Chapter 44 Seating and positioning for disabled children and adults
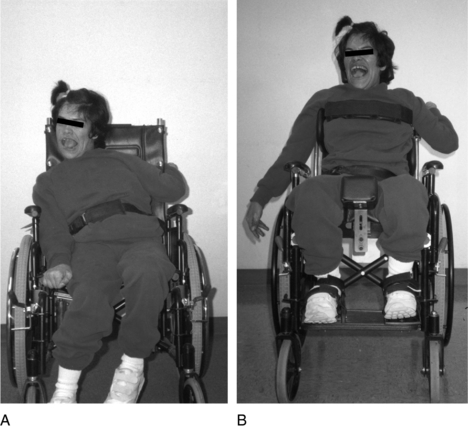
People with disabilities are living longer, and their number is growing. In 2003, 34.3 million people (12.1% of the population) in the United States (noninstitutionalized) had physical limitations in activities due to a chronic condition. An estimated 1.6 million are wheelchair users. Baby boomers are coming of age and are acquiring disabling conditions. By the year 2030, the number of elderly will double to 71.5 million. Medical technology has improved the rate of survival for children and adults with disabilities and their long-term management. Long-term debility is a major risk factor for pressure ulcers. Improvement in the survival rate has increased the number of persons at risk for pressure sores. An estimated five million people in the United States have chronic wounds. From 1.1 to 1.8 million people develop new ulcers each year, and the financial cost and emotional burden are heavy.4,49 The two groups at highest risk are the elderly and persons with spinal cord injury (SCI).3,19 Advances in seating and mobility have made a difference in controlling deformities, preventing pressure sores, and expanding the individual’s potential in life, ensuring participation socially, educationally, and vocationally. Proper seating is like an external orthosis, important for support, comfort, and pressure relief in sitting.18 Better anatomical alignment of the pelvis and trunk enhances physiological functions, such as swallowing and cardiopulmonary function, and affects upper extremity function. Postural supports enhance functional movement by decreasing the influence of abnormal tone and reflexes, thereby improving postural alignment and potential access to technologies, such as powered mobility, communication devices, and computers (Fig. 44-1). The seating system should be as dynamic as possible to allow for growth changes in a child or if a decline in function is anticipated. The seating system must be user friendly for the person in the wheelchair and for the caregiver. The user, family, and caregivers play a key role and must be interviewed extensively regarding the user’s medical and functional needs, environmental considerations, and lifestyle issues.
Evaluation process for seating and mobility systems
A seating and mobility system evaluation should address all aspects of a person’s medical and personal lifestyle issues. The following categories should be assessed thoroughly.
Reflex-Influenced Posturing: Is reflex-influenced posturing interfering with the patient’s functional potential for maintaining the sitting position? For example, two influential primitive reflexes active in seated posture are the tonic labyrinthine reflex, which causes extension of the head, trunk, and extremities as the body tilts backward or reclines, and asymmetrical tonic neck reflexes, which cause rotation of head, trunk and pelvis and potentially a windswept deformity. At times, this reflex posturing is functionally used to extend the upper extremity in order to drive a power wheelchair or point to a communication device. Persons with athetosis or dyskinetic-type movement disorders may use reflex posturing for stability in order to use their extremities purposefully. The seating device may help inhibit unwanted movements and permit functional movements.6
Evaluation of Protective Sensation: Evaluation of protective sensation and assessing for red areas or potential pressure areas helps to determine the appropriate seating surface. History of scar tissue or previous pressure sore intervention can predict areas of high risk. Aging affects the elasticity of the skin and increases risk of damage from shearing, pressure, heat, and moisture.
Functional assessment
The outcome of evaluation of a person’s seating needs focuses on one of three areas in a framework for seating and positioning decision making categorized by Cook and Hussey9: technologies for postural control (typically for the child or client with cerebral palsy), technologies for pressure control, for those at high risk (e.g., population with SCI), or technologies for comfort (for the elderly or patient with amyotrophic lateral sclerosis).
Seating alignment
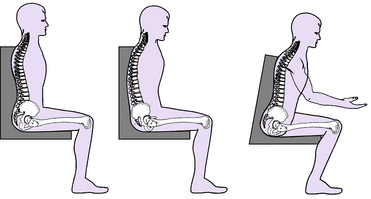
Ideal sitting alignment is different for an able-bodied person than for a disabled person, and depends on the individual’s abilities. Sitting is dynamic; it is a continuous process of postural changes whether the position is task oriented or one of rest. For the able-bodied person, a sitting posture with an anterior pelvic tilt and decreased lumbar flexion is the most favorable posture.17,18,40 Generally three postures of sitting alignment are assumed (Fig. 44-2). Ideally, an upright, symmetrically balanced trunk over a stable pelvis allows better upper extremity reach, head control, and visual field. However, in the sitting position, the pelvis tends to roll back into a posterior tilt because the hips are flexed and the hamstrings pull the pelvis back; the tilt is accentuated when the knees are extended.50 The line of gravity is posterior to the ischial tuberosities. This posture is adopted as a position of rest by an able-bodied person and as a position of stability by a wheelchair user with tetraplegia. The second sitting position is achieved by activating the back extensors to tilt the pelvis anteriorly into lumbar lordosis. As the pelvis rolls anteriorly, the line of gravity falls directly through the ischial tuberosities.15 This posture usually is assumed by a person with muscular disease as it is functionally advantageous because of weakness that is greater proximally than distally.16 The third seated posture is a forward sitting posture that has been described by Kangas25 and Adrian and Cooper1 as a functional task position or position of readiness. In this position, the trunk is forward and the line of gravity shifts toward the direction of activity. The trunk flexes forward in a position of anticipation. The arms and trunk are naturally brought forward into the visual field, and the feet are shifted backward behind the knees and bear more weight.
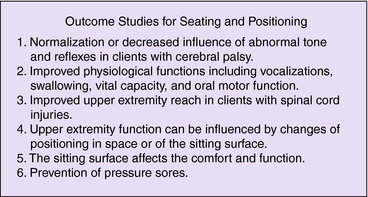
Outcome studies of seating and positioning for function
A number of studies reported on how seating affects functional activities, upper extremity function, head control, and visual field.24,33,36 The components of a seating system can provide support to align the body, normalize tone, prevent deformities, and clearly influence upper extremity movement. In one study, the sitting surface was explored to better determine the capacity to maintain balance and posture as a prerequisite for activities of daily living. The center of pressure of reaching was determined to be significantly greater on a generically contoured sitting surface than on a flat foam surface or a 3-inch Roho seat cushion.2 The effect of different backrest heights and types of cushions were investigated in the SCI population to determine the relationship between posture and upper extremity reaching. The posture adopted by the user and the American Spinal Injury Association (ASIA) score were significant, and no evidence indicated that the type of cushion or back height affected reach.48
Improvements in autonomic functioning, including respiratory, oral intake and digestion in children with cerebral palsy was found following adjustments in seating systems with improvement of the trunk, neck and head alignment.7 Hulme23 found positive perceived changes in social interaction, positioning, tracking, grasping, and self-feeding skills. Nwaobi37 found that the vital capacity in children with cerebral palsy improved with positioning in a seating system versus a sling type wheelchair. Improvements in speech intelligibility were documented in children with cerebral palsy using adapted seating versus without.34
Reports on the effects of seating on upper extremity function are conflicting. In a 1986 study of children with cerebral palsy, different amounts of hip flexion were found to affect upper extremity function.36 Another study found that children with cerebral palsy were able to activate and release a switch the fastest when they were in an anterior 15-degree tilt or in the position of readiness versus 0, 15, or 30 degrees of tilt back.35 However, McPherson et al.31 found no significant differences in the quality of upper extremity movement in subjects with cerebral palsy in four different positions. Seeger et al.45 also did not find any improvement (Fig. 44-3).
Seating assessment
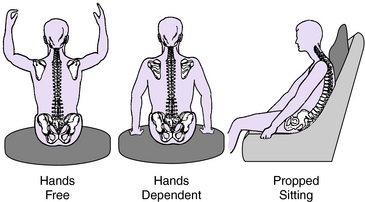
Classifications and description of sitting ability
The ability to sit independently is one factor that determines the type or amount of seating support needed. Hoffer21 classified a person’s ability to sit according to the amount of trunk control present. His classifications were modified by Tredwell and Roxborough in 1991 to include generalizations regarding the type of seating needed (Fig 44-4):
Patterns of deformity
The position of the pelvis influences the alignment of the trunk and therefore of the shoulders, upper extremities, and head. The three common patterns of postural malalignment are as follows28:
Symmetrically Slouched: This position begins with a posterior pelvic tilt. The trunk collapses into a C curve, and the shoulders are protracted with the head forward. The most common cause of a posterior pelvic tilt in persons with cerebral palsy is hamstring hypertonicity. For persons with tetraplegia, the symmetrically slouched position can be a position of stability in which they are able to raise their arms for balance and functional activities28.
Lordotic Posture: This posture begins with an anterior pelvic tilt. The pelvic tilt locks the lumbar facets into extension, mechanically providing spinal stability. Hyperlordosis typically is observed in patients with Duchenne muscular dystrophy prior to spine fusion because of proximal weakness and an imbalance in strength between the abdominals and back extensors.
Asymmetrical or Windswept Posture: This posture is one of the most difficult deformities to control and to treat. The windswept deformity is described as being windswept to the left if the left thigh is abducted and the right thigh is adducted. It is associated with a triad of deformities: dislocated or subluxed hip usually on the adducted side, pelvic obliquity, and scoliosis. A dislocated hip may be painful, severe scoliosis may compromise cardiopulmonary function, and the increase in pelvic obliquity increases the risk for pressure sores.12,41 The person may try to offload the painful hip, which worsens the position and pressure distribution.
The relationship among windswept hips, pelvic obliquity/hip dislocation, and scoliosis was first described by Letts in 1984 in children with cerebral palsy. “Acquired and preventable Special Seating will NOT prevent a contracted hip from dislocating.” However, Letts did advocate abduction of the lower extremities to 25 degrees and not just neutral to decrease abnormal muscle activity.27 Increased abduction also results in good approximation of the head of the femur into the acetabulum, which promotes bony joint development in children. Therefore, flexion and abduction of the hip are recommended to prevent extensor and adductor posturing in children with cerebral palsy who are at risk for development of the windblown syndrome. Without adequate fixation of the pelvis, however, this position may be difficult to obtain.
High complication rates have been documented in patients with severe neuromuscular scoliosis: 81% by Loinstein30 in 1984 and 48% by Boachi8 in 1989. They believed that the high risk of surgery outweighs the benefits, so comfortable seating is the treatment of choice. Table 44-1 lists possible causes and equipment solutions for postural alignment problems.
Table 44-1 Causes and equipment for patterns of deformities
| Problem | Cause | Equipment Solutions |
|---|---|---|
| Slouched posture | ||
| Posterior pelvic tilt | Sling upholstery | Three-point control: solid seat, firm back, and pelvic/hip seat belt |
| Rigid anterior pelvic support: subasis bar, knee blocks | ||
| Inappropriate seat depth | Measure from PSIS to popliteal, include fixed kyphosis | |
| Hip/knee extension | Extensor tone (hip and knee) | Antithrust seat |
| Increase hip angle >90 degrees | ||
| Increase knee angle >90 degrees (foot placement behind knee) | ||
| Hip extension contracture | Accommodate seat cushion to unilateral contracture | |
| Thoracic kyphosis | Trunk weakness/paralysis | Unilateral split seat or leg trough, to maintain trunk upright |
| Fixed deformity | Recline back, tilt back in spine | |
| Lower back height, accommodate in back cushion | ||
| Shoulder protraction | Spasticity/weakness | Firm back with lumbar/thoracic extension |
| Back height too high | Appropriate back height | |
| Accommodate with molded back | ||
| Shoulder straps pulling up and back | ||
| Forward head posture | Weakness | Occipital support with capital extension |
| Spasticity | Head band (stationary or dynamic) attached to head rest | |
| Reflex posturing if too reclined | Recline back or tilt back to seat angle | |
| Rotational/oblique posture | ||
| Pelvic obliquity/pelvic rotation | Sling seat | Firm seat |
| Scoliosis | Lateral hip guides | |
| Hip dislocation | Flexible: build up under low side for even pressure | |
| Asymmetrical hip ROM | Fixed: build up under high side, relieve pressure under low side | |
| Custom-molded seat | ||
| Off-set cut-out in cushion | ||
| Accommodate seat depth for leg length discrepancy | ||
| Anterior pelvic belt | ||
| Two-piece sub-ASIS bar | ||
| Hip problems | Sling seat | Firm seat with medial thigh support |
| Hip adducted—internal rotation | Adductor tone | Medical thigh support |
| Hip abduction—external rotation | Hypotonia | Lateral thigh/knee stabilizers |
| Fixed deformity | Accommodate | |
| Windswept hips | Pelvic rotation | Three-point control: hip guides, medial, and lateral thigh support |
| Adducted thigh with abducted thigh | Dislocated hip | Build up for lack of thigh support |
| Scoliosis | Custom-molded seat | |
| Thoracic scoliosis | Pelvic obliquity and rotation | Three-point control: pelvic/trunk supports |
| Flexible | Weakness | Deep contoured back or trunk supports |
| Spasticity | Rotational deformity: curved supports | |
| Fixed | Asymmetric tone/muscle strength | Custom-molded back or adjustable-tension back upholstery to accommodate to rib hump deformity |
| Asymmetric head posture | Scoliosis | Appropriate support of pelvis, trunk, and shoulder girdle |
| Fluctuating tone | ||
| Reflex posturing | Head and neck support. Support of occiput to mastoid process or over the ear to the temple for lateral control | |
| Weakness | ||
| Visual compensation | Stationary or dynamic headband | |
| Lordotic posture | ||
| Anterior pelvic tilt | Muscle imbalance | Placement of belt across ASIS |
| Hip flexion | Abdominal weakness | Wedge seat/cushion to accommodate if fixed |
| Thoracic lordosis | Contractures | Tilt in space manual or power frame, adjustable seat angle |
| Anterior chest support: molded chest plate, wide Velcro strap | ||
| Retracted shoulders | Spasticity | Appropriate pelvic/trunk positioning with chest support |
| Posturing for trunk weakness | Shoulder wedges | |
| Extended head posture | Spasticity | Neck ring |
| Weakness | Occipital support |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree