The Use of Free Vascularized Fibular Grafts for Reconstruction of Segmental Bone Defects
Arik Zaretski
Ravit Yanko-Arzi
Yehuda Kollender
Eyal Gur
Jacob Bickels
BACKGROUND
Wide resection of long bone tumors can create a large intercalary bone defect requiring reconstruction. Such defects were traditionally reconstructed with prosthetic implants, allografts, and allograft prosthetic composites, all of which were associated with considerably high rates of complications and failures.5
Distraction osteogenesis provides biologic reconstruction of only small- to medium-sized intercalary defects. Moreover, it is a prolonged procedure, which requires up to 2 months for an elongation of 1 cm, and complications are frequent, patient compliance is critical, and large soft tissue defects cannot be addressed simultaneously.8,12 Reported experience regarding safety and efficacy in the oncologic setup is also limited.
Since the introduction of vascularized autogenous graft for long bone reconstruction after tumor resection in the early 1970s, the use of a free fibular flap has become a viable option for reconstruction of large intercalary bone defects following tumor resection or for the purpose of resection arthrodesis.3,4,6,9,10,11,13,15 Its inherent advantage is based on its ability to exploit the biology of normal fracture healing rather than the creeping substitution that is fundamental to the incorporation of a nonvascularized graft.
The fibula is an optimal vascularized graft source because of its anatomic accessibility and because removing an intercalary segment while preserving the proximal fibula, distal tibial-fibular syndesmosis, and the lateral malleolus would have minimal impact on knee and ankle stability and would not compromise weight-bearing capacity and overall function of the lower extremity. It allows reconstruction of large bone defects because of its independent blood supply, which permits graft incorporation into the host bone even when presence or viability of the surrounding soft tissue are considerably compromised because of previous surgery or radiation therapy.
Furthermore, a vascularized fibular graft has the capability to hypertrophy over time as a response to continuous pressure load. As a result, vascularized fibula have shown excellent long-term durability.2,9,16 The fibular head can also be used for joint reconstruction after intercalary resection of bone tumors.7
In summary, a free fibular graft provides a durable true biologic reconstruction with accommodative and regenerative capabilities associated with minimal short- and long-term complications.16 It requires a combined effort of highly trained and committed teams as well as the patient’s compliance throughout a very long, complex, and demanding rehabilitation period.
APPLIED ANATOMY OF THE FIBULAR FLAP
The fibula is long and narrow and therefore provides a strong cortical strut for reconstruction of long bone defects. It has a square cross-section in its superior part and is triangular in its inferior end. In the adult patient, it can reach a width of 1.5 to 2 cm and a length of 35 cm, 25 to 30 cm of which can be harvested for the purpose of free grafting. Its shape and length can match bone segments of the upper extremity (humerus, radius, and ulna) or fit the medullary canal of bones of the lower extremity (femur, tibia); therefore, it can be used for reconstruction of bone defects at these sites.
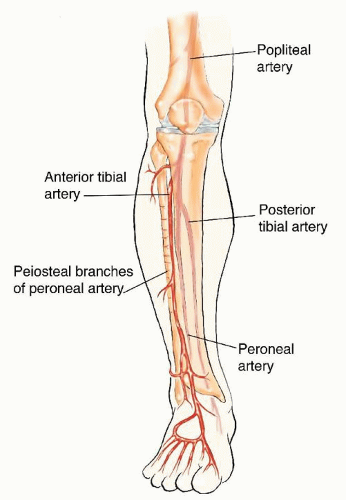
The fibula is circumferentially surrounded by muscle groups on its lateral, anteromedial, and posterior aspects and is also the origin of the four intermuscular septi of the leg. The blood supply and drainage of the fibular shaft are related to the peroneal vessels. The peroneal artery together with the two peroneal venae comitantes follow a course parallel to the fibula and lie between the flexor hallucis longus and tibialis posterior muscles (FIG 1). The fibula is dually vascularized through its endosteal and periosteal vessels.
The endosteal blood supply is based on the nutrient artery, which stems 6 to 14 cm from the peroneal artery bifurcation, enters the middle third of the diaphysis via the nutrient foramen, and then divides into an ascending and a descending branch. The periosteal blood supply is derived from 8 to 9 periosteal branches, mostly in the middle third of the diaphysis. The peroneal artery is also the source of 4 to 6 fascial vessels that pass through the posterior intercrural septum to the skin territory, lateral to the fibula. It provides numerous muscular branches as well; specifically, it supplies multiple small branches to the muscles of the anterior compartment and a few larger branches to the soleus muscle at the deep posterior compartment of the leg.
The unique morphologic characteristics and blood supply of the fibula allow considerable versatility in the use of the fibular flap for reconstruction of skeletal, soft tissue, and growth plate defects, as required. The fibular flap can be transferred in various configurations and compositions to suit the needs of individual cases:
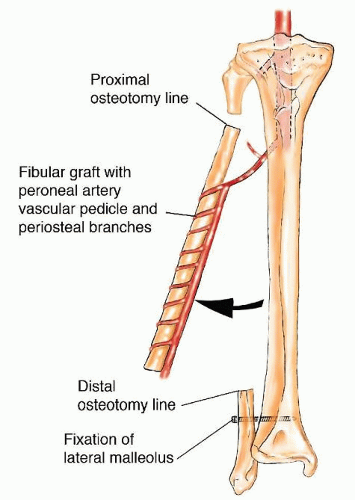
In its straight configuration, it can be used for reconstruction of a relatively narrow bone segment (FIG 2). A longitudinal osteotomy that increases the surface area of the flap can serve as an onlay graft to augment the healing process for partial cortical defects. Based on perforating fasciocutaneous branches at the middle and distal thirds of the pedicle, a skin paddle of up to 20 × 10 cm can be transferred simultaneously to facilitate coverage of concomitant large soft tissue defects and to allow the patency
of the pedicle anastomosis to be monitored. Part of the soleus or the flexor hallucis longus muscles can also be included with the flap to reconstruct soft tissue defects and cover exposed bone.
Transverse osteotomies can be made through the mid-diaphysis to produce two or more cortical struts on a single pedicle (double/triple barrel) for reconstruction of a wide bone segment. In these cases when the endosteal vessels are transected, the bone survives on its periosteal system.
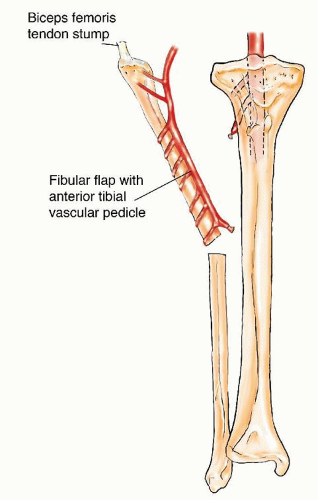
The proximal epiphysis may be included in the flap for joint reconstruction and preservation of longitudinal growth potential (in pediatric patients) after intra-articular resection of bone tumors (FIG 3). This flap is based on the anterior tibial vascular flap or the descending geniculate artery and is most commonly used for reconstructions following resections of the proximal humerus and distal radius.
INDICATIONS
Segmental bone defects larger than 5 cm following resection due to the following:
Tumor
Radiation-induced bone necrosis
Osteomyelitis
In cases of high-grade sarcomas of bone, the authors generally use spacers for immediate reconstruction following tumor resection rather than performing the definitive reconstruction with vascularized fibula. The latter is carried out 2 years after tumor resection if there had been no tumor recurrence or lung metastases.
CONTRAINDICATIONS
Systemic/general conditions
Cardiovascular, surgical, or hematologic diseases that may affect peripheral blood flow
Incompliance with or if patient’s physical or psychological states do not allow to withstand a prolonged non-weight bearing and/or rehabilitation
Poor general health status
Donor site considerations
Fibular deformity following previous injury to the lower extremity
Vascular injury or compromise following previous trauma to the leg
Vascular anomalies of the leg or plantar arches (eg, single-vessel or peroneal vessel-dominant foot)
Recipient site considerations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree