations with a rheumatologist for low back pain are less frequent, and other healthcare professionals (such as chiropractors and massage therapists) play a significant role in LBP care.
The fact that the reference period differed according to whether we considered consultations with healthcare professional (2 months) or the stated presence of LBP (12 months) complicates the interpretation of our present results. Here, we decided to compare people having consulted a healthcare professional in the previous 2 months with people who had not consulted but had reported having suffered from LBP at the time of the survey or in the previous 12 months. An alternative would have been to compare people having consulted with the remainder of the whole survey sample and without taking into account self-reported LBP. However, the latter approach would have prevented us from distinguishing between factors related specifically to consultation and those related to the presence of LBP.
When the regional variable (ZEAT) was included in our analyses, the results were difficult to interpret; there was no apparent link with the density of medical professionals and neighbouring regions were not alike in terms of consultation patterns. Moreover, these regional “effects” differed for men and women. The absence of pertinent results might also be due to the arbitrary nature of the official ZEAT regions; for example, the so-called “Paris Region” includes the Burgundy, Centre, Champagne-Ardenne, Lower Normandy, Upper Normandy and Picardy regions.
Given this context and the lack of a pertinent regional variable, we did not investigate regional differences further.
In terms of seeking care, we considered only consultation with a physiotherapist or a physician (all specialties) and not medication intake. It is probable that patients suffering from acute LBP (even for a short duration) take pain relief medications. Hence, the use of over-the-counter (OTC) medication may equate to seeking care. The next issue would be to find out which factors are specifically related to use of OTC medications.
1.4.2
The main results
Some of the above-mentioned results were expected; it is not very surprising to see that subjects with severe LBP are more likely to consult a healthcare professional.
In the present study, the duration of LBP was a significant determinant of the decision to seek care (for both men and women and regardless of the type of healthcare professional consulted). The presence of sciatica was also a significant determinant (except for consultations with a physiotherapist).
Several studies in other countries have already confirmed the impact of the duration of LBP, the presence of sciatica and the subject’s physical capacities on the decision to seek care from a healthcare professional.
In the study by Szpalski et al., seeking care was related to the duration of the painful symptoms and the patient’s belief that his/her backache would be a long-term problem . The correlation between the duration of LBP and seeking care was also highlighted by Carey et al.’s study in South Carolina .
The link between sciatica and seeking care found in the present study agrees with Carey et al.’s findings .
Somewhat paradoxically, some LBP situations make the subject less likely to seek care; in particular, the presence of sciatic pain radiating below the knee is associated with less frequent consultation than sciatic pain that does not radiate below the knee. It is possible that certain long-term, chronic situations are poorly medicalized.
Functional impairment has appeared to be a significant factor in most of the studies to have addressed this aspect . This is hardly surprising because one would expect individuals to consult more readily when they feel very handicapped from a physical standpoint.
Our most unexpected findings concern the factors associated with consultation with a physiotherapist.
We do not have an obvious explanation for the less frequent consultation with a physiotherapist in large towns and the Paris urban area by male subjects; the greater diversity of health services in larger towns than in the countryside is one hypothesis.
For both men and women, we found that two societal markers were associated with consultation with a physiotherapist for LBP: income per unit of consumption and the SPC.
One hypothesis was that people were more likely to consult a physiotherapist if their LBP causes problems at work. In this respect, workers should consult a physiotherapist more frequently. In fact, managers and the learned professions were most likely to consult.
The fact that high-income individuals consulted a physiotherapist more frequently suggests that the cost of care limits recourse to this type of treatment.
The fact that the consultation with a physiotherapist increases with income per unit of consumption has already been mentioned in a 1998 French study covering health problems in general . In terms of private health insurance, the latter study showed that workers tended to have individual contracts, which provide less coverage and lower reimbursements that the company health insurance packages held by senior managers.
Our results raise a number of questions. Is the more frequent consultation with a physiotherapist by subjects in the most affluent households related to the patients themselves (who might consult more readily on their own initiative) or their referring physicians? Do the up-front honoraria requested by physiotherapists dissuade less affluent subjects? Lastly, is consultation with a physiotherapist related to the type of private health insurance contract held (in addition to the presence or absence of private health coverage per se).
1.5
Conclusions and perspectives
Seeking care for LBP is generally associated with the severity of the condition. There were no apparent financial barriers to accessing care from a GP. Nevertheless, in the French system in which access to care for low-income households has (in principle) been facilitated since 2000 via additional public health insurance coverage, consultation with a physiotherapist appears to be related to income and the SPC. This issue deserves further investigation. Another question relates to the optimal management of LBP, which is related to the kind of treatment and not merely consultation with a health professional. Documentation of these various factors would require more comprehensive data on patient pathways in the general population, the absence of care, the use of OTC medication and (iv) renouncement of access to certain types of care.
Conflicts of interest
The authors have no conflict of interest.
Acknowledgements
This work was partly funded by the French Ministry of Health’s MIRE research unit, as part of secondary analyses of the Décennale Santé survey data.
2
Version française
2.1
Introduction
La fréquence et les répercussions socioéconomiques de la lombalgie constituent un problème de santé publique majeur en France comme dans la plupart des pays industrialisés.
En France, le coût financier médical direct des lombalgies est évalué à 1,4 milliard d’euros et représente 1,6 % des dépenses de santé selon le rapport du Groupe technique national de définition des objectifs de santé publique (GTNDO) de 2003 à l’attention de la Direction général de la santé (DGS) en collaboration avec l’Inserm .
Une étude française réalisée à partir des données de l’enquête Décennale santé (EDS) 2002–2003 a permis d’obtenir des estimations de la fréquence des lombalgies en population générale chez les personnes de 30 à 64 ans . La prévalence de la lombalgie « au moins un jour dans les 12 derniers mois » est ainsi estimée à 55 % et celle de la lombalgie « plus de 30 jours dans les 12 derniers mois » à 17 %.
De part ces fréquences élevées, il paraît légitime de s’interroger sur le recours aux soins pour lombalgie et aux facteurs liés à ce recours.
Plusieurs enquêtes menées dans divers pays se sont intéressées à cette question .
Une étude menée aux Pays-Bas (à partir d’une enquête et de registres de santé sur une population de 25 ans ou plus) insiste sur le fait que la majorité des lombalgiques n’ont pas de recours aux soins . Dans l’enquête auprès des individus, 13 % de la population déclare avoir eu recours aux soins pour lombalgie dans l’année alors que d’après les registres le recours pour lombalgie est de 8,9 %.
Par ailleurs, dans une étude menée par téléphone par Carey et al., en Caroline du Nord, 7,6 % de la population interrogée déclare une lombalgie aiguë sur une période d’un an . Parmi les lombalgiques, seuls 39 % ont consulté un professionnel de santé pour leur lombalgie.
En France, à notre connaissance, aucune étude n’a été réalisée dans le but d’estimer la fréquence des recours aux soins pour lombalgie en population générale et les facteurs liés à ce recours.
Cet article a pour objectif de décrire la fréquence du recours aux soins pour lombalgie sur une période de deux mois (période correspondant à la durée de l’enquête) ainsi que les spécialités médicales consultées et mettre en exergue les facteurs associés au recours aux soins pour lombalgie parmi les personnes ayant déclaré une lombalgie.
2.2
Matériel et méthodes
2.2.1
L’enquête
L’échantillon national de l’EDS 2002–2003 comporte 16 449 ménages, soit 40 867 individus. La population cible est l’ensemble des « ménages ordinaires » résidant en France métropolitaine, ce qui exclut par conséquent les ménages collectifs (maisons de retraite, foyers de travailleurs…).
L’enquête comporte trois entretiens réalisés par des enquêteurs spécialisés et un questionnaire autoadministré incluant entre autres un questionnaire spécifique aux lombalgies (version française du questionnaire nordique) et le questionnaire SF36 .
Les données recueillies permettent de croiser de nombreuses caractéristiques sociodémographiques et économiques des individus avec leur état de santé et leur consommation de soins.
2.2.2
Population d’étude
La population retenue pour cette étude est constituée de toutes les personnes interrogées dans l’EDS, âgées de 30 à 69 ans, aptes à répondre à l’autoquestionnaire et ayant participé aux trois visites de l’enquêteur, soit 17 792 personnes (8403 hommes et 9389 femmes).
Ont donc été exclues 210 personnes non aptes à répondre à l’autoquestionnaire et 5723 personnes qui n’ont pas participé aux trois visites de l’enquêteur.
La classe d’âge de 30–69 ans a été choisie afin de pouvoir prendre en compte les situations professionnelles des personnes et aussi le fait de la relation entre lombalgie et âge. En effet, à partir d’un certain âge, les facteurs liés à la lombalgie sont probablement différents.
2.2.3
Variables décrivant les lombalgies
Dans cette étude, la variable de santé principale était le recours à un professionnel de santé pour lombalgie dans les deux mois de l’enquête, avec une précision sur le type de professionnel. Nous avons considéré qu’un sous-ensemble des personnes de l’enquête était susceptible de recourir à un professionnel de santé pour lombalgie, ceux qui avaient signalé la présence d’une lombalgie (dans les 12 mois précédents) dans l’autoquestionnaire, et ceux qui avaient déclaré spontanément à l’enquêteur une lombalgie parmi les problèmes de santé chroniques. Parmi ces personnes, et pour caractériser la sévérité de la lombalgie, trois variables ont été utilisées : la durée de celle-ci sur 12 mois déclarée dans l’autoquestionnaire, la localisation de la douleur (présence d’une irradiation à la jambe…) et le score au SF36 Physical Functioning (capacité physique).
2.2.4
Autres variables prises en compte
Parmi les nombreuses variables disponibles dans l’enquête, nous avons sélectionné trois catégories de variables, retenues selon la littérature existante sur le sujet, et en fonction d’hypothèses à tester, en particulier sur d’éventuelles disparités géographiques :
- •
les variables sociodémographiques et économiques : sexe, âge, diplôme, statut matrimonial, vie en couple, revenu par unité de consommation, occupation actuelle, profession et catégorie socioprofessionnelle (PCS), revenu minimum d’insertion (RMI), couverture maladie universelle (CMU), couverture complémentaire, zone d’étude et d’aménagement du territoire (Zéat), taille de la commune, classement en zone urbaine sensible (ZUS) ;
- •
les variables individuelles : indice de masse corporel (IMC) calculé comme le rapport poids/(taille) 2 , taille, score au SF36 Mental Health (évaluant la santé psychique) ;
- •
les variables d’expositions professionnelles, issues de l’autoquestionnaire : exposition au port de charges lourdes durant le travail, postures pénibles et fatigantes durant le travail.
2.2.5
Méthodes statistiques
Les analyses ont été menées séparément chez les hommes et les femmes, en se restreignant pour la presque-totalité des analyses au sous-échantillon des sujets qui étaient susceptibles de recourir à un professionnel de santé pour lombalgie, c’est-à-dire ceux qui avaient signalé une lombalgie.
Dans un premier temps, les analyses ont été réalisées de façon univariée. Les associations entre le recours à un professionnel de santé (kinésithérapeutes et/ou médecins) et les variables sélectionnées ont été étudiées. Les facteurs associés au recours au médecin généraliste (exclusivement ou non) et les facteurs associés au recours au kinésithérapeute ont également été recherchés.
Dans un second temps, parmi les individus ayant déclaré une lombalgie dans les 12 mois (dans l’autoquestionnaire ou spontanément à l’enquêteur), des modèles de régression logistique pas à pas descendants ont été utilisés à partir des variables significatives à un seuil de 20 % en mode univarié, cela pour les trois types de recours (professionnel de santé, médecin généraliste, kinésithérapeute).
Dans chacun de ces modèles, les variables significatives au seuil de 10 %, ainsi que l’âge, ont été conservés dans le modèle final. La démarche d’analyse retenue peut amener à ce que les variables retenues dans les modèles finaux soient différentes pour les hommes et les femmes, donc que les variables d’ajustement ne soient pas les mêmes. De façon générale, les variables significatives au seuil de 10 %, mais non au seuil de 5 %, dans les modèles finaux, sont considérées avant tout comme des variables d’ajustement, au même titre que l’âge.
Au vu des résultats d’analyses préliminaires (qui seront brièvement évoqués dans la discussion), nous avons décidé de présenter ici des résultats ne prenant pas en compte la variable régionale Zéat. En effet, chez les hommes comme chez les femmes, cette variable intervenait significativement dans les trois types de recours étudiés. Cependant, aucune région ne se distinguait nettement, et les résultats étaient très difficilement interprétables. Par ailleurs, inclure ou non la variable n’avait pas de conséquence pour les autres résultats.
Les analyses statistiques ont été réalisées avec le logiciel SAS version 9.1.
2.3
Résultats
2.3.1
Fréquence du recours aux soins
Parmi les 17 792 individus de l’étude, 44,9 % déclarent avoir déjà souffert de lombalgie dans les 12 derniers mois soit à l’autoquestionnaire, soit spontanément à l’enquêteur.
Un total de 808, soit 4,54 %, déclarent avoir eu recours au moins une fois à un professionnel de santé pour lombalgie sur la période de deux mois, ce qui correspond à 962 consultations médicales et 245 recours à un kinésithérapeute.
En se restreignant aux individus ( n = 8792) ayant déclaré une lombalgie dans les 12 derniers mois dans l’autoquestionnaire ou spontanément, près de 9,19 % déclarent avoir eu au moins un recours à un professionnel de santé durant la période de l’enquête, soit deux mois.
2.3.2
Spécialités médicales consultées pour lombalgie
Le médecin généraliste représente 77 % des 962 consultations médicales pour lombalgie ( Fig. 1 ). La seconde spécialité médicale la plus consultée pour lombalgie est la rhumatologie (9 %). Les autres spécialités correspondent à peu de consultations, mis à part les chirurgiens qui représentent la troisième spécialité la plus consultée pour lombalgie avec près de 3 % de recours.










