The scapulothoracic articulation consists of the ventral (anterior), concave surface of the scapula and the convex posterior thoracic wall. The stability of the scapula on the posterior thoracic cage is provided by 10 periscapular muscles. The acromioclavicular joint is the only other attachment of the scapula to the rest of the skeleton. At rest, the normal position of the scapula is approximately 2 cm lateral from the spine and between the second and the seventh ribs (
3). The plane of the scapula is a static position defined as 30° to 40° in the frontal plane with 10° to 20° of anterior inclination (
4). The soft tissue and osseous structures of the scapulothoracic space determine the congruity of movement.
The soft tissue structures surrounding the scapula consist primarily of muscle and bursae. More importantly, the scapulothoracic articulation consists of three muscular layers: superficial, intermediate, and deep.
Table 26.1 defines these layers with respect to muscles and bursae (
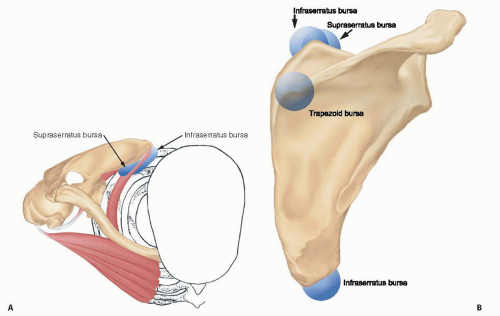
5). Understanding this anatomy is critical to determining the etiology of a symptomatic scapulothoracic articulation, to establishing an adequate treatment plan, and to planning operative procedures. Several bursae exist not only between the muscles but also between the muscles and the chest wall (
Fig. 26.1).
Table 26.2 provides a summary of the scapulothoracic bursae, which are critical to the normal function of the scapula and a common source of pain and crepitus.
The osseous anatomy of the scapula and the ribs is also important in understanding the etiology of a snapping scapula. The surfaces of these structures must be smooth in order for there to be normal motion between the scapula and the thorax. Bony abnormalities of the scapula or the ribs may create incongruity and lead to a symptomatic scapulothoracic motion.
Etiology of the Snapping Scapula
Snapping of the scapula occurs during rotation of the anterior scapula on the posterior surface of the chest wall. In general, the etiology of the snapping scapula can be classified according to the pathologic lesion, which is usually a soft tissue or bony prominence that disrupts the congruity of the scapulothoracic space (
Table 26.3). In some cases, there may be no identifiable lesion. Clinically, the snapping may be described as physiologic (nonpathologic/asymptomatic) or pathologic (symptomatic). Patients with physiologic snapping have scapulothoracic crepitus but are asymptomatic. In these patients, treatment is rarely necessary. However, the onset of symptoms, such as pain, reflects a transition to a pathologic articulation that requires further assessment and treatment. In most cases, this transition represents either a change in the intervening soft tissue between the scapula and the chest wall or the development of an osseous lesion that causes a loss of congruity between the scapula and the thorax. In some patients, pain may occur without audible or palpable crepitation or snapping (
6).
The most common soft tissue abnormalities involve bursae and muscles. Similar to bursae near other joints, the scapulothoracic bursae can become inflamed and symptomatic. In chronic cases, the development of adhesions and scar tissue in the scapulothoracic space significantly affects scapular function (
7).
Trauma, disuse, or nerve injury may lead to damage, weakness, and atrophy of the periscapular muscles (
8,
9). As a result, there is often an associated decrease in the soft tissue cushion interposed between the scapula and the rib cage. The loss of soft tissue decreases the congruency of the scapulothoracic space and contributes to the development of a painful, snapping scapula. For example, the serratus anterior atrophy occurs secondary to paralysis of the long thoracic nerve. Likewise, the subscapularis atrophy occurs secondary to surgical fusion of the glenohumeral joint or from damage of motor branches to the subscapularis during open surgery. The serratus anterior and subscapularis are two of the most important muscles that prevent scapular winging and provide a mechanical cushion between the scapula and the ribs. Atrophy and loss of function of these muscles are relevant factors in the development of a snapping scapula. Furthermore, the superior angle, inferior angle, and medial border are relatively poorly cushioned compared with the rest of the scapula. As a result, these locations are common areas of increased friction that lead to symptomatic snapping. In addition, muscle fibrosis can develop secondary to traumatic injuries and disrupt the normal motion of the scapulothoracic space. Muscle tightness (pectoralis minor and levator scapulae) may cause abnormal scapulothoracic rhythm and produce a snapping scapula.
Less common causes of a snapping scapula include infection, congenital deformity, and tumors. Infectious lesions of the ribs or scapula may develop, in rare cases, secondary to tuberculosis or syphilis (
10). Sprengel’s deformity is present at birth and may lead to symptomatic
scapular motion later in life. Tumors, such as elastofibromas, may also develop in the scapulothoracic space (
11,
12). In some patients, the scapulothoracic symptoms may be out of proportion to the expected level of discomfort for a snapping scapula. In these cases, secondary gain, workers’ compensation issues, and psychiatric conditions should be considered as relevant factors in the development of a diagnosis and treatment plan.
Osseous Anatomy
The gliding motion of a bony prominence over the ribs provokes the sounds associated with a snapping scapula. The morphology of the superomedial border of the scapula is a common factor contributing to the development of this condition (
13,
14). Several reports have described variations in this morphology ranging from a thickened bulbous corner to a hook-shaped bony prominence (
7,
10,
14). More specifically, Luschka’s tubercle is a fibrocartilagenous nodule on the anterior aspect of the superomedial angle of the scapula. The prominent nature of the tubercle within the scapulothoracic space can become a significant source of pain contributing to the development of a snapping scapula. Being aware of its role in the development of a snapping scapula is essential to creating a treatment plan that addresses all sources of pain within the scapulothoracic space.
Bony prominences also develop secondary to fractures, dislocations, and tumors. Fractures of the ribs and/or scapula may heal with exuberant callus or as a malunion or nonunion that causes a painful, snapping scapula (
15). An osseous tumor, such as an osteochondroma, may form on the anterior surface of the scapula and, depending on its size, become a significant irritant during scapular motion. Another source of osseous irritation in the scapulothoracic space is a bone spur that develops from the traction
of muscles on the scapula during movement. This process most commonly occurs at the inferolateral portion of the scapula at the attachment site for the teres minor (
13). Overall, soft tissue or bony lesions in the scapulothoracic space most commonly contribute to the development of a symptomatic snapping scapula. Scapulothoracic pain may also occur secondary to cervical spondylosis, cervical radiculopathy, glenohumeral pathology, and periscapular muscle strain. These conditions should be considered in the differential diagnosis of all patients with a snapping scapula.