and Peter J. Millett2
(1)
Steadman Philippon Research Institute, Vail, CO, USA
(2)
The Steadman Clinic, Steadman Philippon Research Institute, Vail, CO, USA
Keywords
ShoulderScapulaScapulothoracicDyskinesisWingingPhysical examClinical exam9.1 Introduction
The scapula is a complex osseous structure that plays a critical role in the maintenance of glenohumeral stability throughout the entire range of motion of the shoulder. Therefore, an evaluation of scapular motion should be performed in each patient to prevent the development or progression of various shoulder conditions such as rotator cuff disease and glenohumeral instability. Specific physical exam findings and observations related to scapular motion can have a significant effect on the approach to either operative or nonoperative management in patients who present with shoulder pain. As an example, increased upward rotation of the scapula may be a compensatory mechanism to prevent pain related to shoulder pathology whereas increased downward rotation may be factor associated with the production of shoulder pathology [1]. An understanding of the pertinent anatomy and biomechanics of scapular motion is required before any diagnosis can be made regarding scapular motion.
9.2 Anatomy and Biomechanics
The primary function of the scapula is to provide a stable fulcrum against which humeral elevation and rotation can occur. This is achieved through dynamic positioning of the glenoid to maximize glenohumeral contact through all planes of shoulder motion (see Chap. 3 for a detailed explanation of normal three-dimensional scapular motion). A complete understanding of the osseous, muscular, bursal, and neurovascular anatomy along with the biomechanics of normal scapular motion is critical to the evaluation of any patient with shoulder pathology.
9.2.1 Osseous Anatomy
The scapula is a large, flat, triangular-shaped bone positioned over the posterior thorax between the second and seventh ribs. The scapula has three borders (superior, medial, and lateral) and two important angles (superomedial and inferomedial) that primarily serve as sites for muscle attachment (Fig. 9.1). According to Lewitt [2], the three-dimensional resting position of the scapula is defined as being tilted anteriorly between 10° and 20° and medially rotated in the coronal plane between 30° and 40° (in other words, the glenoid faces more in the superior direction). As discussed in Chap. 2, the scapula is also angled anteriorly between 10° and 20° from the coronal plane. This position of anterior angulation is often referred to as the “scapular plane” when evaluating the shoulder.
Fig. 9.1
Posterior view of a normal scapula. The superior, medial, and lateral borders along with the superomedial and inferomedial angles are labeled.
While the general shape of the scapula is fairly consistent across the population, there exist several known topographical variations that may predispose some individuals to certain pathologic conditions (such as scapulothoracic bursitis or snapping scapula syndrome). For example, Aggarwal et al. [3] performed measurements in 92 dried scapulae and found that the costal (anterior) surface of the scapula “undulated” and also varied in depth between 10.5 and 26.5 mm. The investigators noted that the thickness of the superomedial angle ranges between 2 and 4 mm whereas the inferomedial angle had a thickness between 5 and 8 mm. Anterior angulation of the superomedial angle also varied between 124° and 162° in the majority of their specimens. In addition, the investigators also identified an anterior “horn-like” projection along the lateral border of at least one scapula. Several researchers have described other osseous abnormalities that may predispose some individuals to painful scapular snapping. These include the superomedial “bare area,” [4] the “Luschka tubercle” (bony protuberance at the superomedial angle) [5], the teres major tubercle (located at the insertion of this muscle) [6], and anterior “hooking” of the superomedial angle [7].
The suprascapular notch is located near the junction of the lateral third of the superior scapular border, just medial to the confluence of the coracoid process with the scapular body [8]. The anatomy of the suprascapular notch is also known to have various morphological features that may predispose some individuals to suprascapular nerve entrapment [9–12]. The transverse scapular ligament travels mediolaterally between the crests of the suprascapular notch. In most cases, the suprascapular nerve is found below the ligament and within the notch whereas the suprascapular artery is found above the ligament and outside of the notch (Fig. 9.2). The transverse scapular ligament is also known to have significant anatomic variations that can also generate symptoms related to suprascapular nerve entrapment [13, 14].
Fig. 9.2
Posterior view of a normal scapula with important neurovascular structures highlighted. The dorsal scapular nerve and artery lie approximately 2 cm medial to the medial scapular border. The suprascapular nerve travels below the transverse scapular ligament whereas the suprascapular artery passes above the ligament.
9.2.2 Muscular Anatomy
The scapulothoracic articulation is unique in that its motion is not dictated by osseous constraints. Rather, the scapula is positioned through the dynamic, coordinated action of surrounding periscapular muscles (see Chap. 3). Therefore, disruption or dysfunction of any one of these muscles can result in scapular malposition or dyskinetic motion which can lead to disordered shoulder function.
9.2.3 Bursal Anatomy
Bursae are fluid-filled sacs lined with synovial-like cells that facilitate gliding of opposing surfaces over one another. In the case of the scapula, there are several periscapular bursae that allow the scapula to glide smoothly over interposed muscle layers. These bursae are commonly defined as either “anatomic” or “adventitial” bursae, depending on their propensity to cause periscapular pain [15]. Anatomic bursae are typically thought to represent normal, physiologic bursae that allow smooth gliding over the posterior thorax. The infraserratus and supraserratus bursae lie on either side of the serratus anterior muscle along the medial scapular border and are the most frequently recognized anatomic bursae [15, 16]. Adventitial bursae are most often located at the superomedial or inferomedial scapular angles and are thought to be significant pathological pain generators [17, 18]. Some researchers have suggested that pain near the superomedial angle can be due to pathologic infraserratus or supraserratus bursal tissue [19, 20], pain near the inferomedial angle is most likely the result of pathologic infraserratus bursal tissue [21, 22], and pain near the confluence of the scapular spine may be caused by a pathologic scapulotrapezial bursa which is most commonly located deep to the trapezius and superficial to the scapular spine (Fig. 9.3) [23].
Fig. 9.3
Illustrations demonstrating the positions of the pertinent periscapular bursae. (a) Positions of the periscapular bursae relative to the scapular body. (b) Axial view showing the positions of the periscapular bursae relative to the surrounding musculature from [23].
9.2.4 Neurovascular Anatomy
Knowledge of pertinent neurovascular anatomy around the scapula is necessary to fully evaluate any patient with a condition related to disordered shoulder motion (see Chap. 3). The spinal accessory nerve, which innervates the levator scapulae muscle, travels with the transverse cervical artery along the levator scapulae muscle which is situated deep to the trapezius muscle. In some cases, the spinal accessory nerve may penetrate through the central portion of the levator scapulae [24]. As the transverse cervical artery travels distally, it becomes the dorsal scapular artery which, in turn, travels with the dorsal scapular nerve beneath the rhomboid musculature a few fingerbreadths medial to the medial scapular border (see Fig. 9.2) [25]. The long thoracic nerve is relatively protected as it travels along the anterior aspect of the serratus anterior muscle. The suprascapular nerve arises from the superior trunk of the brachial plexus and courses towards the suprascapular notch with the suprascapular artery. As mentioned above, the suprascapular nerve passes beneath the transverse scapular ligament whereas the suprascapular artery travels above the ligament (see Fig. 9.2).
9.2.5 Biomechanics
With respect to normal shoulder kinematics, the scapula has several important functions that should be considered before evaluating any patient with a complaint related to the shoulder. First, the scapula provides a stable fulcrum against which glenohumeral motion can occur through the dynamic action of the periscapular musculature, including the rotator cuff and deltoid muscles. In fact, several authors have shown that external stabilization of the scapula may improve the contraction strength of the rotator cuff [26, 27]. Smith et al. [27] found that stabilizing the scapula in a position of retraction substantially increased external rotation strength in 20 normal subjects when compared to external rotation strength with the scapula protracted. Similarly, in a series of 20 patients with shoulder pain (but without rotator cuff tears) and ten healthy controls, Kibler et al. [26] demonstrated a 13–24 % increase in supraspinatus strength when the “empty can” test was performed with the scapulae in a retracted position (see Chap. 4 for details regarding Jobe’s “empty can” test). In 29 overhead athletes with scapular dyskinesis, Merolla et al. [28] measured significantly increased contraction forces of both the supraspinatus and the infraspinatus muscles following the completion of specially designed rehabilitation protocols designed to improve periscapular muscle balance. The same group published similar results in a series of volleyball players who also demonstrated scapular dyskinesis upon initial presentation [29]. Second, accurate positioning of the scapula through coordinated muscle contractions facilitates glenohumeral articular congruency by maintaining alignment of opposing force couples, thus preserving the so-called concavity compression mechanism of dynamic stability (concavity compression is discussed more thoroughly in Chaps. 4 and 6). Third, the scapula plays an important role in the transmission of force through the kinetic chain. In short, the scapula facilitates the transfer of kinetic and potential energy from the largest muscles of the core and trunk towards site of action [30]. Dynamic scapular stability, which is facilitated by adequate core and trunk strength, is necessary to optimize the efficiency of this complex system [31]. Perhaps one of the most well-known examples of this concept is the classic pitching motion most often utilized to deliver a high-velocity pitch in baseball.
9.3 Scapular Dyskinesis
Although most established sports medicine clinicians (both generalists and upper extremity sub-specialists) evaluate and treat patients with some form of scapular dyskinesis on a regular basis, the disorder is still an understudied, underappreciated, and often overlooked category of shoulder dysfunction, especially in novice examiners. The knowledge deficiency in this area may be caused by the relatively infrequent need for surgical intervention, by the lack of sufficient education on the topic or, perhaps, by generational differences in examination and treatment philosophies (such as the gradual transition from primarily experience-based practice to primarily evidence-based practice). In addition to these potential challenges, the precise cause of the condition is often unknown, the risk for secondary injury is often unknown and its effect on shoulder mechanics is probably very complex. In most cases, we prefer to view this problem as a manifestation of some underlying condition rather than an isolated disorder, regardless of whether the pathology is academically defined as “primary” or “secondary” (described below), since appropriate treatment of the underlying condition (ranging from a specific physical therapy protocol to surgical excision of a space-occupying mass) typically resolves the issue altogether. Once scapular dyskinesis has been detected by the initial screening examination, the remainder of the patient encounter should focus on the evaluation and treatment of its potential causes and effects.
9.3.1 Possible Etiologies of Scapular Dyskinesis
There are numerous potential etiologies responsible for the development of scapular dyskinesis, most of which can be divided into primary and secondary causes.
9.3.1.1 Primary Causes of Scapular Dyskinesis
Primary causes of scapular dyskinesis are most commonly related to mechanical or neurogenic defects. Mechanical problems may be associated with a decrease in the scapulothoracic space, such as kyphoscoliosis, rib fracture callus or hypertrophic nonunion, shortened clavicle as a result of fracture malunion and enlarging soft-tissue or skeletal masses, among several other potential defects, can produce symptoms such as scapulothoracic crepitation with shoulder motion (caused by any abnormality that results in a decreased scapulothoracic space) or clinical findings such as the gradual appearance of scapular malposition (caused by the presence of an enlarging mass within the scapulothoracic space which can push the scapular body away from the posterior thorax, thus producing the appearance of scapular winging and dyskinesis). In addition to disordered scapular motion, many of these mechanical issues manifest as periscapular bursitis, crepitus, or so-called scapular “snapping” and are discussed later in this chapter (see the Sect. 9.3.3.7 below).
9.3.1.2 Secondary Causes of Scapular Dyskinesis
Many patients with shoulder pain develop compensatory periscapular muscle contraction (or relaxation) that functions to limit the pain associated with shoulder motion. This abnormal firing pattern produces disordered scapular motion that, in some cases, may exacerbate the inciting injury. In at least one study, the amplitude of activation and the contraction strength of the serratus anterior muscle was significantly decreased in patients with subacromial impingement. This produced an abnormal scapular resting position (increased anterior tilt and downward rotation) and subsequent scapular dyskinesis due to the unbalanced opposing force couple between the serratus anterior muscle (weaker muscle) and the trapezius muscle (stronger muscle). Other potential etiologies of scapular dyskinesis include AC joint instability and/or degenerative osteoarthritis, some forms of glenohumeral instability and neurogenic causes such as cervical radiculopathy and the oft-cited palsies involving the long thoracic nerve (results in prominence of the medial scapular border) and the spinal accessory nerve (results in more subtle scapular winging with difficulty in abduction) (Fig. 9.4).
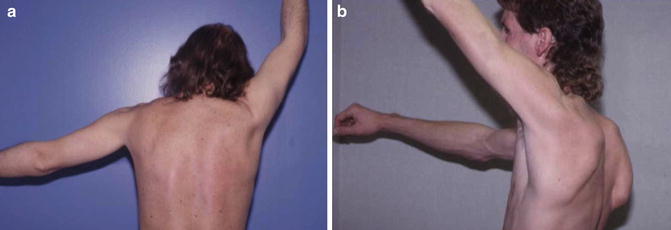
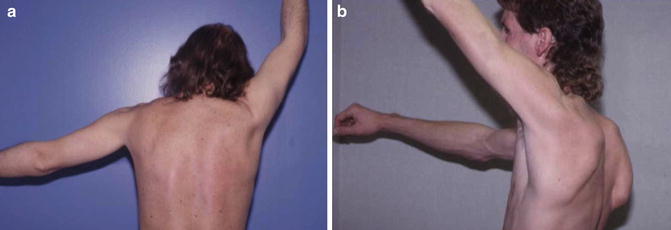
Fig. 9.4
(a) Scapular winging due to trapezius muscle weakness. (b) Scapular winging due to serratus anterior muscle weakness.
Currently, most forms of scapular dyskinesis are attributed to underlying defects related to soft-tissue structures around the shoulder. For example, many overhead athletes display physical evidence of a glenohumeral internal rotation deficit (GIRD) which generally is not considered pathologic unless there is an associated range of motion loss relative to the total arc of motion (Fig. 9.5). However, posterior capsular contractures are often found in these same athletes due to repeated throwing [32]. These contractures essentially “stiffen” the posterior capsule such that glenohumeral adduction and internal rotation causes the scapula to internally rotate (or “windup”) without input from the periscapular musculature [1]. In this example, the scapula can no longer be placed in a position of maximal glenohumeral contact when the arm is adducted and internally rotated, potentially leading to subsequent injuries if not clinically addressed (often related to the SICK scapula syndrome). Other common findings in patients (most commonly athletes) with scapular dyskinesis are tightness of the short head of the biceps tendon and the pectoralis minor tendon [33]. Because each of their tendons forms an attachment to the coracoid process, tightness of either muscle (or both) can result in scapular malposition and disordered scapular motion.
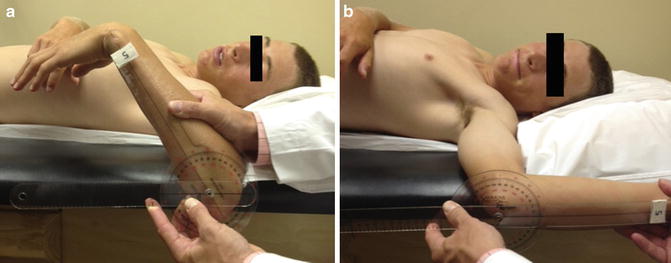
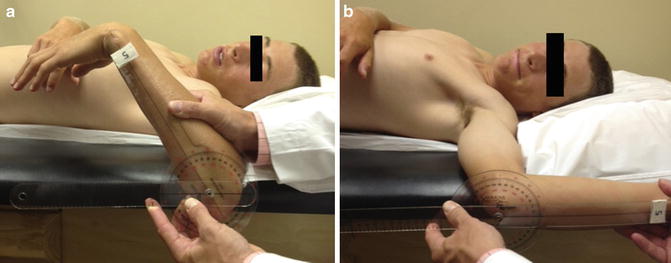
Fig. 9.5
Clinical photographs showing a patient with GIRD. (a) Measurement of passive internal rotation with a goniometer revealed decreased internal rotation capacity. (b) Measurement of passive external rotation with a goniometer revealed increased external rotation capacity. Because the total arc of motion was decreased, the loss of internal rotation was deemed pathologic (Courtesy of Craig Morgan, MD).
Overall, many of the above-mentioned etiologies (except for the specific nerve palsies) result in the same general pattern of scapular malposition and dyskinesis—that is, a protracted resting position and further protraction with arm motion. This is the most common manifestation of scapular dyskinesis which can lead to subacromial impingement (due to a decreased volume within the subacromial space), diminished rotator cuff contraction strength (due to alterations in the length-force relationship of each muscle [discussed in Chap. 3]) [26–28], and chronic overuse injuries such as symptomatic internal impingement in throwing athletes (due to repeated supraphysiologic scapulohumeral angulation) and superior labral anterior to posterior (SLAP) tears (due to the “peel back” mechanism proposed by Burkhart et al. [34] [discussed in Chap. 6] and/or repeated maximal tension placed on the anterior capsule). These common secondary effects, which are often at least partially attributed to scapular dyskinesis, can also lead to tertiary pathologies, thus initiating a so-called vicious cycle. The most commonly encountered cascade of events occurs in the following sequence: (1) primary or secondary dyskinesis, which leads to (2) submaximal supraspinatus contraction, which leads to (3) gradual superior humeral head migration, which leads to (4) a gradual decrease in subacromial space, which leads to (5) subacromial impingement and supraspinatus tears, which lead to (6) pain, which leads to (7) compensatory, asymmetric muscle firing patterns, which lead to (8) worsening of scapular malposition, dyskinesis, superior humeral head migration, and so on.
Regardless of the precise cause, recognition and correct interpretation of disordered scapular motion is an extremely important part of the clinical examination that should never be overlooked in any patient who presents with a shoulder complaint. It is important to remember that the scapula also plays an important role in force transmission through the kinetic chain. Therefore, in most athletic (i.e., non-sedentary) individuals with secondary scapular dyskinesis, a thorough, yet efficient assessment of scapular motion can be considered a reflection of muscular symmetry and the overall health of the kinetic chain.
9.3.2 Physical Examination
Scapular dyskinesis is usually diagnosed by simple palpation of the relevant scapular landmarks while also observing both scapulae during movement of the shoulder through the various motion planes. The condition is most often characterized by prominence of the inferomedial angle and the medial scapular border (as a result of protraction in the resting position), early upward rotation of the scapula during arm elevation and/or early downward rotation of the scapula when lowering the arm back to the side (variations in dyskinetic patterns are described below for specific conditions). Recent evidence suggests that increased upward rotation may be associated with symptom compensation whereas increased downward rotation may be associated with symptom causation. Regardless, any abnormal scapular motion can compromise normal shoulder function by reducing glenohumeral articular congruency, reducing the acromiohumeral distance, increasing tension and strain across the AC joint capsule, decreasing the strength of rotator cuff contraction (which can also reduce glenohumeral stability) and shifting the arc of glenohumeral motion as which commonly occurs in overhead athletes. In addition to these changes, scapular dyskinesis can also mask or enhance the symptoms related to other concomitant shoulder pathologies, such as rotator cuff tears and labral tears, thus complicating the physical diagnosis and subsequent treatment decisions.
Clinical examination of the scapulae should begin with an assessment of posture and symmetry. In many overhead athletes, the dominant shoulder will appear to rest in a slightly lower, or depressed, position relative to the contralateral shoulder (Fig. 9.6). This abnormality often occurs in conjunction with SICK scapula syndrome (scapular malposition, inferomedial angle prominence, coracoid pain, and scapular dyskinesis) which can often be corrected by a focused rehabilitation program. As necessary components of scapular motion, AC and SC joints should also be evaluated for any evidence of pain and/or instability (see Chaps. 7 and 8 for details regarding the AC and SC joints, respectively). The clavicle should also be palpated to confirm adequate length and to identify any abnormal angulation or malrotation.


Fig. 9.6
Clinical photograph of right-handed overhead throwing athlete with a depressed right shoulder (Courtesy of Craig Morgan, MD).
In most cases, the clinician can identify dyskinetic scapular motion by simple observation, palpation and compression of the medial scapular border as the patient elevates and lowers the affected arm (forward flexion, horizontal abduction, and scaption). Specifically, the appearance of a visible prominence of the medial scapular border with any of these motions can be considered dyskinetic motion (Fig. 9.7) [35]. Weights (e.g., 3 or 5 pounds) can also be used to increase the visibility of medial border prominence with shoulder motion (also known as the scapular dyskinesis test). Similarly, resisted external rotation can also produce same pattern of scapular dyskinesis as that which is observed during humeral elevation (i.e., a positive “flip test”; Fig. 9.8). Pain with compression of the scapular body against the thoracic wall with shoulder motion may also be an indicator of snapping scapula syndrome.



Fig. 9.7
Clinical photograph of a patient performing a wall push-up (also discussed in Chap. 3). Note the prominence of the medial scapular border of the left shoulder, a common finding in patients with scapular dyskinesis.

Fig. 9.8
Flip test. Resisted external rotation can often elicit signs of scapular dyskinesis when the examiner is positioned behind the patient in order to visualize both scapulae from posteriorly.
9.3.2.1 Lateral Scapular Slide Test
The lateral scapular slide test was originally developed by Kibler [36] in 1991 as a method to detect asymmetric scapular resting positions with the arms in various degrees of abduction. According to the original description, the distance from the inferomedial scapular angle to the corresponding spinous process along the same horizontal plane was measured bilaterally with both arms (1) at the side, (2) abducted to approximately 30° and slightly internally rotated (i.e., hands on hips), and (3) abducted to 90° in the coronal plane (Fig. 9.9). Kibler [36] suggested that the latter two testing positions required substantial muscular activation involving the upper and lower trapezius and the serratus anterior muscle—weakness of any of these muscles would therefore produce increased lateral deviation of the scapular body. Thus, a difference in bilateral measurements in any of the three testing positions was considered a positive test. Kibler [37] more recently proposed that this cut-off point be increased to 1.5 cm based on experiences within clinical practice combined with other unpublished work involving scapular malposition. However, a study by Odom et al. [38] found no improvement in sensitivity or specificity for the detection of scapular dyskinesis with any of the three testing positions or when the threshold for diagnosis was increased from 1.0 to 1.5 cm. Another study by Shadmehr et al. [39] found that the test was unreliable. However, it should be noted that any study that evaluates the accuracy of a physical examination test for the detection of a specific pathology or defect, the findings on examination should always be coupled with the findings obtained from the diagnostic gold standard. In the case of scapular dyskinesis, there currently does not exist a diagnostic gold standard and, thus, inhibits study interpretation.
Fig. 9.9
Lateral scapular slide test. (a) This test is meant to identify a difference in the medial-lateral positioning of the scapula relative to the thoracic spine. (b) With the patient standing and their arms at the side, the examiner uses measuring tape to measure the distance between the inferomedial scapular angle and the midline, typically marked by the spinous processes (be wary of patients with abnormal spinal curvature, such as those with scoliosis). The measurement is repeated for the contralateral scapula. (c) The measurement is repeated with the hands on the iliac crests and/or with the arms abducted.
9.3.2.2 Scapular Assistance Test
The scapular assistance test was first described by Kibler et al. [26] in 2006 and is typically used to assess the effect of scapular malposition on rotator cuff impingement. In this test, the examiner applies an anterior and superior force to the inferomedial scapular angle to assist upward rotation and posterior tilt of the scapula while the patient flexes and/or abducts the arm (Fig. 9.10). A positive test occurs when the patient reports relief of impingement-like symptoms as the scapula of the affected extremity is manipulated. Acceptable inter-rater reliability has been reported when the test was performed during elevation in either the scapular plane (scaption) or the sagittal plane (forward flexion) [40].


Fig. 9.10
Scapular assistance test. With the patient standing, the examiner places on hand over the superior aspect of the involved scapula with the fingers resting on the anterior clavicle. The examiner’s other hand is placed on the inferomedial scapular angle with the fingers pointed towards the lateral thorax. The patient is then asked to slowly abduct the humerus (scapular plane or sagittal plane). During the process of abduction, the examiner facilitates upward rotation of the scapula by pushing upward and laterally on the inferomedial angle. This maneuver encourages increased posterior scapular tilt and may relieve symptoms of rotator cuff impingement during humeral elevation.
9.3.2.3 Scapular Retraction Test
The scapular retraction test, described by Kibler et al. [41] in 2009, is often used in conjunction with the dynamic labral shear test (discussed in Chap. 6) or the Jobe test (discussed in Chap. 4) to evaluate the potential role of scapular dyskinesis on supraspinatus strength and labral injuries. In this maneuver, the scapula is first positioned and stabilized in a fully retracted position. With the scapula in this position, the examiner performs the dynamic labral shear test to evaluate the glenoid labrum followed by the Jobe test to evaluate supraspinatus strength (empty- or full-can position; however, it is advisable to use the full-can position in the setting of a positive scapular assistance test to minimize symptoms of impingement which can decrease strength measurements) (Fig. 9.11). The test is considered positive when the above-described scapular manipulation decreases the symptoms associated with labral injury or rotator cuff impingement. A similar test has been described for the evaluation of infraspinatus strength in overhead athletes with scapular dyskinesis [42].


Fig. 9.11
Scapular retraction test. With the patient standing, the examiner manipulates the involved scapula into a position of full retraction. The patient then actively abducts the arm within the scapular plane while the examiner continues to apply a stabilizing pressure to the scapula. This posterior stabilization is maintained while the examiner performs both the dynamic labral shear test and Jobe test to assess for pathology involving the labrum or the rotator cuff, respectively [109].
9.3.2.4 Scapular Reposition Test
The scapular reposition test was first described in 2008 by Tate et al. [43] as a modification of the scapular retraction test. The investigators aimed to decrease the amount of retraction while also emphasizing increased posterior tilt and external rotation of the scapula. In their study, the Neer sign, Hawkins–Kennedy test, and Jobe’s empty can test (these maneuvers are described in Chap. 4) were performed in 142 collegiate-level asymptomatic athletes. If any of the above-mentioned tests were positive, each maneuver was repeated with the addition of manual scapular repositioning. Manual scapular repositioning was performed by first manually grasping the top of the shoulder with the fingers over the AC joint and the thumb resting along the scapula spine. The examiner’s forearm was then obliquely positioned over the scapular body. The examiner then applied a moderate force to the scapula using both their hand and forearm to encourage increased posterior tilt and external rotation without achieving full retraction (Fig. 9.12). Following scapular manipulation, the Neer sign and Hawkins–Kennedy test were repeated to assess for any change in shoulder symptoms and the Jobe test was repeated to assess for any change in rotator cuff strength. The intra-class correlation coefficients for the evaluation of rotator cuff strength (using Jobe’s empty can test) were above 0.95 when the scapula was in its original resting position and during manual repositioning. No other studies have evaluated the clinical utility of this test.


Fig. 9.12
Scapular reposition test. With the patient standing, the examiner positions their forearm obliquely across the scapular body such that the fingers rest over the anterior shoulder. The patient is then asked to abduct the humerus in the scapular plane. During humeral elevation, the examiner’s elbow is used to push the inferomedial angle anterolaterally while the fingers are used to pull the scapula posteriorly. This posterior stabilization is maintained while the examiner performs the rotator cuff impingement signs [110].
9.3.3 Selected Conditions Associated with Scapular Dyskinesis
As mentioned above, there are many shoulder disorders that may have an association with scapular dyskinesis. However, we have chosen to focus on several of the more common conditions that we believe are closely related to scapular dyskinesis. The purpose of this section is to highlight the most important concepts related to disordered scapular motion that can subsequently be applied to other, less common shoulder pathologies that are not specifically mentioned below.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








