Sauvé-Kapandji Procedure for Distal Radioulnar Joint Arthritis
Robert M. Szabo
DEFINITION
Disorders of the distal radioulnar joint (DRUJ) are a significant source of wrist pain that is typically caused by one or a combination of conditions: instability, impingement, impaction, and inflammatory arthritis.
The etiology of impingement or impaction symptoms referable to this joint includes displaced fractures or malunions of the distal radius, which cause pain during forearm pronation-supination, and tears of the foveal attachment of the triangular fibrocartilage (TFC) complex, which result in DRUJ instability, mechanical symptoms, and pain.
Both Madelung deformity23 and rheumatoid arthritis (RA) can display secondary incongruity of the DRUJ, causing pain and loss of forearm rotation. Radial head fracture treated by resection and subsequent shortening of the radius (Essex-Lopresti lesion) also can result in painful incongruity or instability of the DRUJ.
ANATOMY
The DRUJ is a distal articulation in the biarticulate rotational arrangement of the forearm that allows 1 degree of motion: pronation and supination. The sigmoid notch of the radius is concave, with a 15-mm radius of curvature.
The ulnar head is semicylindrical, with a radius of curvature of 10 mm, and has an articulate convexity of 220 degrees. It is surrounded by the ulnolunate and ulnotriquetral ligaments, which originate from the palmar radioulnar ligament near the ulnar styloid.
The TFC is a fibrocartilaginous disc originating at the junction of the lunate fossa and the sigmoid notch inserting at the base of the ulnar styloid. Its central portion is cartilaginous and avascular and is designed for weight bearing.
The peripheral margins, the dorsal and palmar radioulnar ligaments, are thick lamellar cartilage designed for tensile loading. They are well vascularized from the palmar and dorsal branches of the anterior interosseous artery and from the ulnar artery.
The ulnar styloid acts as a strut on the end of the ulna to stabilize the ulnar soft tissues of the wrist. The sheath of the extensor carpi ulnaris (ECU), the ulnocarpal ligaments, and the TFC attach at the base of the ulnar styloid to the fovea and together are known as the triangular fibrocartilage complex (TFCC).
The radius of curvature of the head of the ulna does not equal that of the sigmoid notch. In the extremes of pronation-supination, less than 10% of the ulnar head may be in contact with the notch. In pronation, the ulnar head translates 2.8 mm dorsally from a neutral position and in supination, the ulnar head translates 5.4 mm volarly from a neutral position.
The stability of the DRUJ comes from the joint surface morphology, the joint capsule, the dorsal and palmar radioulnar ligaments, the interosseous membrane (particularly the distal oblique bundle), and the musculotendinous units that cross the joint, primarily the ECU and pronator quadratus. The pronator quadratus actively stabilizes the joint by coapting the ulnar head in the sigmoid notch in pronation and passively by viscoelastic forces in supination. The ECU is retained over the dorsal distal ulna by a separate fibro-osseous tunnel deep to and separate from the extensor retinaculum, allowing unrestricted rotation of the radius and ulna.18
PATHOGENESIS
Traumatic injury to the wrist can lead to derangement of the DRUJ, which can result in instability and eventually painful degenerative changes.
Distal radial malunions with dorsal or volar subluxations or dislocations of the DRUJ produce secondary rupture, elongation, or functional shortening of the distal radioulnar ligaments. Shortening of the radius due to malunion can result in ulnar impaction against the lunate and incongruity of the DRUJ.
Arthritis of the DRUJ is a common complication of Colles fractures, particularly when fractures involve the sigmoid notch.
Congenital disorders such as Madelung disease as well as traumatic epiphyseal closures of the distal radius can produce marked positive ulnar variance with dorsal dislocation of the DRUJ.
In the rheumatoid wrist, progression of distal radioulnar synovitis typically results in the “caput ulnae syndrome” as described by Backdahl,1 which consists of the following:
Wrist weakness with pain on pronation and supination
Dorsal prominence of the ulnar head
Limitation of pronation and supination
Swelling of the distal radioulnar area
Secondary tendon changes with possible extensor tendon rupture and ECU subluxation1
If allowed to progress without intervention, the carpus will eventually fall in a more ulnarward and palmarward direction, with strength, mobility, and function all suffering.21
A chronically unstable DRUJ without degenerative changes can be treated with various soft tissue reconstructions, depending on the abnormalities and underlying pathology.
As a group, many of these reconstructions fail to restore stability; even if stability is restored, limitation of forearm motion persists.
NATURAL HISTORY
The natural history of DRUJ derangement is painful limitation of forearm rotation, often with additional functional deficits.
When positive ulnar variance exceeds a few millimeters, additional limitations of wrist flexion-extension as well as radial-ulnar deviation movements can occur.
PATIENT HISTORY AND PHYSICAL FINDINGS
Clinical evaluation begins with a detailed and accurate history.
A history of fracture involving the forearm or wrist is clearly important. Patients may recall a specific injury involving damaging forces of torque with axial load applied to the involved wrist and forearm. In the absence of trauma, congenital conditions may also be considered.
The patient’s occupation or hobbies may give insight into the mechanism of injury as well as the most important functional deficits currently experienced by the patient.
A complete medical history is important, including questions about inflammatory arthritis or osteoarthritis.
DRUJ pathology most often causes ulnar-sided wrist pain, diminished grip strength, limited forearm pronation and supination, and limited wrist ulnar deviation.
Pain is exacerbated with activity and increases with resisted rotation of the forearm.
With large ulnar length discrepancy (positive ulnar variance), limited flexion-extension also can be seen.
During the physical examination, the clinician should determine whether loss of forearm rotation is solely due to DRUJ pathology or if there is a concurrent problem at the proximal radioulnar joint or interosseous membrane. Other sources of wrist pain and dysfunction must be ruled out.
The clinician should check for instability or chronic dislocation of the joint, comparing the injured with the uninjured wrist.
The patient’s normal and affected wrist and forearm ranges of motion, both active and passive, should be measured. A rigid end point with loss of motion suggests bony pathology such as fracture malunion, whereas a soft end point with limited motion suggests soft tissue contractures.
The clinician should carefully palpate, ballote, and compress around the DRUJ and compare the findings to the opposite side. Grip strength measurements should be checked bilaterally. The presence of isolated pain on palpation of the fovea should lead the examiner to consider other etiologies such as a TFCC tear or split ulnotriquetral ligament tear.
When evaluating patients with RA, the clinician should try to distinguish the pain and instability of the DRUJ from radiocarpal and midcarpal joint symptoms by careful palpation, ballottement, and compression of areas around the DRUJ, comparing the degree of symptoms elicited by forearm rotation versus wrist flexion-extension.
Examinations to perform include the following:
Piano key test. The test, which isolates DRUJ disorders, is positive if it causes pain and/or crepitus.
Selective anesthetic injections. The test is positive when precise, selective injection of anesthetic into the area eliminates pain and improves function. Injections help to confirm pathologic changes and can be used to distinguish intra-articular from extra-articular lesions.
Ulnocarpal compression test. A positive test reproduces the ulnar-sided wrist pain and grinding by translating force across the TFC. It also isolates pathologic changes in the TFC.
Lunotriquetral (Regan) shuck test. Pain, sometimes with increased joint mobility and grinding, represents a positive test. This test detects and assesses abnormalities or pathologic conditions associated with the lunotriquetral joint.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard neutral rotation posteroanterior (PA), lateral, and ulnar variance radiographs of the wrist should be obtained and compared with the normal side. The clinician should look for evidence of fractures, arthritic changes, bone lesions, and distal ulna position relative to the radius.
Forearm and elbow radiographs are obtained if there is a history of an elbow injury (especially a radial head fracture) or forearm injury.
If ulnocarpal abutment is suspected, a PA radiograph is obtained with the forearm in pronation and the fist clenched. This will increase ulnar variance and potentially reveal ulna impaction.
Computed tomography (CT) is best to evaluate subluxation and articular congruity of the DRUJ.4,18 To assess the distal radioulnar articular surfaces, simultaneous views are obtained of both extremities with the forearms in neutral rotation, full supination, and full pronation.
Magnetic resonance imaging (MRI) with single-injection gadolinium arthrography is a good way to evaluate TFC lesions as well as the integrity of the scapholunate and lunotriquetral interosseous ligaments.
DIFFERENTIAL DIAGNOSIS
ECU tendinitis or subluxation
Flexor carpi ulnaris (FCU) tendinitis
Pisotriquetral arthritis
Lunotriquetral ligament tear
TFCC tear
Acute DRUJ dislocation
Split ulnotriquetral ligament tear
NONOPERATIVE MANAGEMENT
A trial of nonoperative management is helpful for some patients with DRUJ disorders.
Minor strains of the DRUJ capsule or sprains of other ulnarsided wrist ligaments may respond to rest, ice after activity, wrist splints, and oral anti-inflammatory medications.
Easily reducible dislocations of the DRUJ can be treated by immobilization in a rigid splint or cast for 6 weeks.
Inflammation of the ulnar-sided wrist tendons often accompanies DRUJ problems.
Tendinitis should be treated first with stretching exercises, other physical therapy modalities, and sometimes a steroid injection before addressing the DRUJ surgically.
SURGICAL MANAGEMENT
The Sauvé-Kapandji procedure is especially useful for patients with RA. Despite advanced radiographic findings of radiocarpal or midcarpal arthritis, complaints of wrist pain can be relieved in many RA patients by addressing the DRUJ pathology with a Sauvé-Kapandji procedure.
Commonly, resection of the distal end of the ulna, the Darrach procedure, is recommended for patients with RA and ulnar-sided wrist pain. However, the inflammatory changes and deforming forces acting on the hand and wrist in RA tend to cause palmar and ulnar translocation of the wrist and secondary radioulnar impingement resulting in decreased mobility, strength, and function. Removal of the distal ulna exacerbates and accelerates the problem.
The Sauvé-Kapandji procedure is also beneficial in the treatment of DRUJ disorders resulting from trauma.2
In cases of wrist trauma with ulnar-sided ligamentous injury and incompetence, retaining the ulnar head, as is performed with a Sauvé-Kapandji reconstruction, maintains the ulnocarpal buttress and the TFC to allow a more physiologic transmission of load from the hand to the forearm.
The osteotomy made in the ulna in the Sauvé-Kapandji procedure allows as much shortening as is needed to match the level of the radius while retaining supination and pronation.
Other surgical options include hemiresection and interposition arthroplasty, matched resection of the distal part of the ulna, Darrach resection, and more recently prosthetic replacements of either constrained or unconstrained design.2
Preoperative Planning
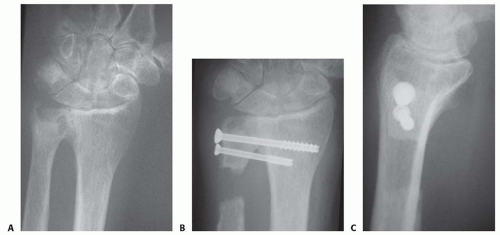
The clinician should review preoperative radiographs carefully for marked positive ulnar variance to assess whether fixation of the ulna head can be performed before the osteotomy or if the osteotomy and excision of ulna segment should be done first to restore proper length and head position into the sigmoid fossa.
Positioning
The patient is positioned supine with the upper extremity on a hand table.
A pneumatic tourniquet is placed on the arm.
An intraoperative fluoroscope is draped sterile and made available throughout the procedure.
TECHNIQUES
▪ Author’s Preferred Technique for the Sauvé-Kapandji Procedure
Incision and Dissection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree