Septic arthritis is defined as an infection within the closed space of a joint.
It is usually acute and purulent secondary to a bacterial infection.
It can cause irreversible damage to articular cartilage and therefore warrants prompt treatment with adequate drainage and an appropriate antibiotic regimen.
Delay in making the diagnosis and initiating treatment can have serious negative implications to the condition of the joint and health of the patient.2
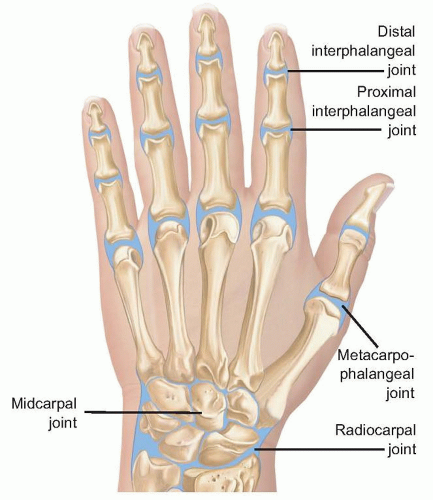
The interphalangeal (IP) and metacarpophalangeal (MP) joints of the hand are hinge joints (FIG 1).
The IP joint space is maximized in slight flexion and the MP joint in extension.
The wrist joint includes the radiocarpal, midcarpal, and radioulnar joints. Septic arthritis may be present in all of these joint spaces, concomitantly or separately, depending on the integrity of the intercarpal ligaments and the triangular fibrocartilage complex (see FIG 1).
Septic arthritis may affect any joint of the hand or wrist.
Septic arthritis does not have a gender or race predilection, but it is more common in adults than in children.
The inoculation of the joint is most likely due to a penetrating injury (ie, lacerations, puncture wounds, and bites). Other causes include hematogenous seeding or contiguous spread.10
At the distal IP joint, septic arthritis is common from penetrating trauma as well as contiguous infection from a mucous cyst, felon, paronychia, or suppurative flexor tenosynovitis.
At the proximal IP joint, contiguous infection is most commonly related to a suppurative flexor tenosynovitis.
At the MP joint, septic arthritis is most common after direct inoculation from a clenched fist injury or fight bite.
Hematogenous spread can result from any concomitant or preceding infection of the body, including oral, upper respiratory, gastrointestinal, and genitourinary infections.
The synovium is highly vascular and contains no limiting basement membrane, promoting easy access of blood contents to the synovial space.3
The presence of bacteria within the joint induces a cellular and immunologic response that is detrimental to the joint. Bacteria rapidly replicate, producing toxins. The presence of bacteria stimulates an immunogenic response, resulting in the arrival of leukocytes, which produce proteolytic enzymes. Both the bacterial toxins and leukocytic enzymes destroy the articular cartilage of the joint by degrading proteoglycans and eventually injuring the underlying chondrocytes.
Any disorder that results in an immunocompromised state can predispose to septic arthritis.
Table 1 Common Risk Factors Predisposing to Septic Arthritis
Local factors
Penetrating joint trauma
Recent joint surgery
Open reduction of intra-articular fractures
Osteoarthritis
Prosthetic joints
Social factors
Newborns
Elderly
Occupational exposure to animals
Low socioeconomic status
Systemic disorders
Rheumatoid arthritis
Diabetes mellitus
Liver diseases, alcoholism
Chronic renal failure, hemodialysis
Malignancies
AIDS
Immunosuppressive medication
IV drug abusers
IV, intravenous.
Table 2 Common Microorganisms Causing Septic Arthritis
Gram-positive aerobes
Staphylococcus aureus
Streptococcus pyogenes
Streptococcus pneumoniae
Gram-negative aerobes
Haemophilus influenzae
Escherichia coli
P. multocida
N. gonorrhoeae
Anaerobes
Eikenella corrodens
Borrelia burgdorferi
Mycobacterial species
Fungus
Sporotrichosis
Cryptococcus
Blastomycosis
Rheumatoid arthritis, in particular, poses a higher risk of infection. This risk is related to a variety of factors including general debilitation, immunosuppressive medication, tumor necrosis factor blockers (eg, infliximab or etanercept), and chronic joint injury.
In patients with rheumatoid arthritis, a diagnosis of septic arthritis may be delayed because of misinterpretation of a rheumatoid flare. A high index of suspicion must be maintained when evaluating for septic arthritis in patients with rheumatoid arthritis.9
Virtually, any microbial pathogen is capable of causing pyogenic septic arthritis (Table 2).
Staphylococcus aureus and Streptococcus species are the most common offending organisms.
Gram-negative, anaerobic, and polymicrobial infections also are possible, especially in intravenous (IV) drug abusers and immunocompromised patients.
Specific bacterial pathogens are related to certain circumstances, for example, Eikenella corrodens in human bite wounds, Pasteurella multocida after domestic animal bites, Neisseria gonorrhoeae infections in sexually active young patients, and fungal and mycobacterial infections in immunocompromised patients.
The combination of the growing bacterial load and the ensuing inflammatory response results in a growing effusion that causes synovial ischemia, pressure necrosis of the cartilage, and infiltration of the bacteria into both the subchondral bone and overlying skin.
Bacterial infiltration out of the joint can result in secondary osteomyelitis, suppurative flexor tenosynovitis, and skin breakdown with spontaneous drainage.
Patients will complain of pain and swelling about the joint.
Systemic signs of joint infection may include fevers, chills, malaise, and tachycardia.
The patient should be asked about a history of penetrating trauma; human, animal, or insect bites; recent joint aspirations; recent infections elsewhere; and the presence of an immunocompromising condition.
On examination, patients will manifest a painful swollen joint, with overlying erythema and warmth.
The most important physical examination finding is exquisite pain with precise joint motion, different from that typically seen when a noninfectious effusion or overlying cellulitis is present.
Use of a regional block for pain relief, often performed by an emergency or primary care physician, will mask the condition and must be discouraged.
Attempted active digital motion will result in significant guarding, and passive flexion and extension should induce exquisite pain.
Physical examination of the wrist often is less dramatic than that of the digits. The joint typically is held in a neutral position.
Active wrist motion also will induce guarding and pain.
Passive flexion will also cause the patient to guard secondary to pain.
Passive pronation and supination may also help determine involvement of the distal radioulnar joint.
Laboratory studies should include white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and blood cultures.
The WBC usually is not elevated, but the ESR and CRP levels are consistently elevated (unless the patient is immunocompromised).
Diagnosis of a septic arthritis is best accomplished by joint aspiration, microscopic analysis, and culture.
If an infection is present, increased fluid turbidity will be noted.
Joint aspirates should be sent for a cell count with differential, Gram stain, crystal analysis, glucose, and cultures (aerobic, anaerobic, fungal, and mycobacterial) (Table 3).
Diagnosis can be made most reliably with a joint fluid WBC count greater than 50,000 (and a differential of 75% or more segmented neutrophils), a Gram stain confirming the presence of bacteria, or positive cultures.5
Table 3 Differential Diagnosis of Synovial Fluid Analysis
Test
Normal
Septic
Inflammatory
Clarity
Transparent
Opaque
Straw
Color
Clear
Yellow-green
Yellow
Viscosity
High
Variable
High
WBC count
<200
>50,000
2000-10,000
PMN (%)
<25
>75
>50
Culture
Negative
Often positive
Negative
Glucose (mg/dL)
Equivalent to plasma
−25 < plasma
−40 < plasma
WBC, white blood cell; PMN, polymorphonuclear leukocyte.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree