Sauve Kapandji Procedure
Robert M. Szabo
Indications
Traumatic injury to the wrist can lead to derangement of the distal radioulnar joint (DRUJ), which can result in instability, painful degenerative changes, and arthritis. A chronically unstable DRUJ without degenerative changes can be treated with various soft tissue reconstructions, depending on the abnormalities. As a group, many of these reconstructions fail to restore stability and, even if stability is restored, limitation of forearm motion persists (1,2,3,4). Distal radial malunions with dorsal or volar subluxations or dislocations of the DRUJ produce secondary rupture, elongation, or functional shortening of the distal radioulnar ligaments. Arthritis of the DRUJ is a common complication of distal radius fractures, particularly when fractures involve the sigmoid notch. Congenital disorders such as Madelung’s disease as well as traumatic epiphyseal closures of the distal radius can produce marked positive ulnar variance with dorsal dislocation of the DRUJ. In the rheumatoid wrist, progression of distal radioulnar synovitis typically results in the caput ulnae syndrome as described by Backdahl, which consists of (a) wrist weakness with pain on pronation and supination; (b) dorsal prominence of the ulnar head; (c) limitation of pronation and supination; (d) swelling of the distal radioulnar area; and (e) secondary tendon changes with possible extensor tendon rupture and extensor carpi ulnaris subluxation (5). If allowed to progress farther without intervention, the carpus will eventually fall in a more ulnarward and palmarward direction, leading to loss of strength, mobility, and function (6).
The consequences of the natural history of DRUJ derangement is painful limitation of forearm rotation with functional deficits. When positive ulnar variance exceeds a few millimeters additional limitations of wrist flexion or extension as well as radial or ulnar deviation movements can occur. Alternative treatment options include hemiresection and interposition arthroplasty, matched resection of the distal part of the ulna, a Darrach resection, and more recently, ulnar metallic prosthetic replacement (7). Retaining the ulnar head, such as with a Sauve-Kapandji reconstruction after wrist trauma with ulnar-sided ligamentous incompetence, maintains the ulnocarpal buttress and the triangular fibrocartilage complex to allow a more physiologic transmission of load from the hand to the forearm. In rheumatoid arthritis, rather than providing a support to prevent ulnarward and palmarward translocation of the carpus, removal of the distal end of the ulna results in a worsening of deformity and increasing dysfunction. And, as the translocation progresses, a worsening of more distal joint problems, such as ulnar drift at the metacarpophalangeal joints. Retention of the distal ulna provides both a bony support and retains the ulnocarpal complex soft tissue attachments as well. The stability at the wrist then helps prevent more distal joint deformity (6). The osteotomy made in the ulna in the Sauve-Kapandji procedure allows as much shortening as is needed to match the level of the radius while retaining supination and pronation.
Contraindications
No absolute contraindications exist to performing a Sauve-Kapandji procedure, but there times alternative options should be explored. I would not recommend considering to use it in children with open physes. When ulnar length is greater than 1 cm or in cases of a multiplanar radius deformity in a younger patient, I would perform a radial osteotomy; if needed, I would perform the Sauve-Kapandji
procedure as a second stage. The procedure should also be used with extreme caution if the interosseous ligament between the radius and ulna is injured such as with an Essex–Lopresti fracture where proximal migration of the radius can be progressive.
procedure as a second stage. The procedure should also be used with extreme caution if the interosseous ligament between the radius and ulna is injured such as with an Essex–Lopresti fracture where proximal migration of the radius can be progressive.
Patients who have dorsal subluxation or dislocation of the ulna preoperatively are at particular risk for having postoperative instability of the ulnar stump (3). Although there is no reliable resolution to this problem, the Sauve-Kapandji procedure can be considered in conjunction with a flexor carpi ulnaris (FCU) or extensor carpi ulnaris (ECU) tenodesis in these cases.
Preoperative Preparation
Clinical evaluation begins with a detailed accurate history. A history of fracture involving the forearm or wrist is clearly important. Patients may recall a specific injury in which forces of torque were applied with axial load applied to the involved wrist and forearm. Those forces may cause damage to the DRUJ resulting in joint instability. The patient’s occupation or hobbies may give insight to a mechanism of injury. Obtain a complete medical history, specifically seeking out inflammatory or osteoarthritis. DRUJ pathology causes wrist pain, weak grip, limited forearm pronation and supination, and sometimes limited wrist ulnar deviation. Pain is exacerbated with activity and increases with resisted rotation of the forearm. With larger ulnar length discrepancy (positive ulnar variance) limited flexion or extension also can be seen.
During the physical examination, determine if loss of forearm rotation is caused by DRUJ pathology or if a problem exists at the proximal radioulnar joint or interosseous membrane. Check for instability and chronic dislocation of the joint. Measure the patient’s normal and affected wrist and forearm ranges of motion, both active and passive. A rigid end point with loss of motion suggests bony pathology (e.g., fracture malunion), whereas a soft end point with limited motion suggests soft tissue contractures. Carefully palpate, ballote, and compress around the DRUJ and compare with the opposite side. Check grip strength measurements bilaterally.
Standard neutral rotation posteroanterior (PA), lateral, and ulnar variance radiographs of the wrist should be obtained and compared with the normal side. Use these views to look for evidence of fractures, arthritic changes, and bone lesions. Forearm radiographs are obtained if there is a history of an elbow injury, especially a radial head fracture, or forearm injury. If ulnocarpal abutment is suspected, obtain a PA radiograph with the forearm in pronation and the fist clenched, which increases ulnar variance. Computed tomography (CT) is best to evaluate subluxation of the distal radioulnar joint (4,8). To accurately assess the congruity of the distal radioulnar articular surfaces, obtain simultaneous views of both extremities with the forearms in neutral rotation, full supination, and full pronation. Magnetic resonance imaging (MRI) with single-injection gadolinium arthrography (MRA) is a good way to evaluate lesions of the triangular fibrocartilage complex as well as the integrity of the scapholunate and lunotriquetral interosseous ligaments. CT and MRI scans and other diagnostic tests are useful in evaluating certain conditions, such as the status of the triangular fibrocartilage complex, but are not needed in most cases before performing the Sauve-Kapandji procedure.
A trial of nonoperative management is helpful for some patients with DRUJ disorders. Minor strains of the DRUJ capsule or sprains of other ulnar-sided wrist ligaments may respond to rest, ice after activity, wrist splints, and oral anti-inflammatory medications. Easily reducible dislocations of the DRUJ can be treated by immobilization in a cast for 6 weeks. Inflammation of the ulnar-sided wrist tendons often accompanies DRUJ problems. Tendonitis should be treated first with stretching exercises, other physical therapy modalities, and sometimes a steroid injection before addressing the DRUJ surgically.
Technique
Position the patient supine with the upper extremity on a hand table.
Place a pneumatic tourniquet on the arm.
An intraoperative fluoroscope is draped sterile and made available throughout the procedure.
Make a straight longitudinal incision, 6 to 8 cm long, along the ulnar border of the distal forearm.
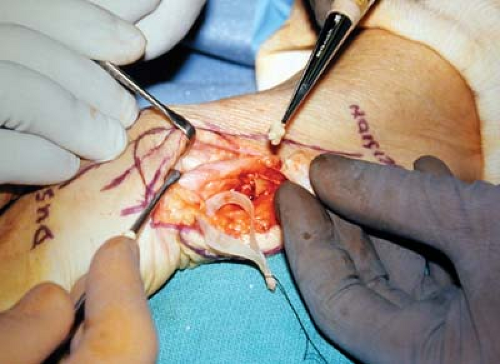
Identify the dorsal cutaneous branch of the ulnar and protect it throughout the case (Fig. 35-1). An alternative incision may be used if additional procedures are planned at the same sitting. For example, in patients with rheumatoid arthritis, often there is a need to combine the Sauve-Kapandji
procedure with another soft tissue procedure, such as a dorsal wrist synovectomy, tenosynovectomy, or tendon transfer, to treat extensor tendon ruptures that result from the caput ulnae syndrome. In that case, start the incision more dorsally to facilitate exposure for the additional procedure, and then extend it proximally and obliquely to expose the distal ulna (9).

Figure 35-1 Identification and mobilization of the dorsal sensory ulnar nerve, which is tagged with a rubber dam. Notice a dorsal branch under the probe.

Figure 35-2 Measure the osteotomy resection. As shown here, take into consideration the amount of shortening needed to obtain neutral ulna variance.
Expose the distal 4 to 6 cm of the ulna extraperiosteally through the interval between the ECU and FCU.
Select the appropriate level for an osteotomy of the ulnar diaphysis (Fig. 35-2).
Cut the bone just proximal to the flare of the ulnar head, which will leave sufficient distal ulna to accommodate two fixation screws.
With fluoroscopy, confirm that the proposed osteotomy site is appropriate.
Make a second cut proximal and parallel to the first (Fig. 35-3) and remove a 10- to 14-mm segment of ulna (Fig. 35-4).
Save the removed bone for subsequent grafting into the DRUJ arthrodesis site (Fig. 35-5).
Next, expose the distal radioulnar joint by way of a dorsoulnar capsulotomy just radial to the ECU tendon.
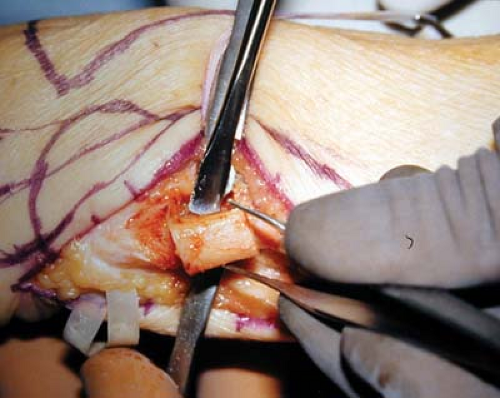
Figure 35-4 Removal of the resected ulna. Preserve the pronator quadratus, which is left behind for later use.
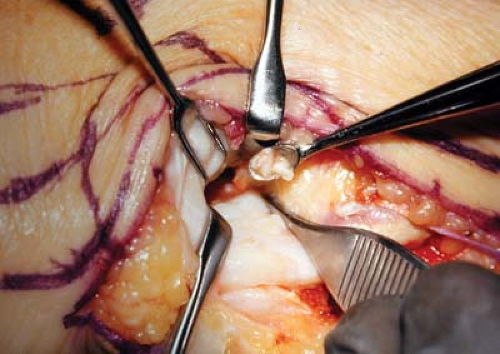
Figure 35-6 Curette the sigmoid notch of any remaining cartilage and then pack in the bone graft from the resected ulna.
Denude both the ulnar head and sigmoid fossa of the radius of all remaining cartilage to create flush surfaces of cancellous bone on each side of the arthrodesis site and pack the harvested cancellous bone from the removed ulna segment (Fig. 35-6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree